Duodenum, Duodenum Anatomy, DUODENUM functions, DUODENUM Conditions, DUODENUM disorders, DUODENUM Diganosis
Duodenum- Anatomy, Functions and Conditions
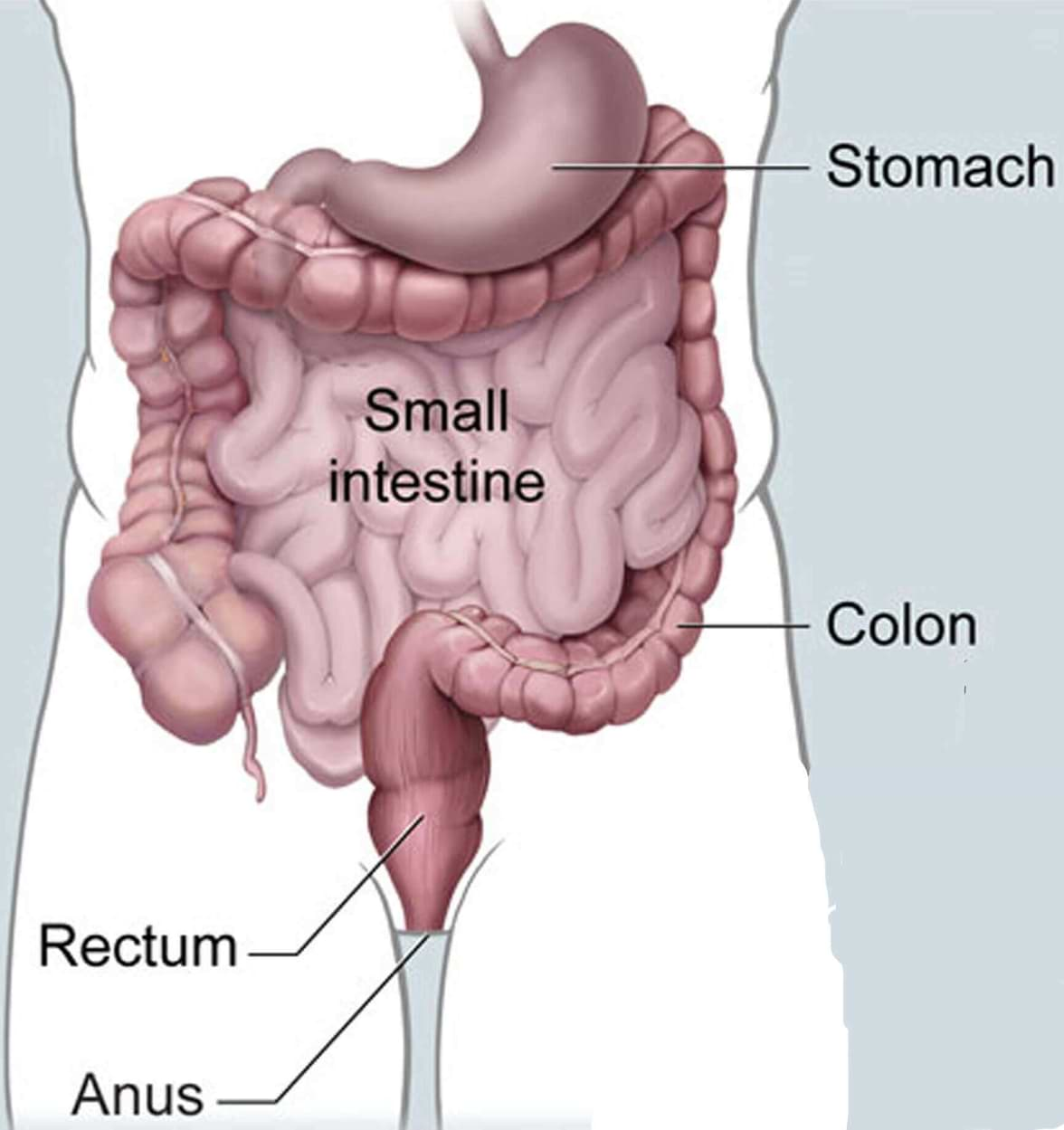
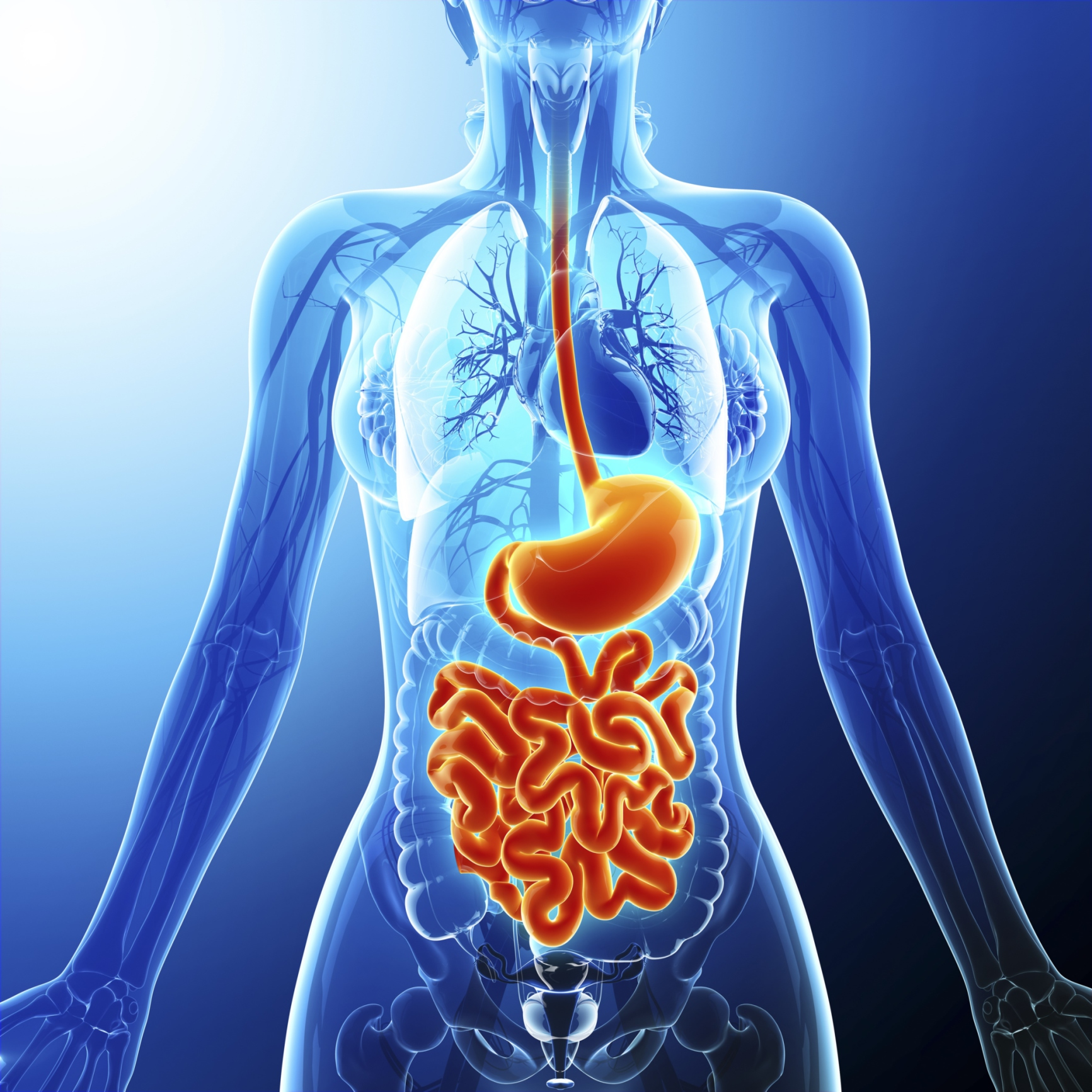
The duodenum is the first and shortest of three sections that make up the small intestine, including the jejunum and ileum. At 8 to 10 inches long, it is a key organ in the gastrointestinal (GI) system, working to digest nutrients and make them available for absorption into the bloodstream.
Overview
Just as the esophagus connects to the stomach so that food can enter it, the duodenum is connected to the stomach so that food can leave it and begin its course through the intestines.
In this article you will learn about the anatomy and function of the duodenum in the digestive system of the body. Also, you will learn about conditions that may affect the duodenum, as well as their diagnosis and treatment.
Duodenum Anatomy
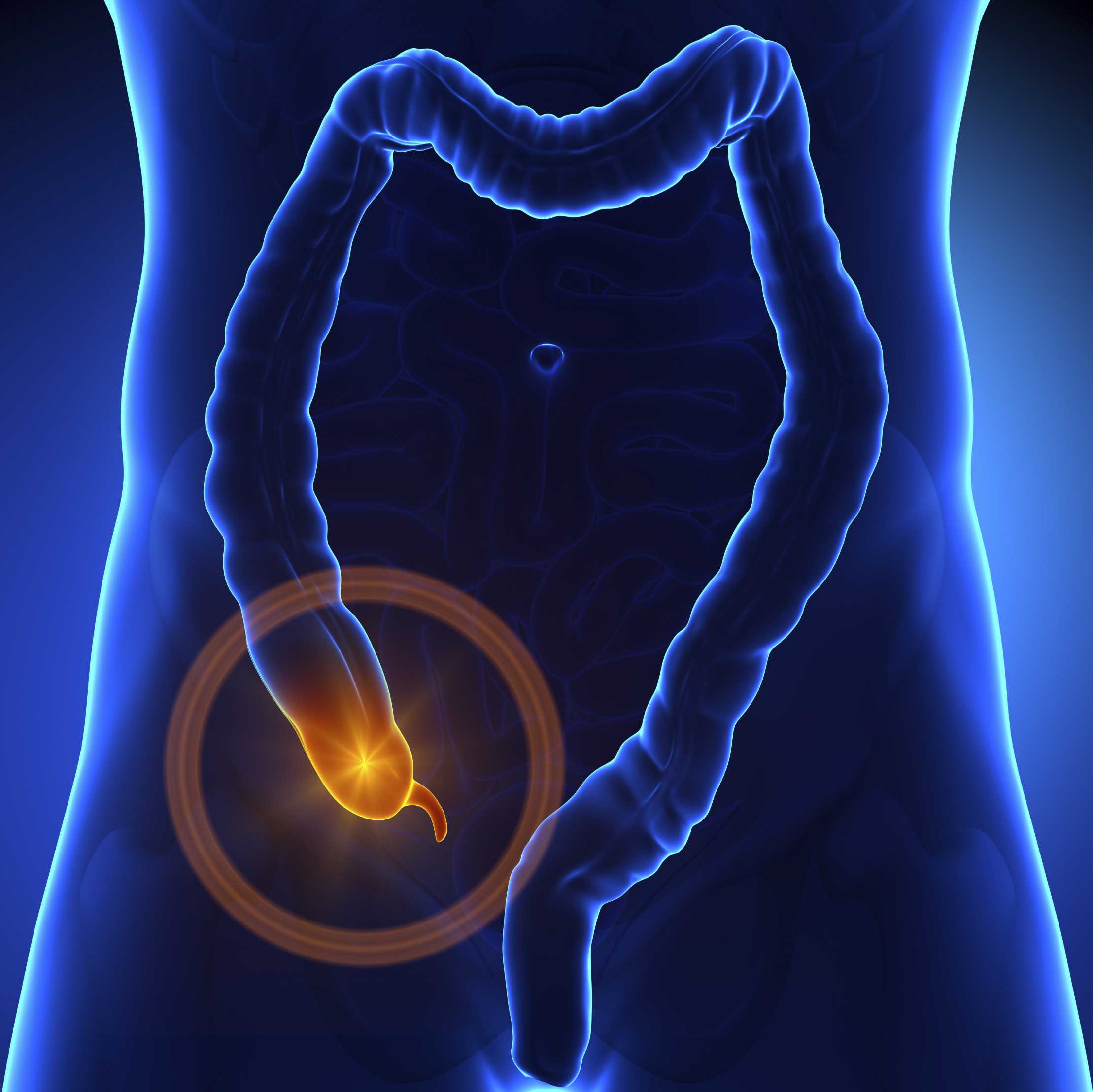
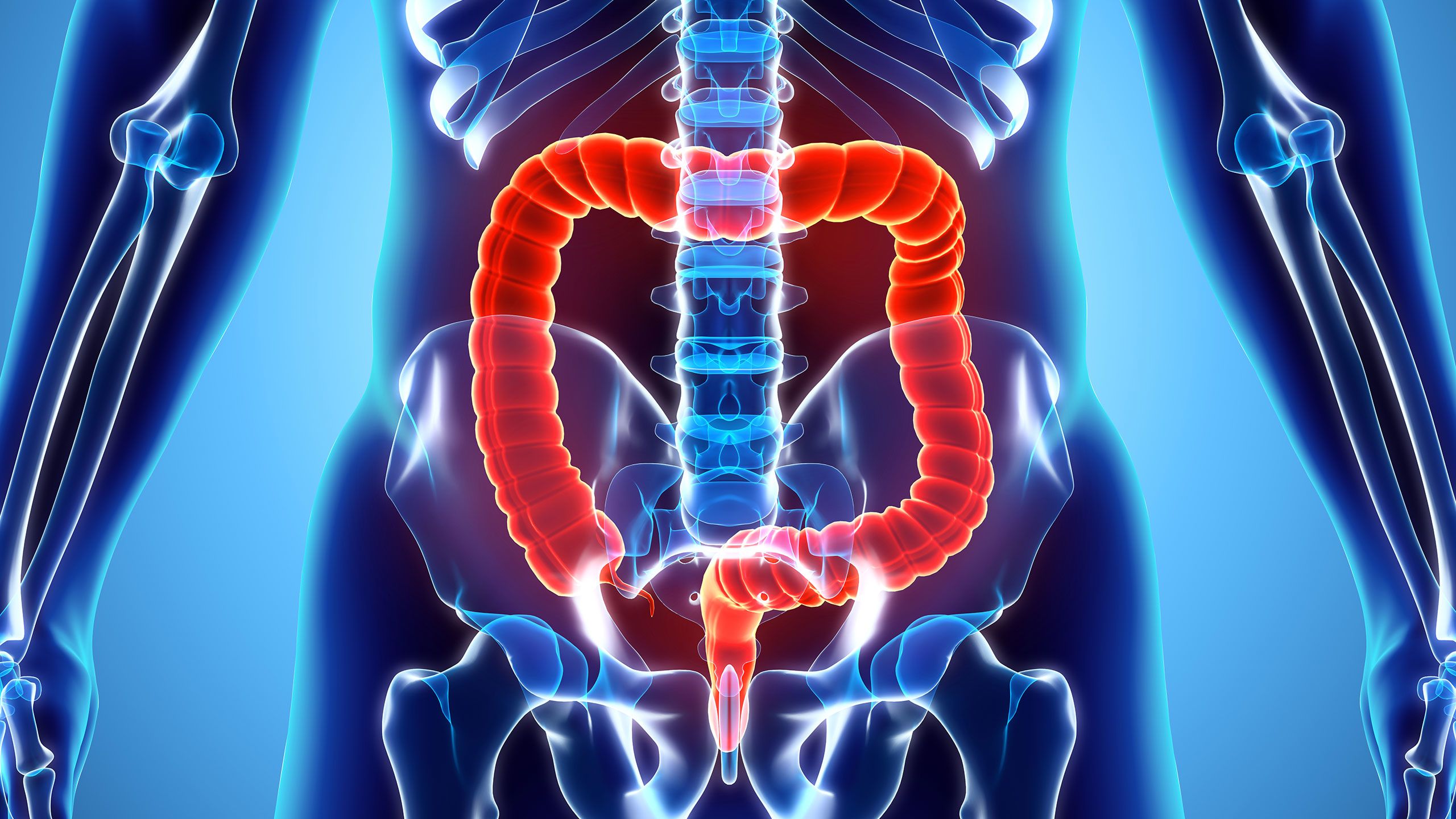
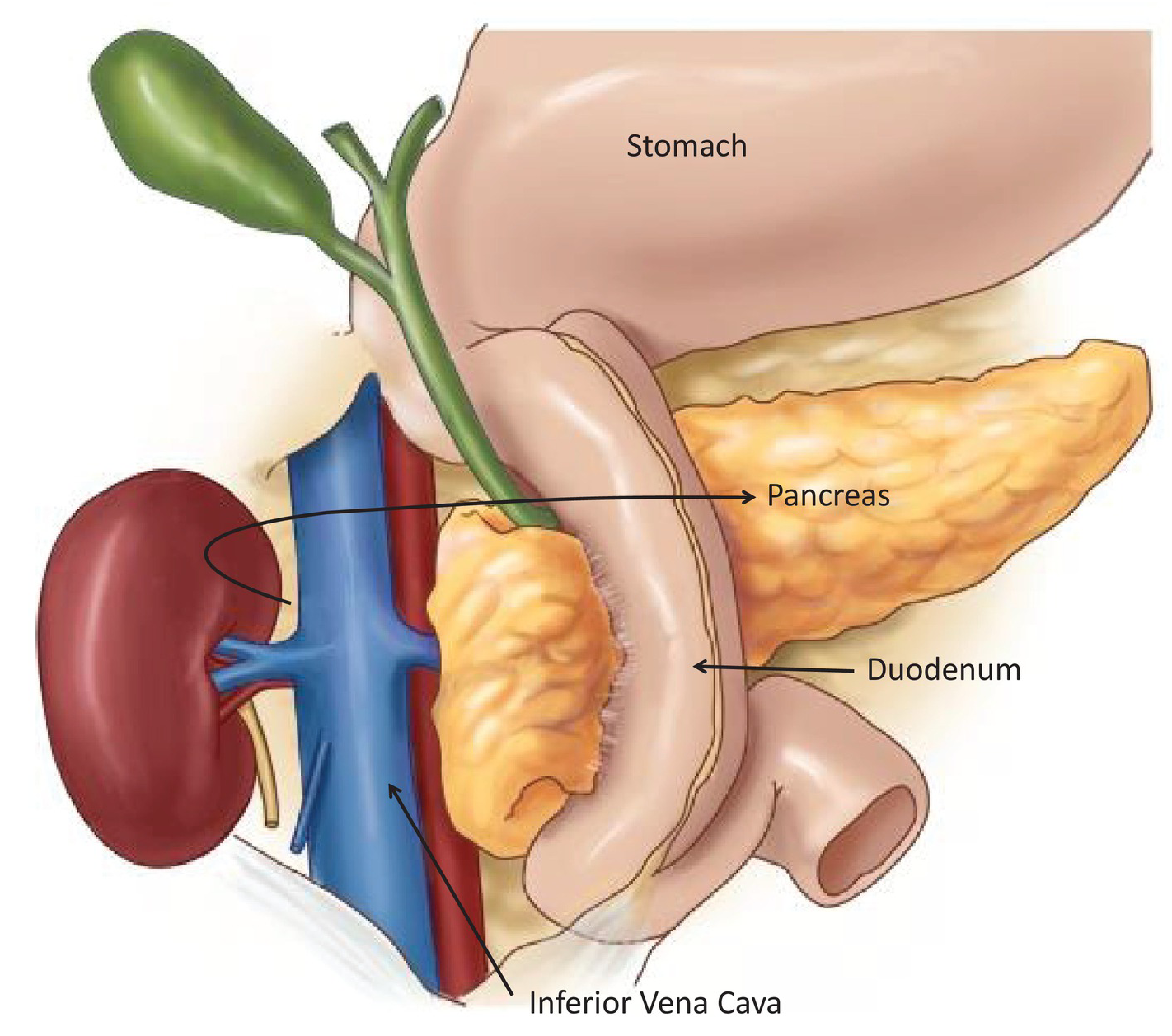
The duodenum has been described as a C-shaped or horseshoe-shaped segment of the small intestine. It is located below the stomach.
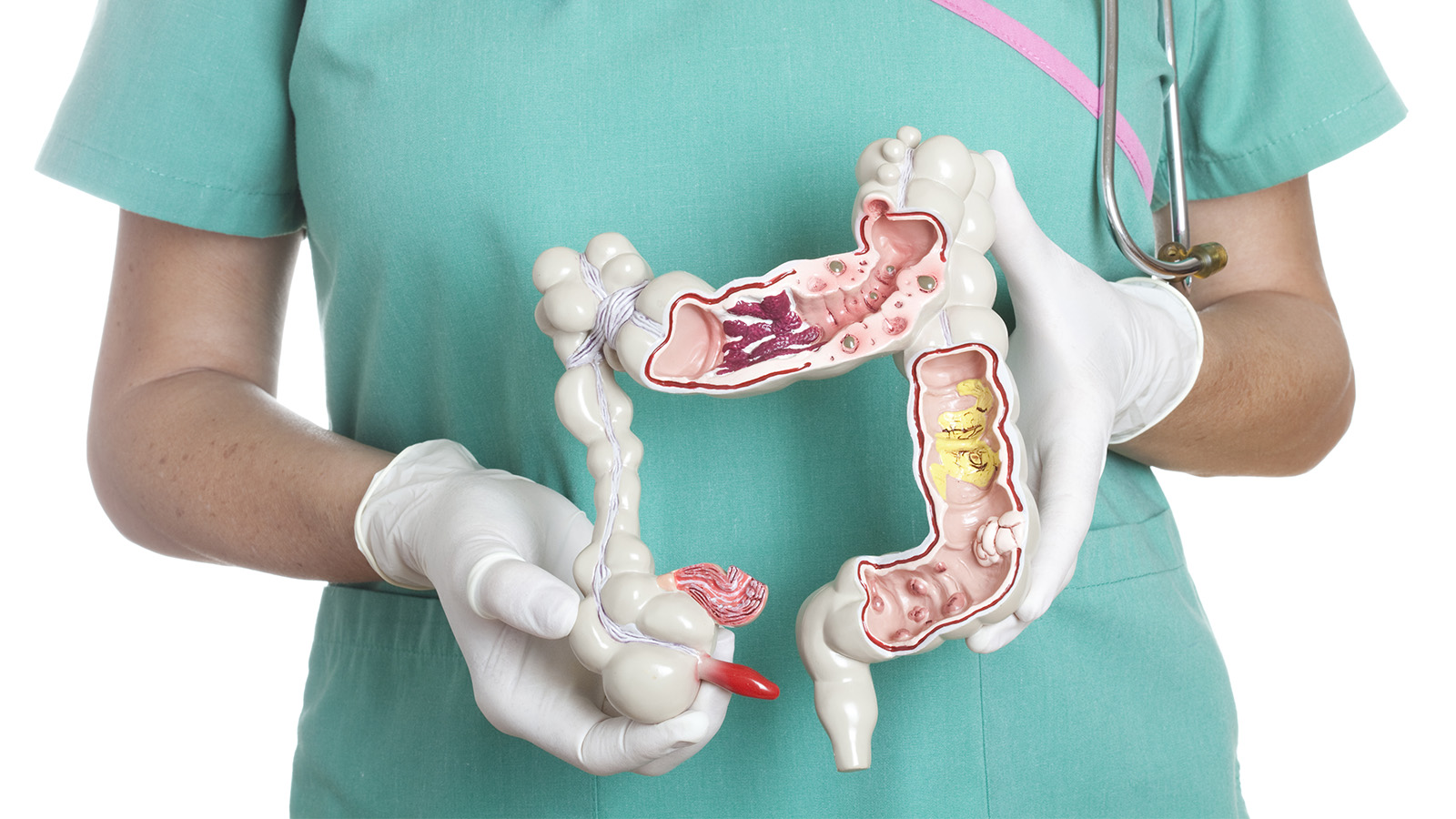
The duodenum can be separated into four segments. Each segment has a different anatomy (shape) and performs a different function. The lining of the duodenum is composed of four layers, each with its own specialized function.
Duodenum Structure
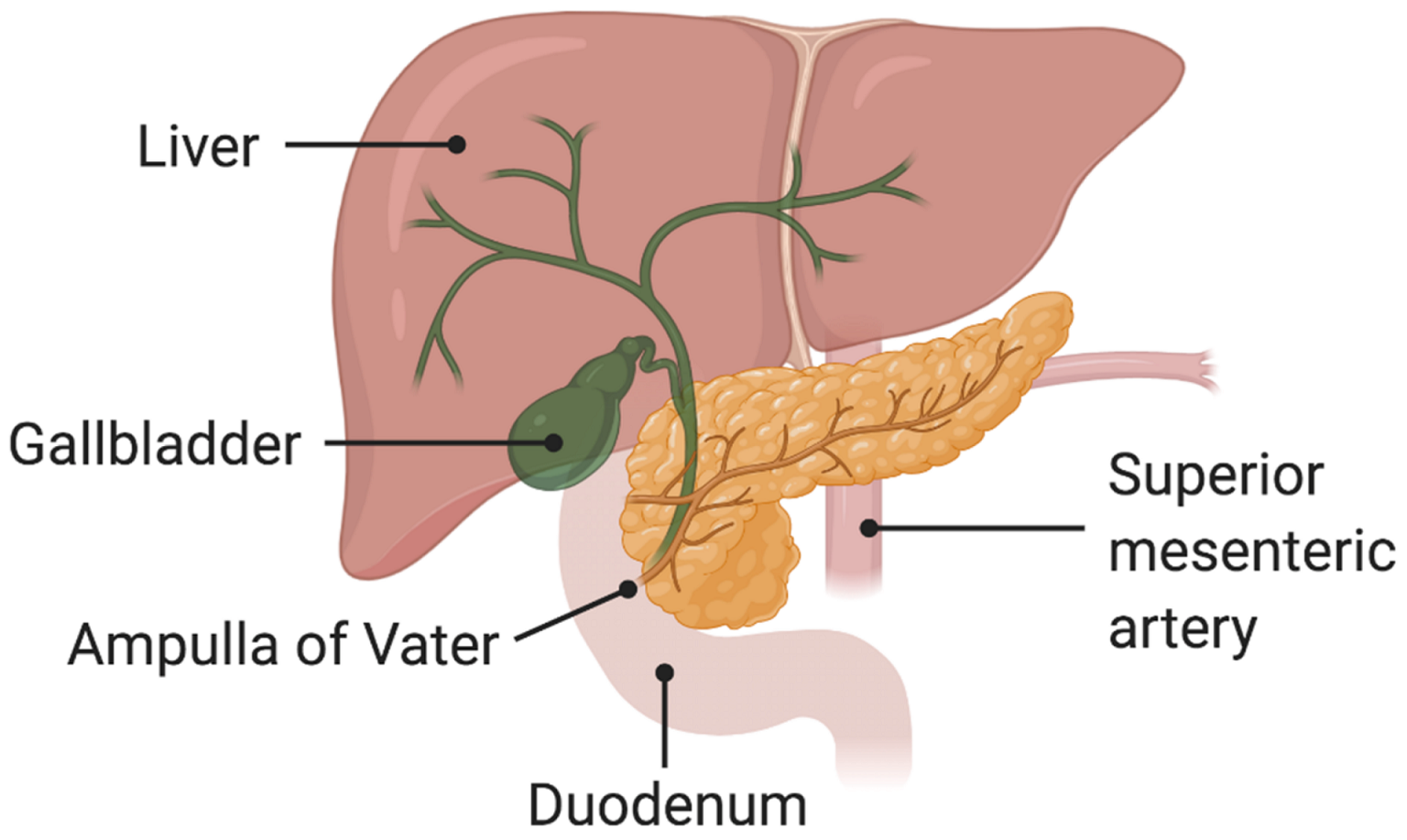
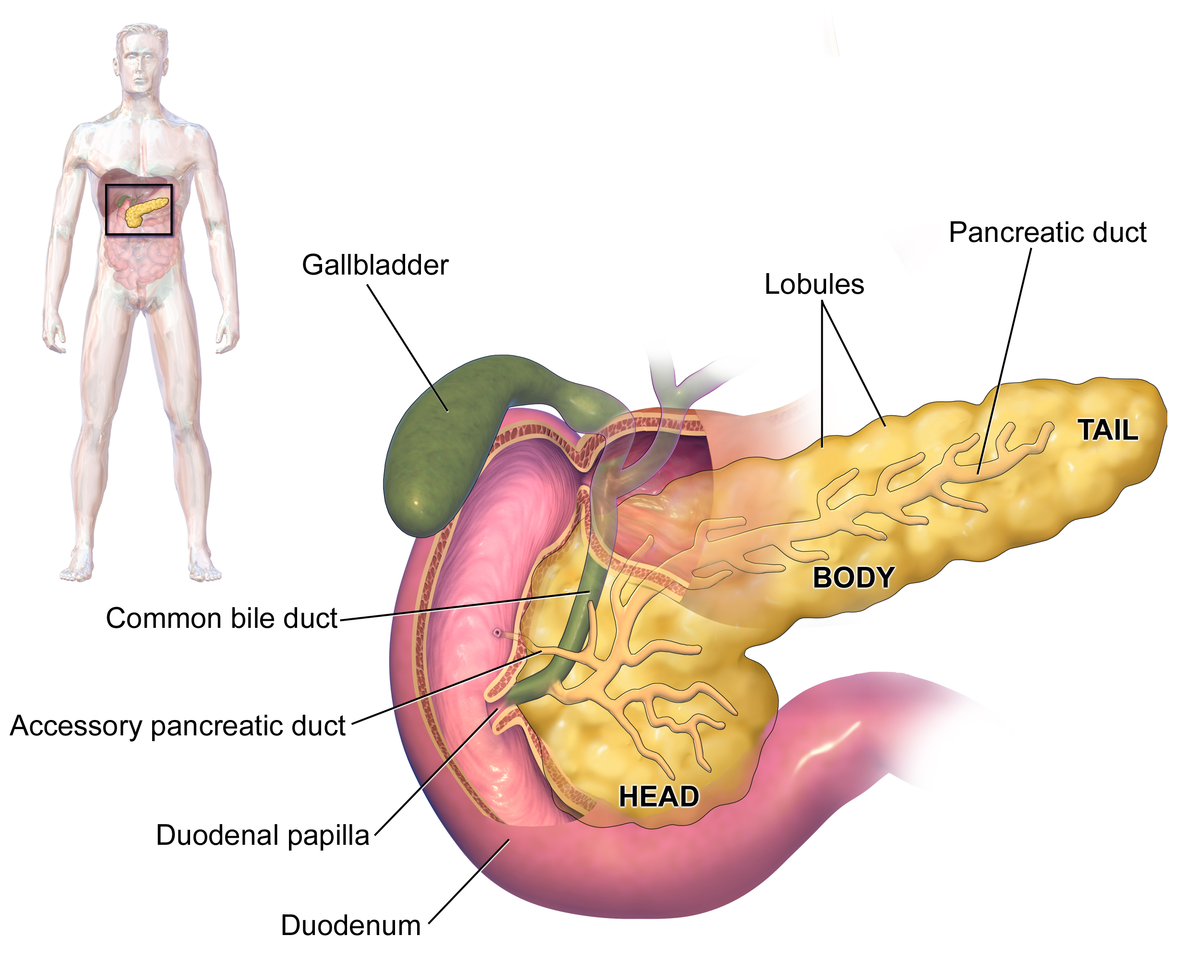
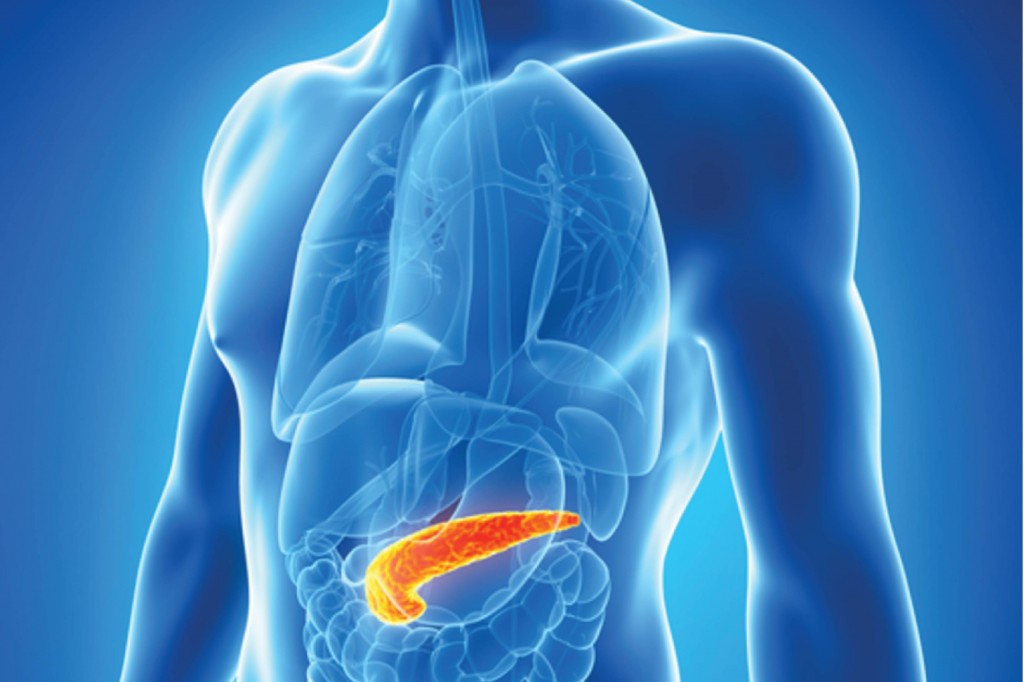
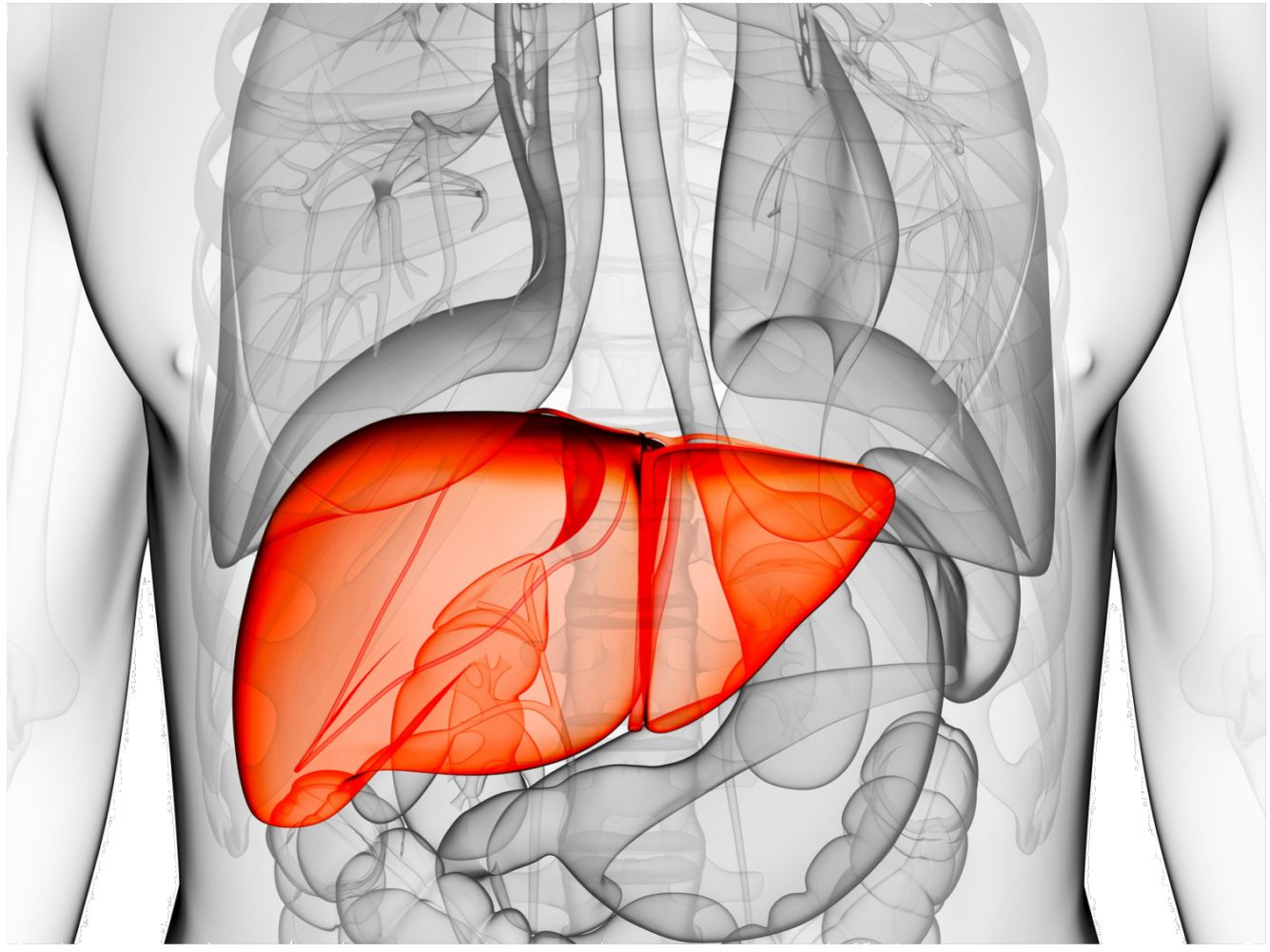
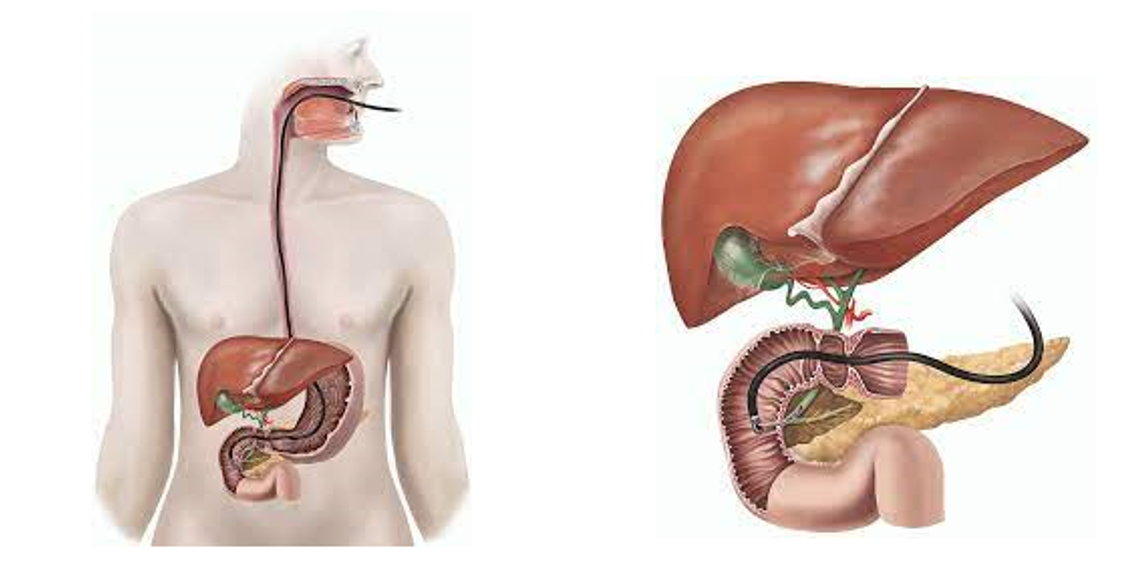
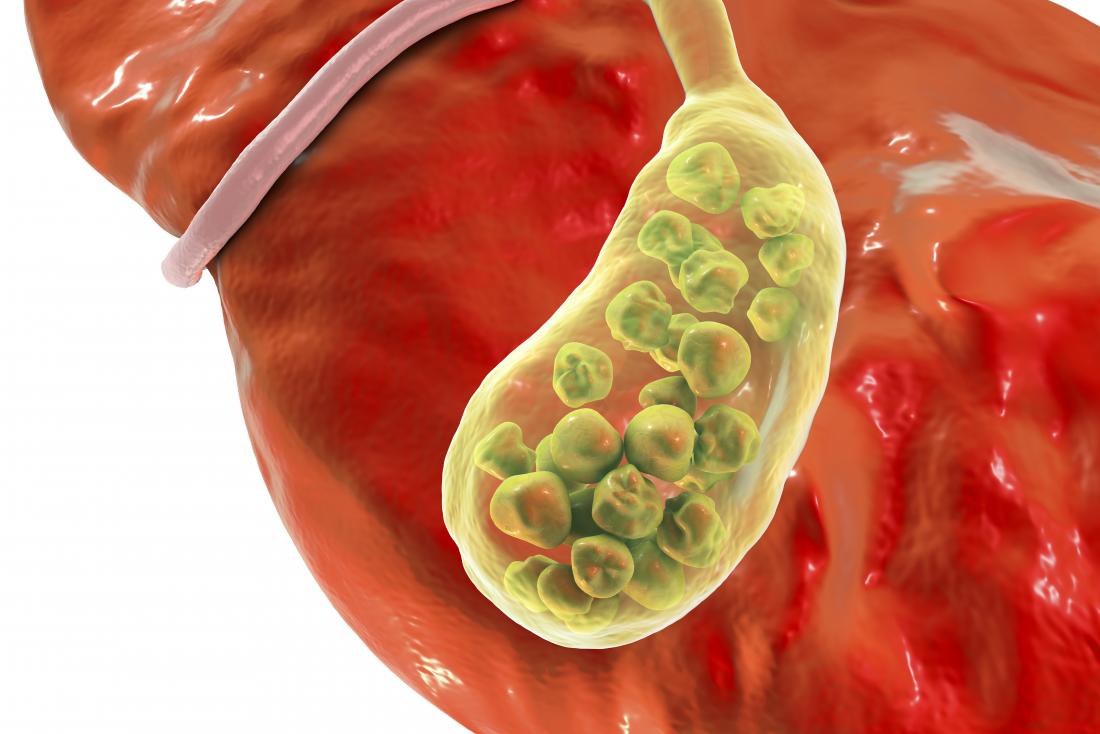
The duodenum’s “C” shape surrounds the pancreas, where it receives pancreatic enzymes for digestion. The duodenum also connects to the liver via a structure called the hepatoduodenal ligament. This junction is where the duodenum receives bile to mix with chyme, an important part of the chemical digestive process.
Segments of the Duodenum
The segments of the duodenum are-
- The duodenal bulb connects to the liver via the hepatoduodenal ligament. This connection allows nutrients to move from the small intestine to the liver. It also allows the duodenum to receive bile from the liver.
- The descending duodenum is located above the right kidney and extends down. It connects to the pancreas via a small tube called the pancreatic duct, which feeds enzymes into the duodenum to help break down food. The common bile duct carrying bile from the liver also enters this second part of the duodenum.
- The transverse duodenum extends horizontally across the abdomen. It is located in front of the aorta and travels from right to left, behind a network of blood vessels.
- The ascending part of the duodenum extends up, passing atop or slightly to the left of the aorta. This final segment leads to the jejunum, the middle portion of the small intestine.
Layers of the Duodenum
The walls of the duodenum are composed of four layers. Sometimes called duodenum histology, to describe the cells and tissues, these layers include:
- The mucosa layer is the innermost layer made up of mucus glands and microvilli, the fingerlike projections that work to absorb nutrients.
- The submucosa layer is primarily composed of connective tissue. It has a rich network of blood vessels and nerves traveling the length of the duodenum. This submucosal layer also contains Brunner’s glands, which secrete mucus to help enable food to move through, and bicarbonate. Bicarbonate is a chemical that neutralizes acid in the chyme ahead of further digestion.
- The muscularis externa layer is made up of smooth muscle tissue that's responsible for contractions in the GI tract. The muscles churn the chyme, mix it with digestive enzymes, and cause the food to move into the jejunum. This muscle movement is called peristalsis.
- The serosal layer, which is the outermost layer of the duodenum. It is composed of squamous epithelium, a single layer of flat cells that provides a barrier to other organs.
Location of Duodenum
The small intestine is located below the stomach. While the small intestine includes the duodenum, jejunum, and ileum, it's the duodenum that is connected to the stomach. Where it meets the stomach is its start. It ends where it connects to the jejunum.
Anatomical Variations
Duodenal atresia, also called duodenal stenosis, is a rare congenital (present at birth) disorder of the duodenum. It involves complete closure of a portion of the tube-like opening, or lumen, inside the duodenum.
Signs and symptoms of duodenal atresia in the fetus include a buildup of amniotic fluid during pregnancy, called polyhydramnios. Duodenal atresia also causes intestinal obstruction in newborns.
Digestive Function of Duodenum
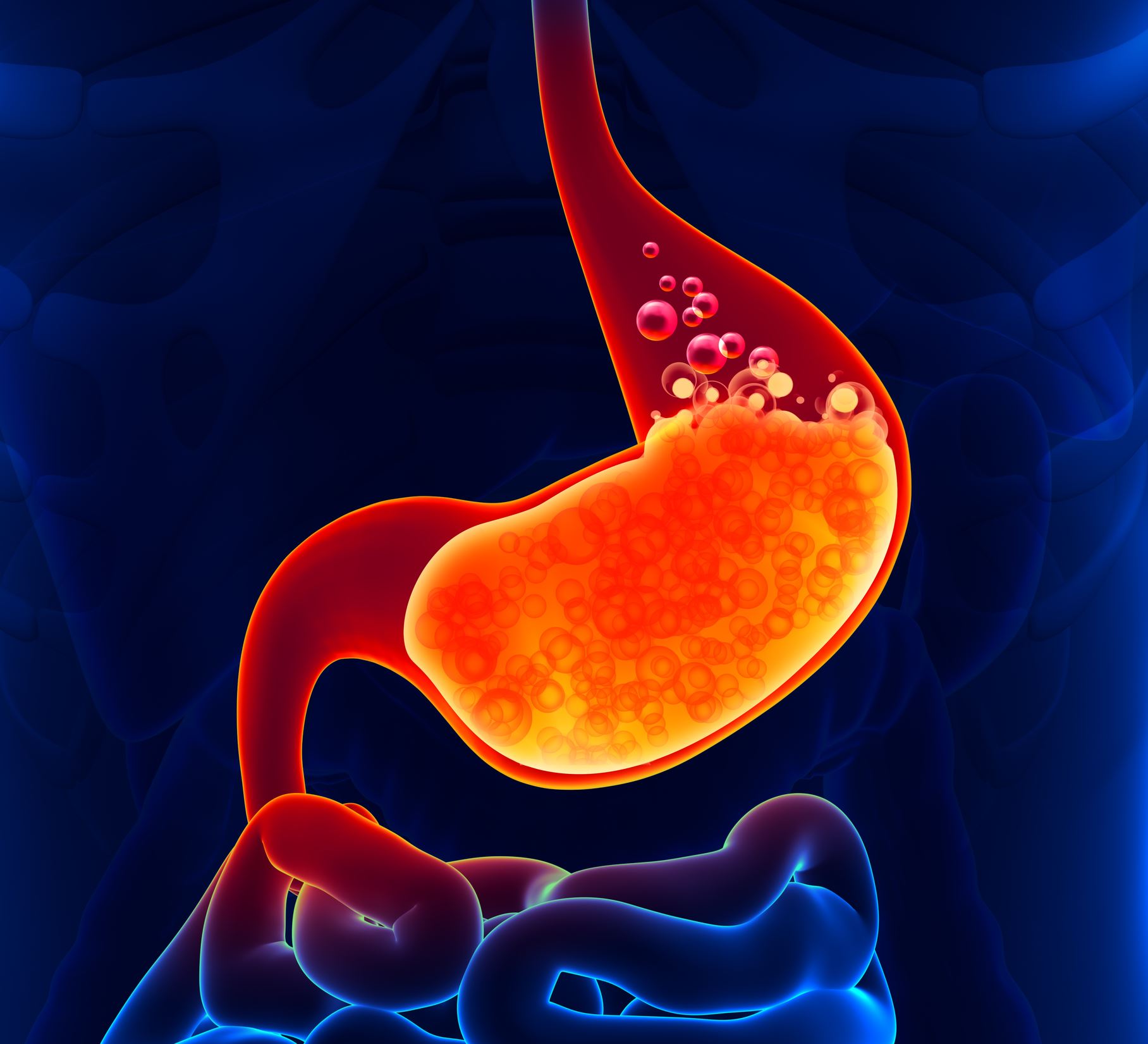
The duodenum's primary function is to begin the digestive process of breaking down and absorbing nutrients needed by the body. The duodenum begins this process by preparing the chyme so that nutrients can then be absorbed easily.
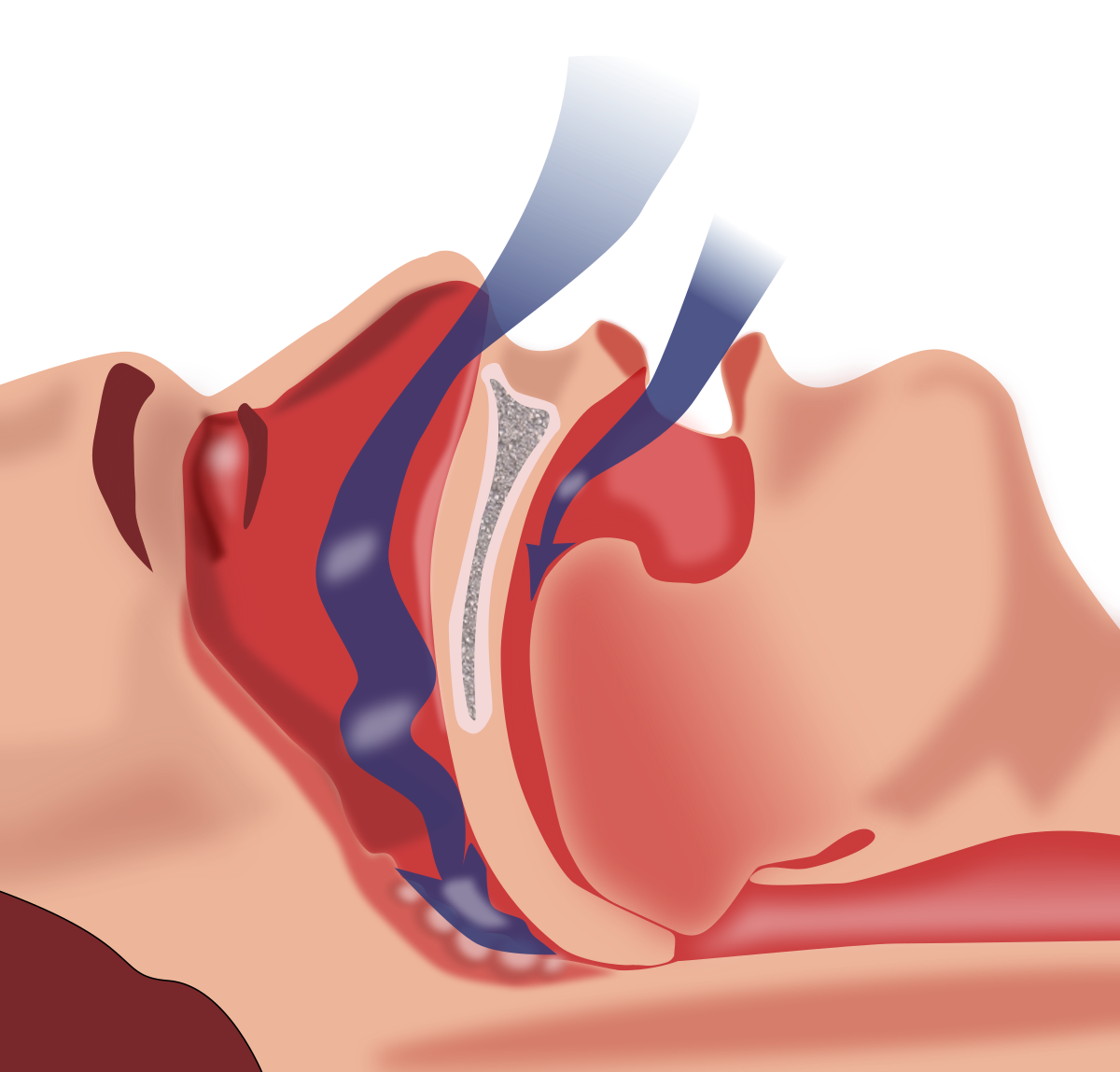
While chemical digestion begins in the mouth with saliva, food that is swallowed and travels down the esophagus into the stomach will then mix with gastric (stomach) acid. It then enters the duodenum, to begin the body's process of absorbing vitamins, minerals, and other nutrients.
The duodenum is considered the mixing pot of the small intestine because of the churning process that takes place there. It mixes the chyme with enzymes to break down food, adds bicarbonate to neutralize acids, and prepares the chyme for the breakdown of fats and proteins in the jejunum, where most of the body's nutrient absorption occurs.
Specific functions of the duodenum include:
- Receiving the mixed, churned small pieces of food from the stomach
- Neutralizing the acidity (pH level) in chyme
- Advancing the digestive process with bile from the liver, digestive enzymes from the pancreas, and intestinal juices secreted by the duodenum walls and other digestive organs
- Preparing the chyme for further digestion by mixing in bile to help break down fats
- Absorbing certain nutrients, such as folate, iron, and vitamin D
Duodenum's Other Functions
The duodenum contributes to other important digestive processes in the body. This includes the release of two key hormones:
- Secretin, which is released when the pH of the duodenum needs adjusting (specific pH levels are needed for proper digestion of fats and proteins)
- Cholecystokinin, which is released to aid in the digestion and absorption of nutrients such as fats and proteins
Another important function of the duodenum is immune support. The duodenum acts as a barrier to prevent harmful microbes from entering the body.
The friendly bacteria in the duodenum and other parts of the small intestine take up space and compete for food inside the duodenum. As a result, pathogens (disease-causing germs) have a difficult time multiplying there.
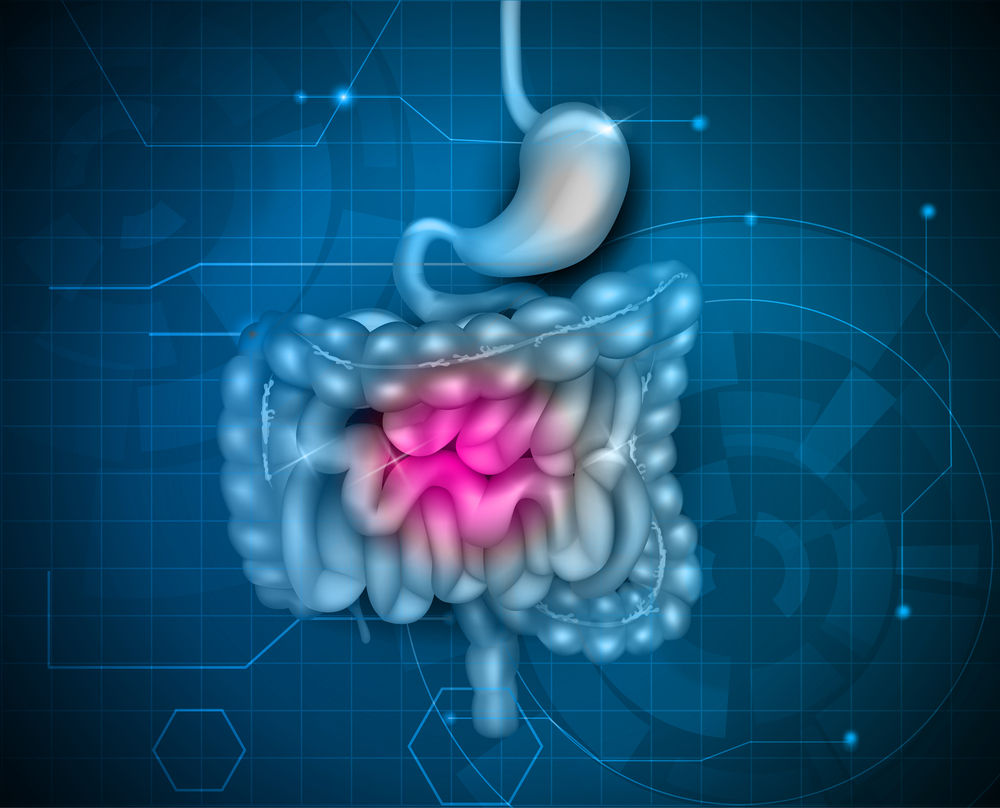
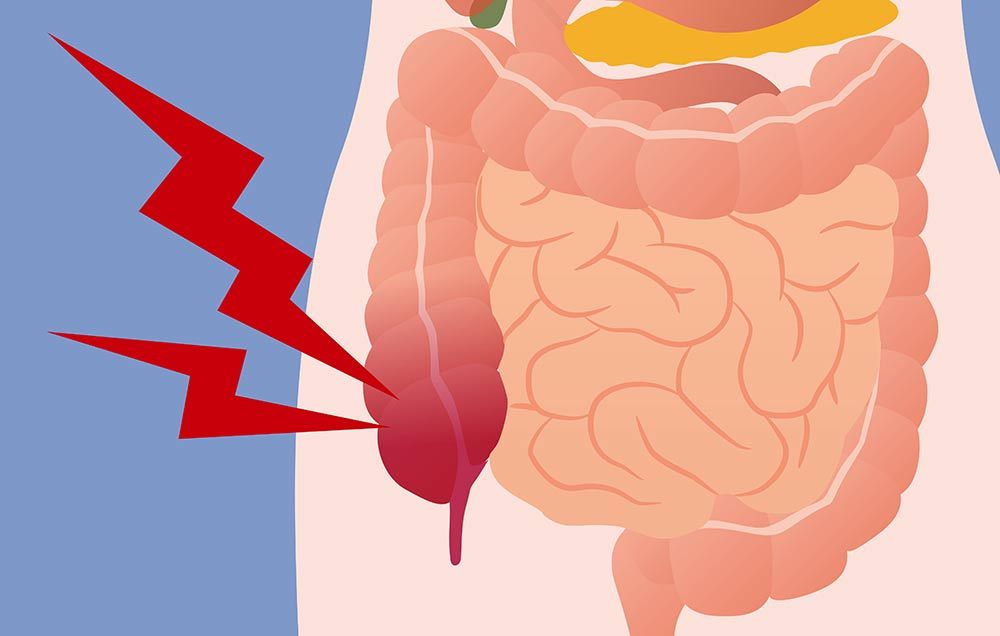
Symptoms of Duodenal Disorders
The duodenum is affected by disorders or disease that may be acute (short-term and severe) or chronic (long-term). Symptoms such as discomfort or a burning sensation in the abdominal region may be present. Other symptoms may include:
- Feeling bloated after eating (even small amounts)
- Nausea and vomiting
- Indigestion
- Pain in the lower abdomen (or in some cases, pain felt in the lower back)
- Black tarry stools, which can occur if there is intestinal bleeding
A condition affecting the duodenum may not result in any symptoms at all. It may be diagnosed when a person is being examined for another type of digestive disorder.
Duodenum and related Health Conditions
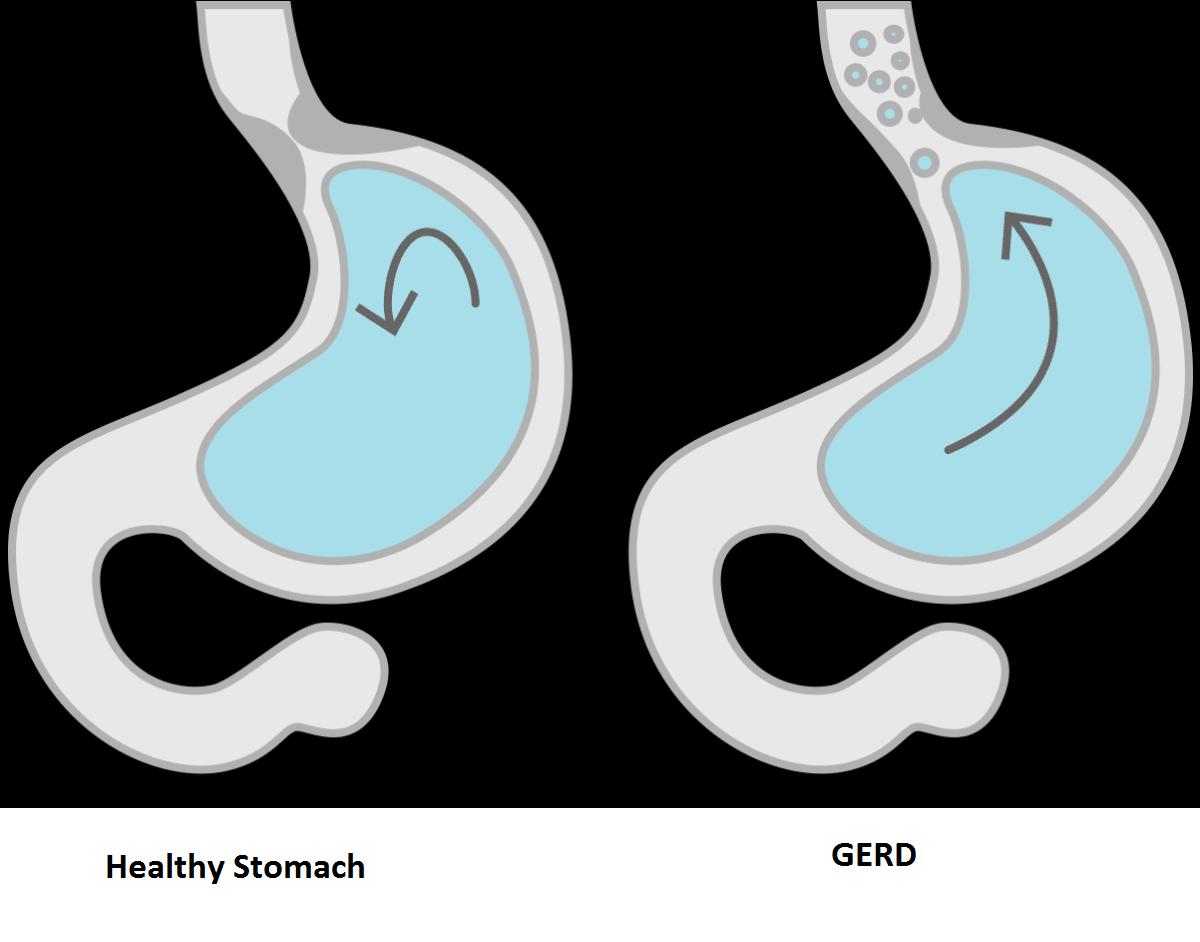
The duodenum can be affected by a number of health conditions common to people of any age. For example, the duodenum is a common source of abdominal discomfort, with symptoms of indigestion, heartburn, and upper abdominal pain.
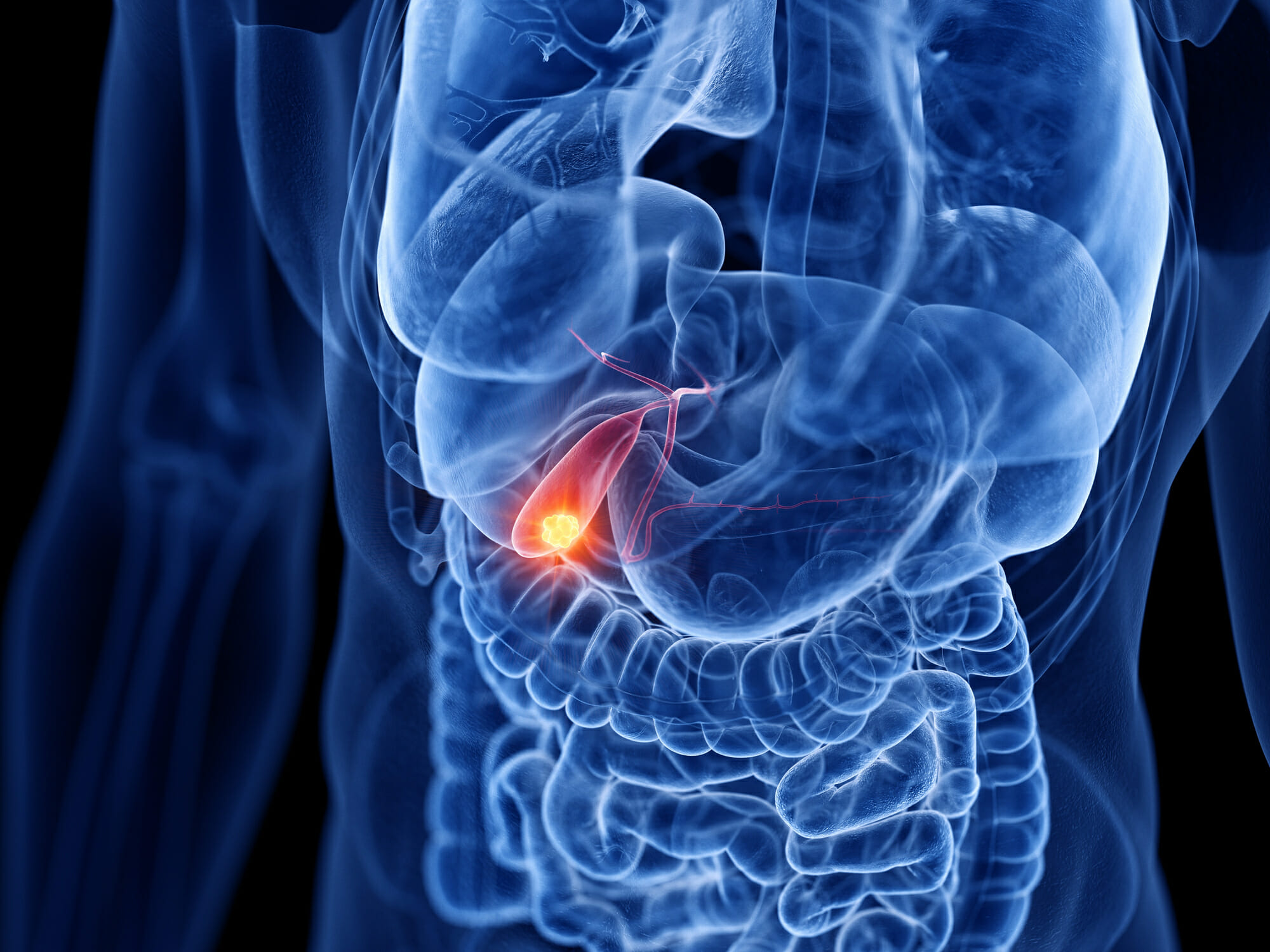
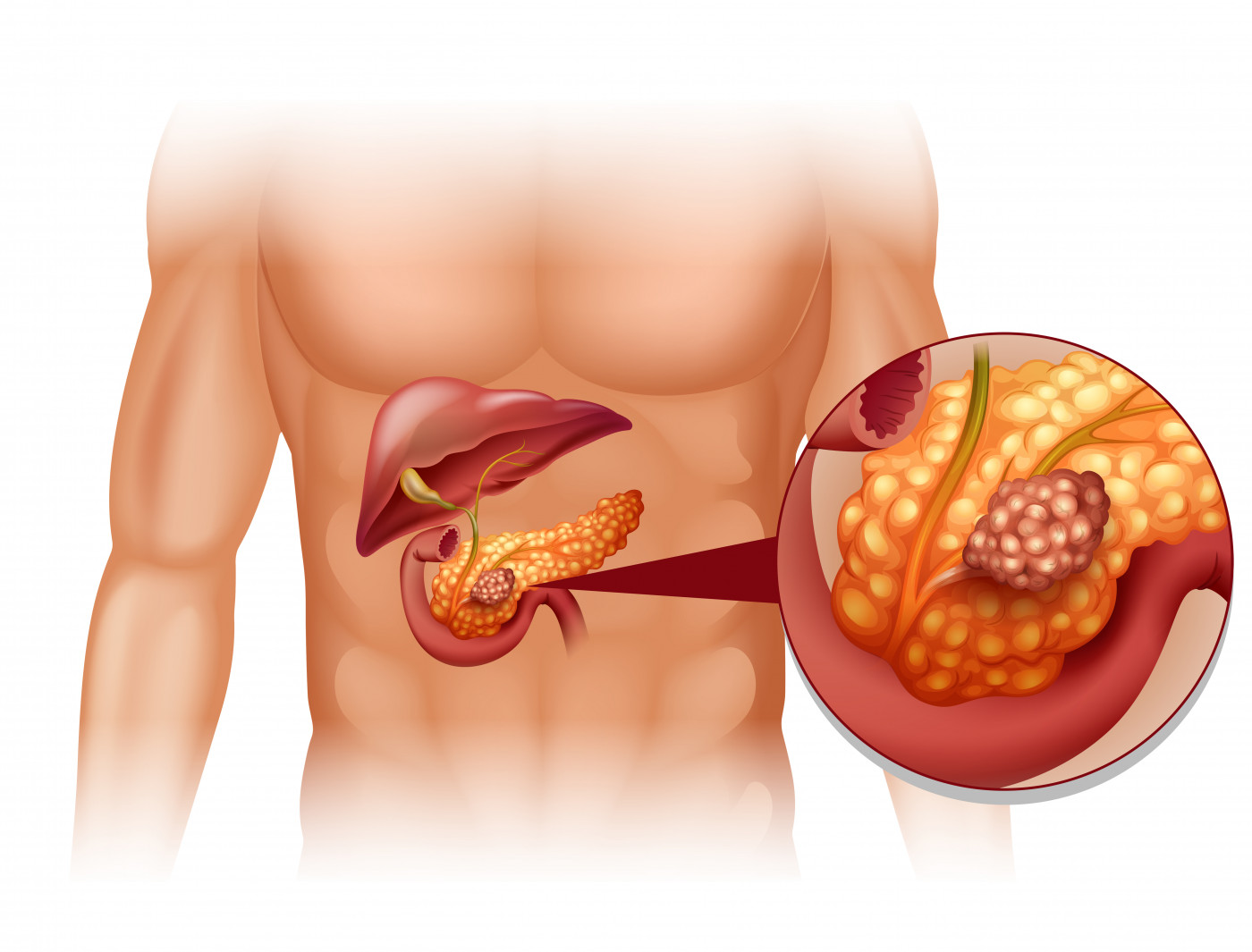
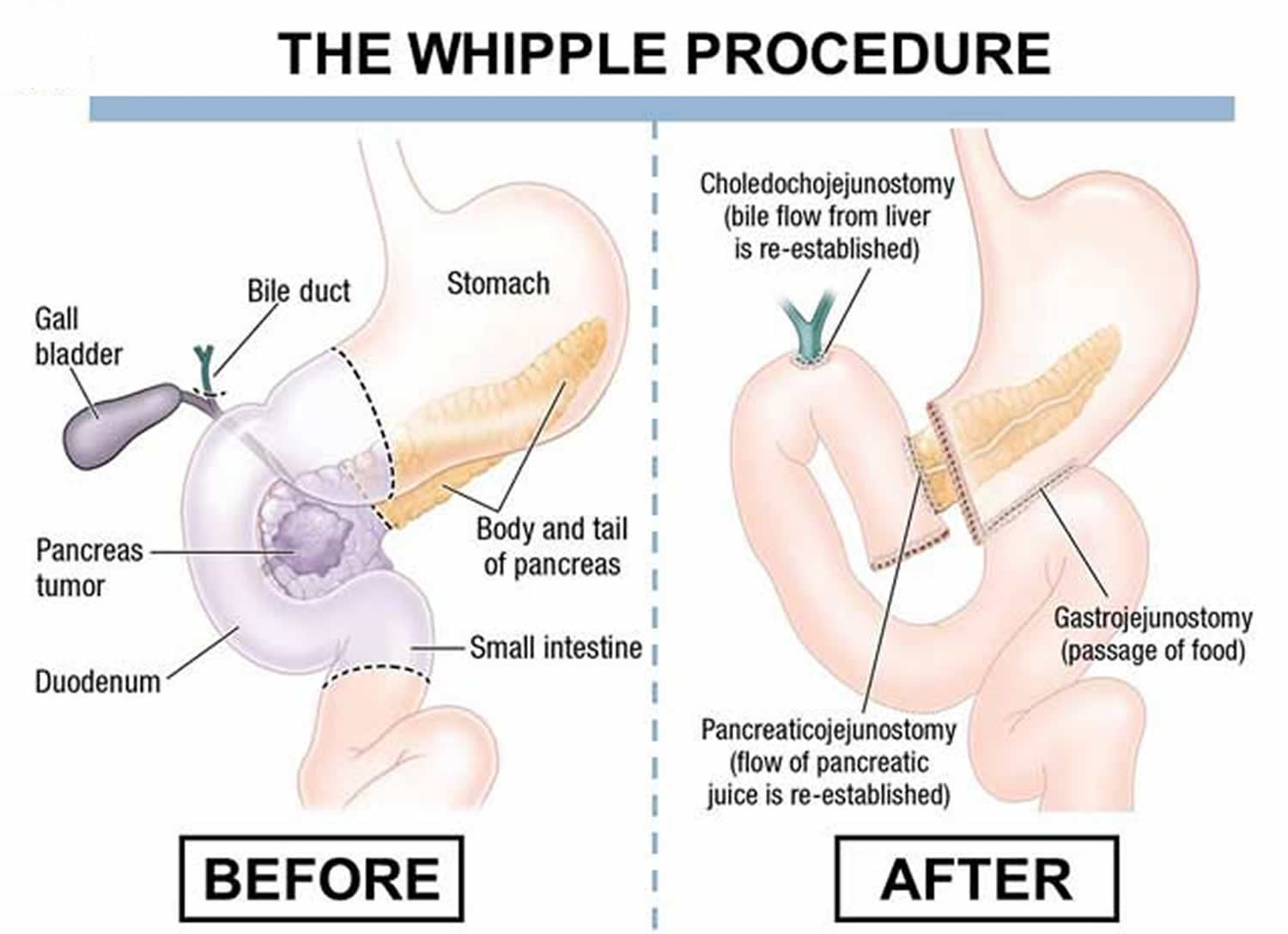
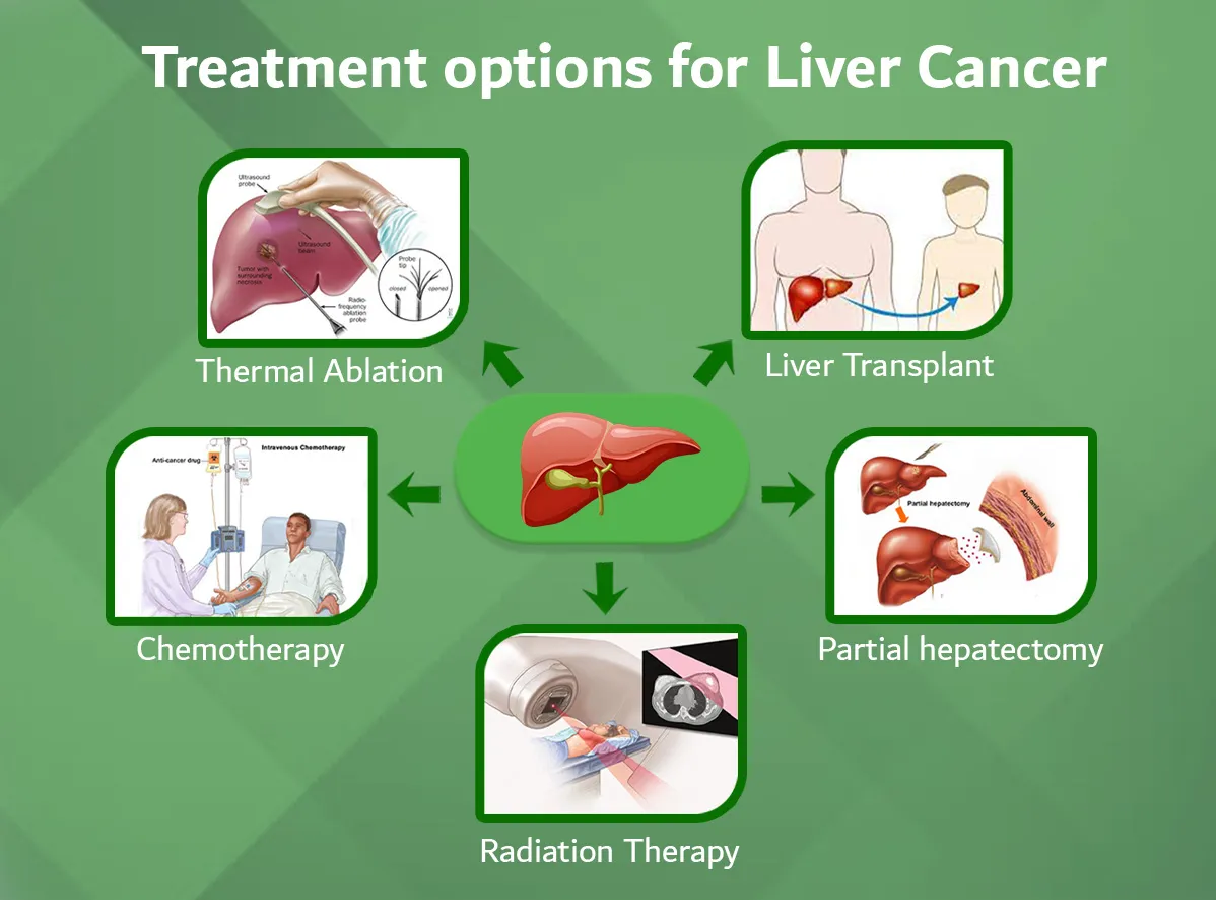
Duodenum and Cancer
Due to a complex connection between the duodenum and the accessory organs of digestion, such as the liver and pancreas, cancer cells are often seen at the same time in both the duodenum and pancreas, as well as the bile duct of the liver.
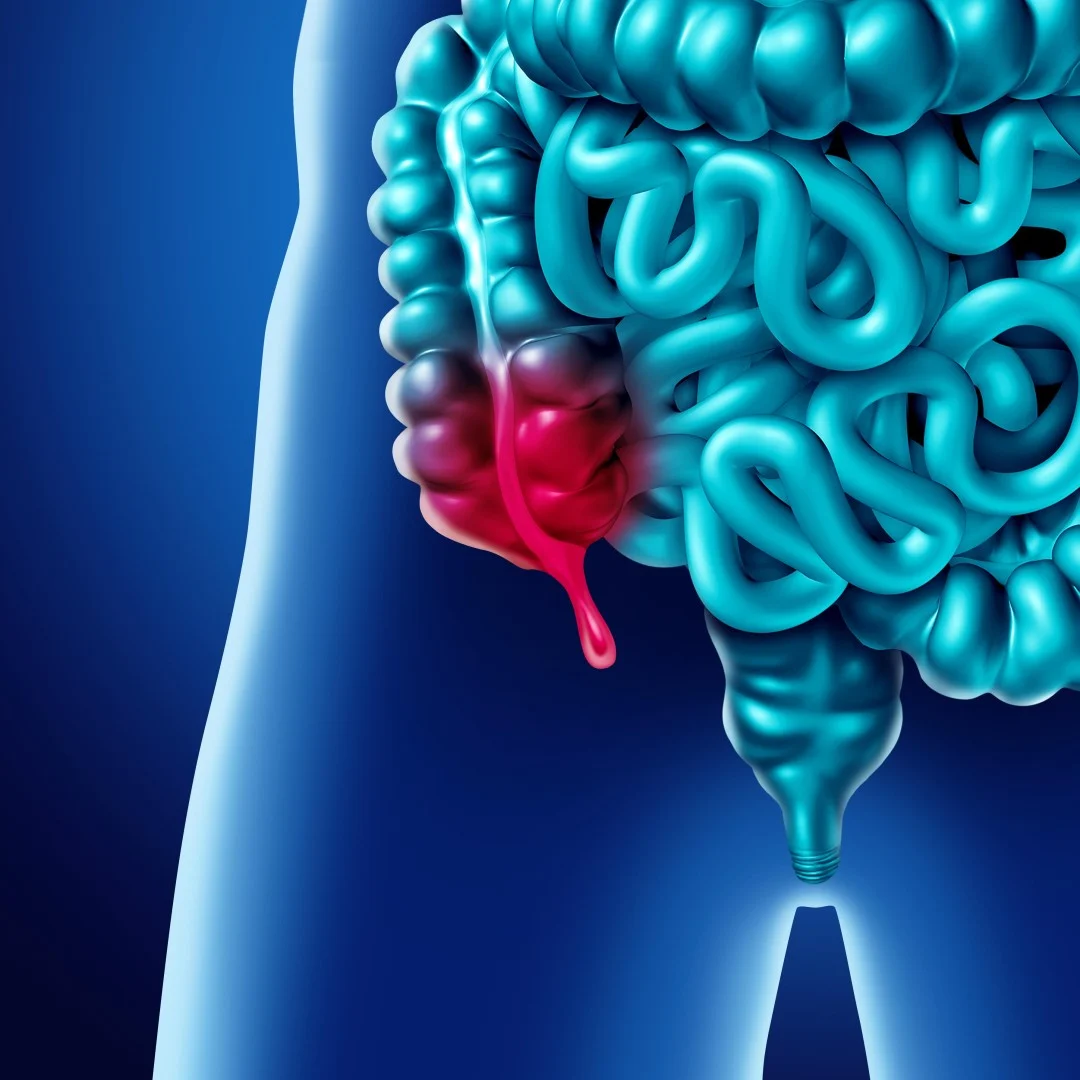
Other common disorders of the duodenum include:
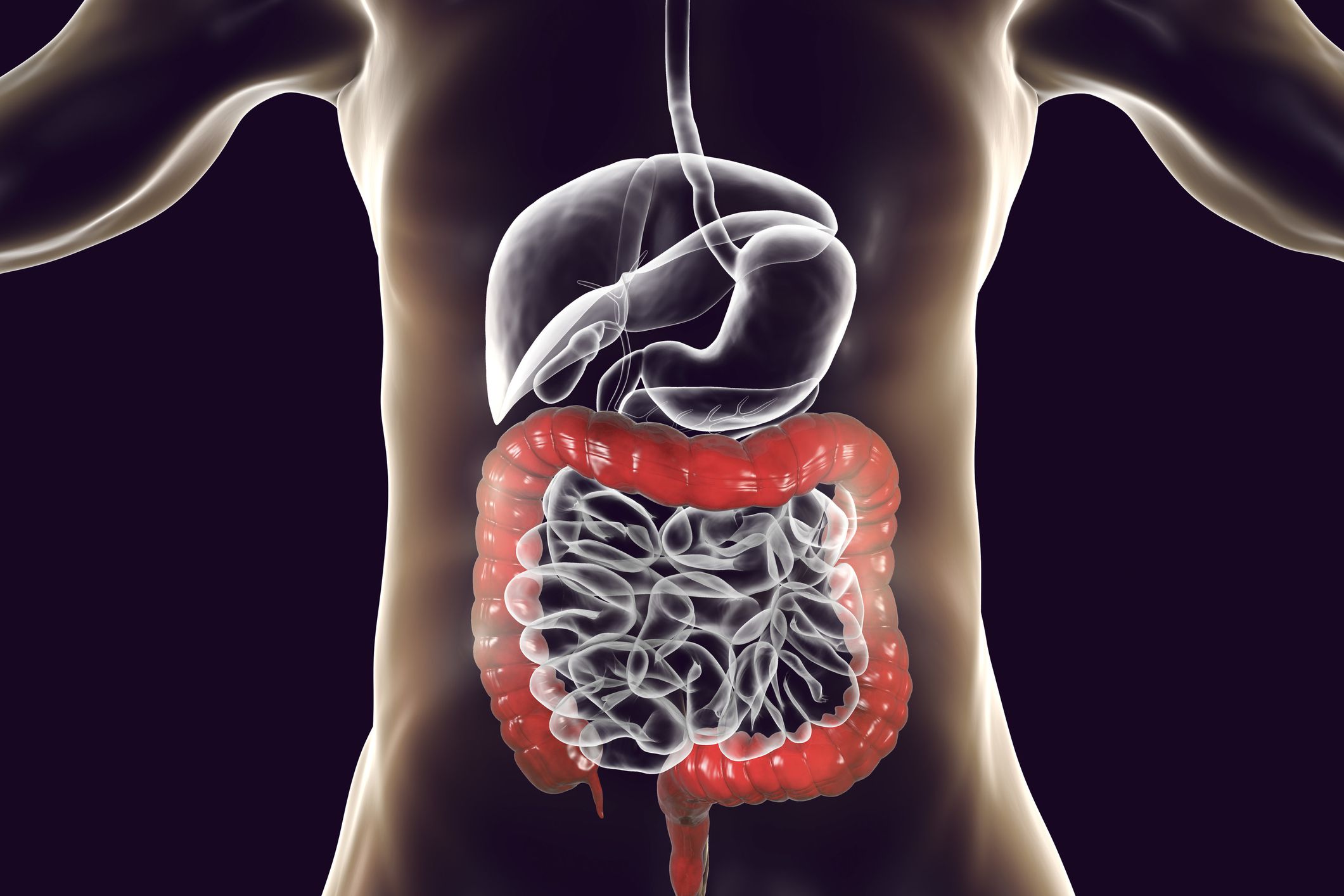
- Inflammatory bowel disease (IBD), which may cause inflammation in the duodenum or the stomach. Inflammatory bowel disease has two types: Crohn's disease and ulcerative colitis. Only Crohn's disease affects the duodenum. Ulcerative colitis does not affect the duodenum.
- Celiac disease, a condition that particularly impacts the duodenum due to adverse effects when a person eats gluten or wheat products.
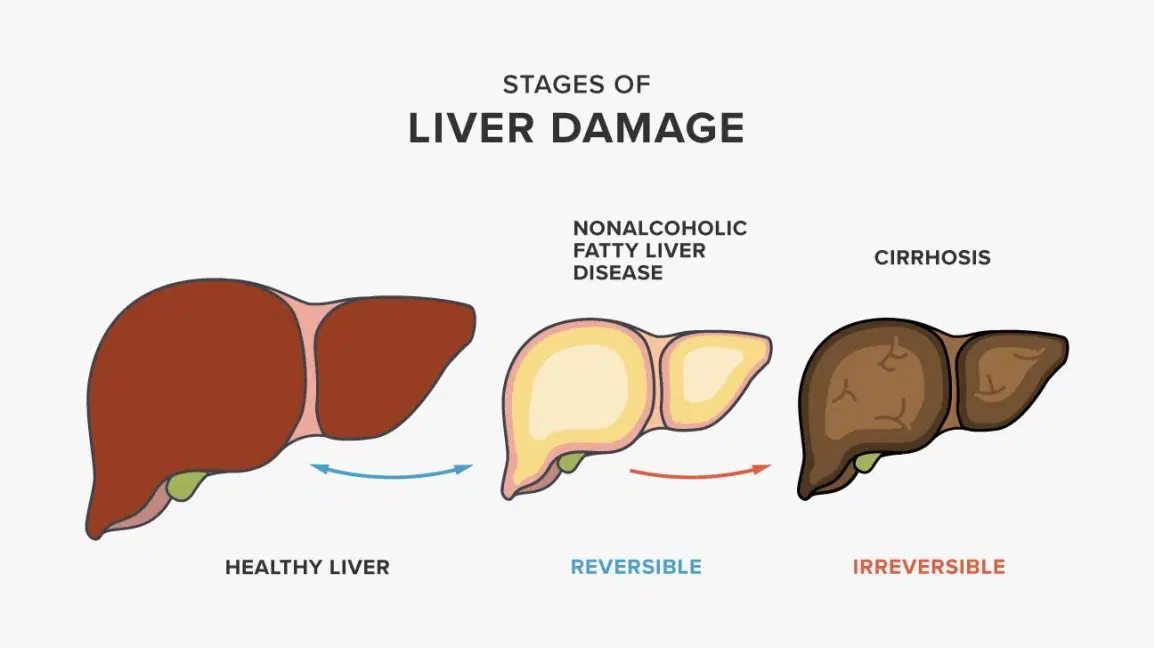
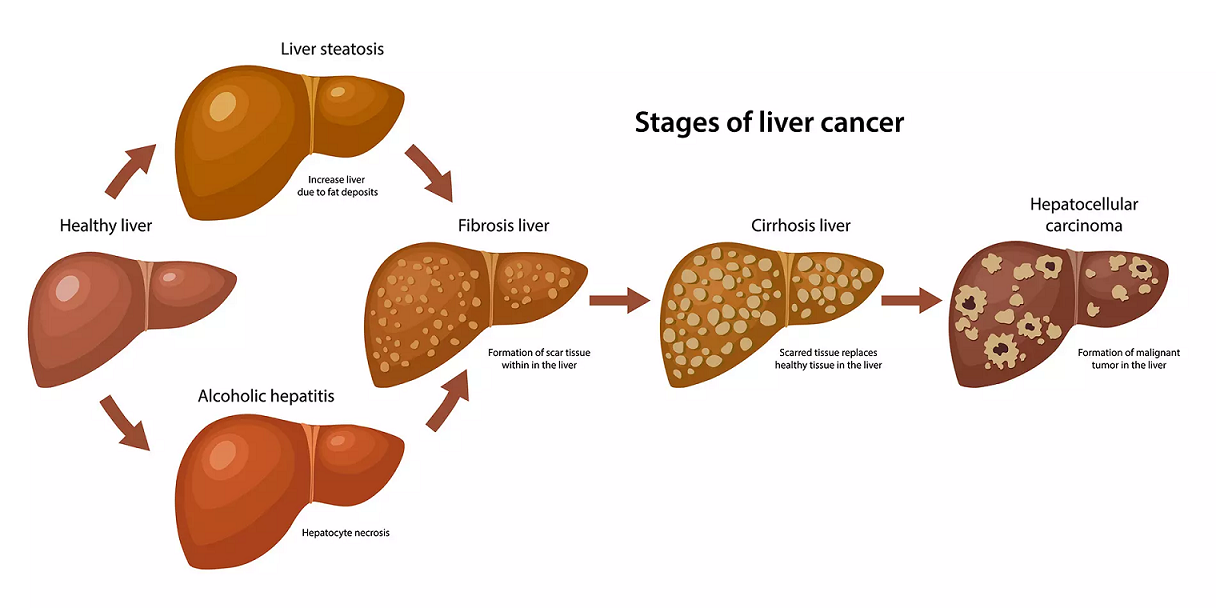
- Excessive alcohol consumption, which can cause duodenitis, an inflammation of the duodenum
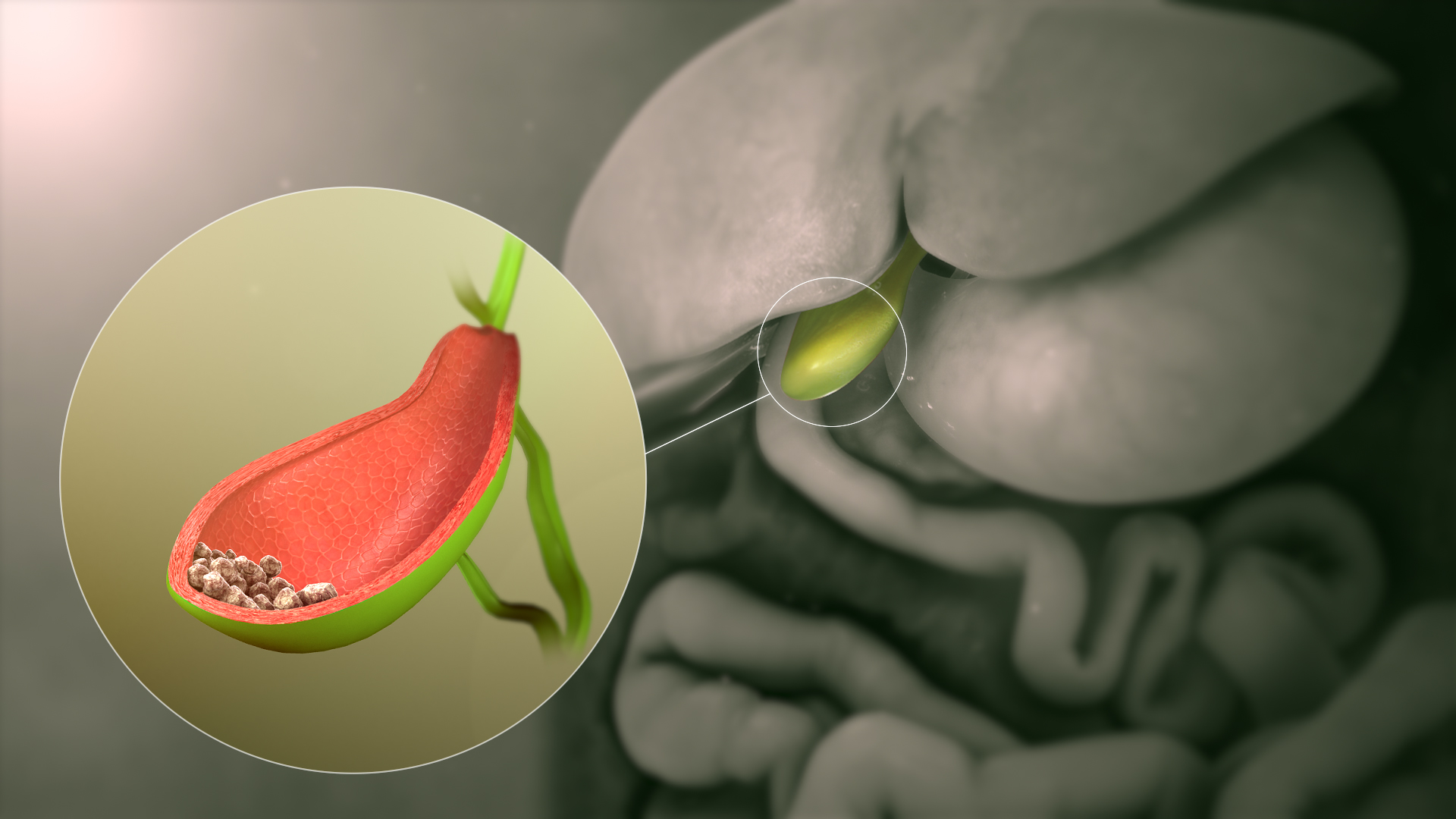
- Duodenal ulcers, lesions similar to stomach ulcers that form in the lining of the duodenum
Duodenitis can have several different causes, including a Helicobacter pylori infection (H. pylori) that commonly causes ulcers and inflammation in the stomach and duodenum. Other types of bacterial infection may cause inflammation too. Additional causes of duodenitis include:
- Viral infections
- NSAIDs (nonsteroidal anti-inflammatory drugs), a class of pain medications such as Advil (ibuprofen) that can lead to inflammation with long-term use.
- Duodenal lymphocytosis, a condition involving an increase of small white blood cells, called intraepithelial lymphocytes, in the lining of the duodenum (discovered via a biopsy)
- Smoking tobacco (heavy use)
- Accidental injury or surgery affecting the duodenum
- Chemotherapy or radiation therapy
- Idiopathic (unknown causes)
Different types of duodenitis are treated in different ways, including antibiotics to treat an infection. It's an especially effective treatment in cases caused by H. pylori infection. Duodenitis is curable in most cases, though, some instances may become a chronic condition.
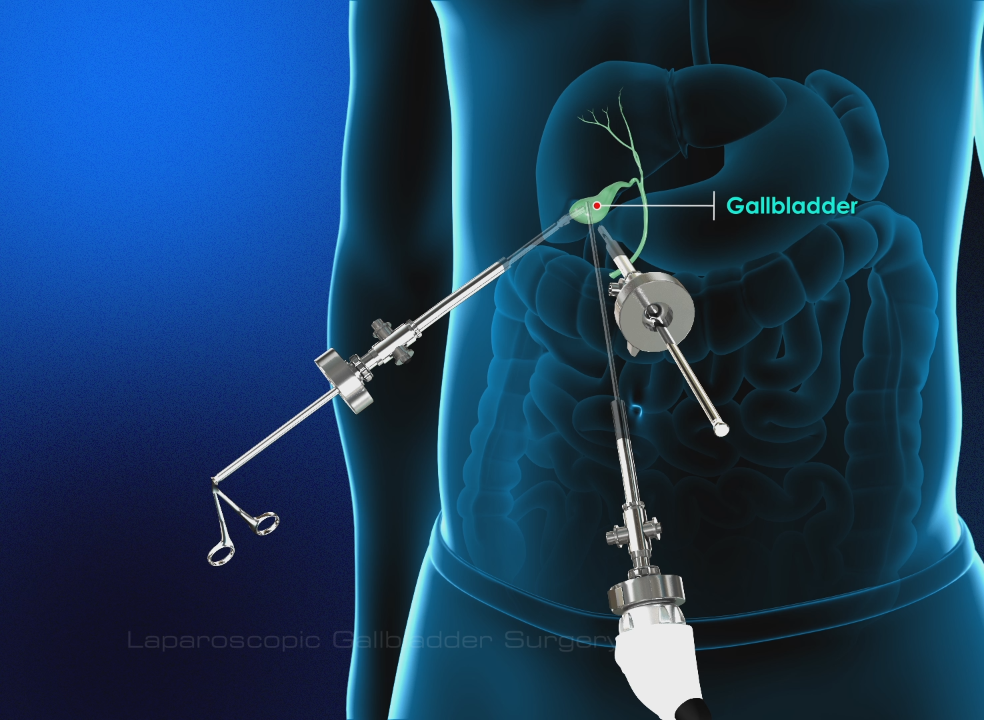
Can You Live Without the Duodenum?
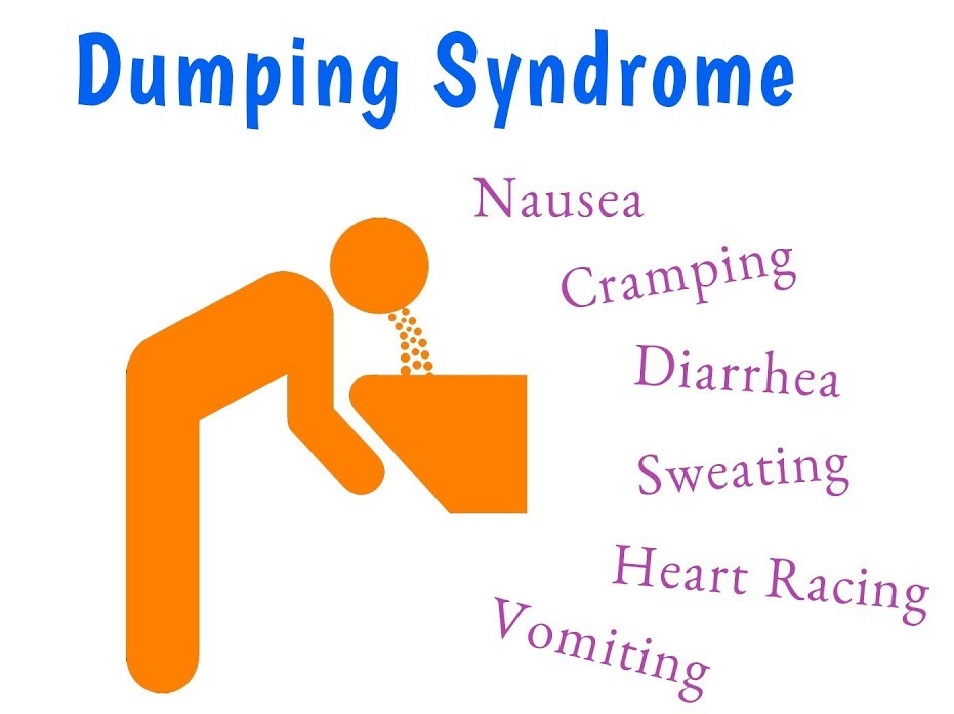
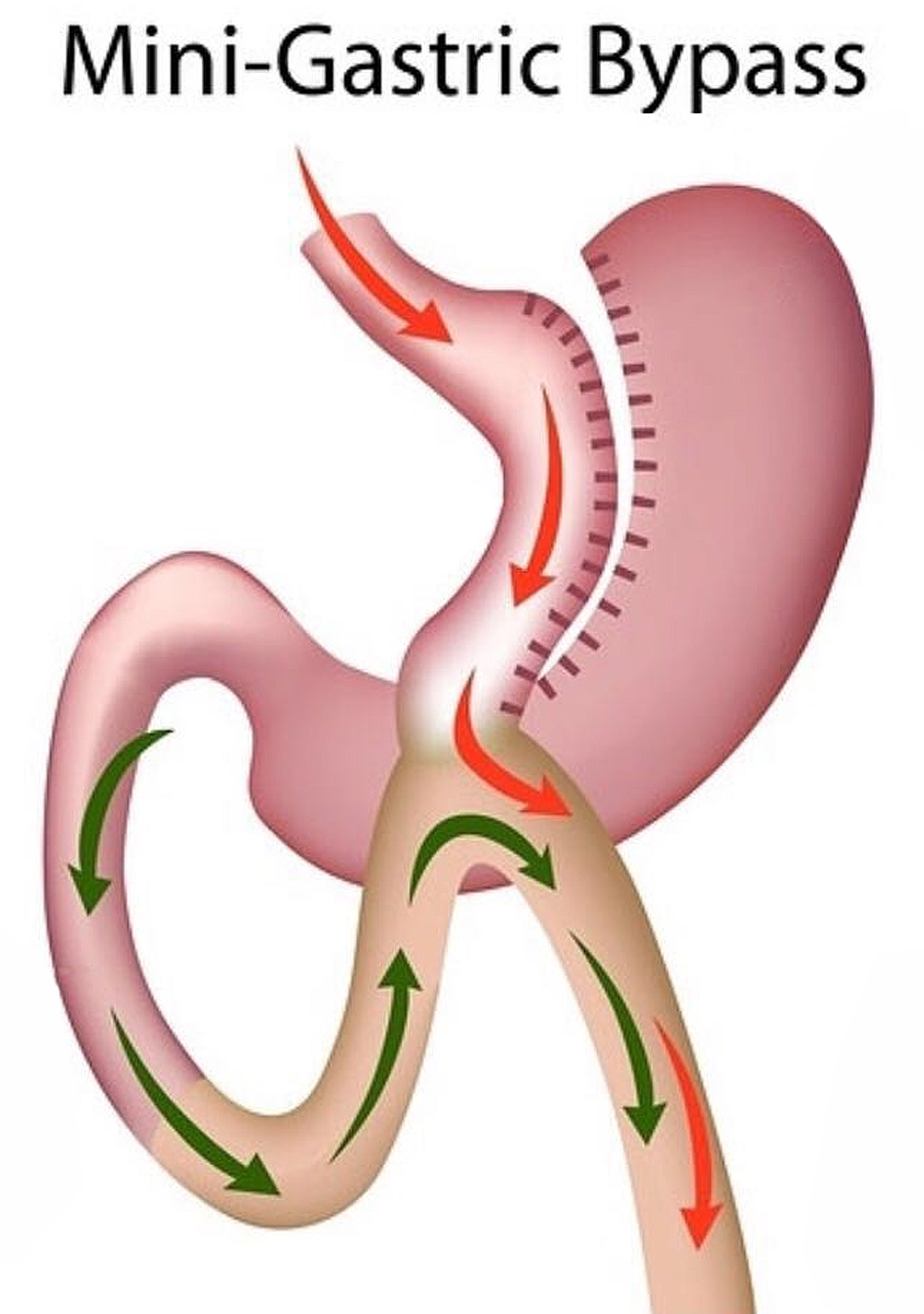
Yes, but it's likely you'll experience complications. For example, a pancreaticoduodenectomy (Whipple procedure) can be done to treat duodenal and pancreatic cancer. It's a complex procedure, with side effects that include digestive problems and bowel habit changes.
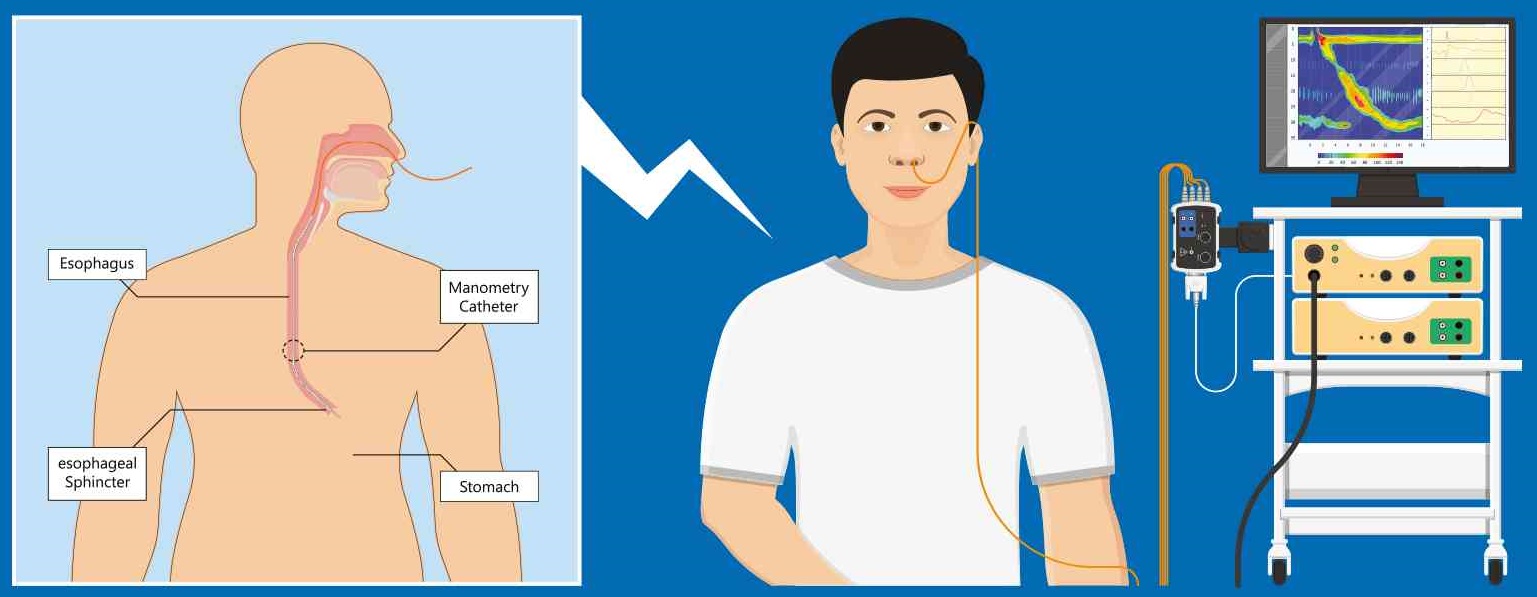
Duodenum and Diagnosis
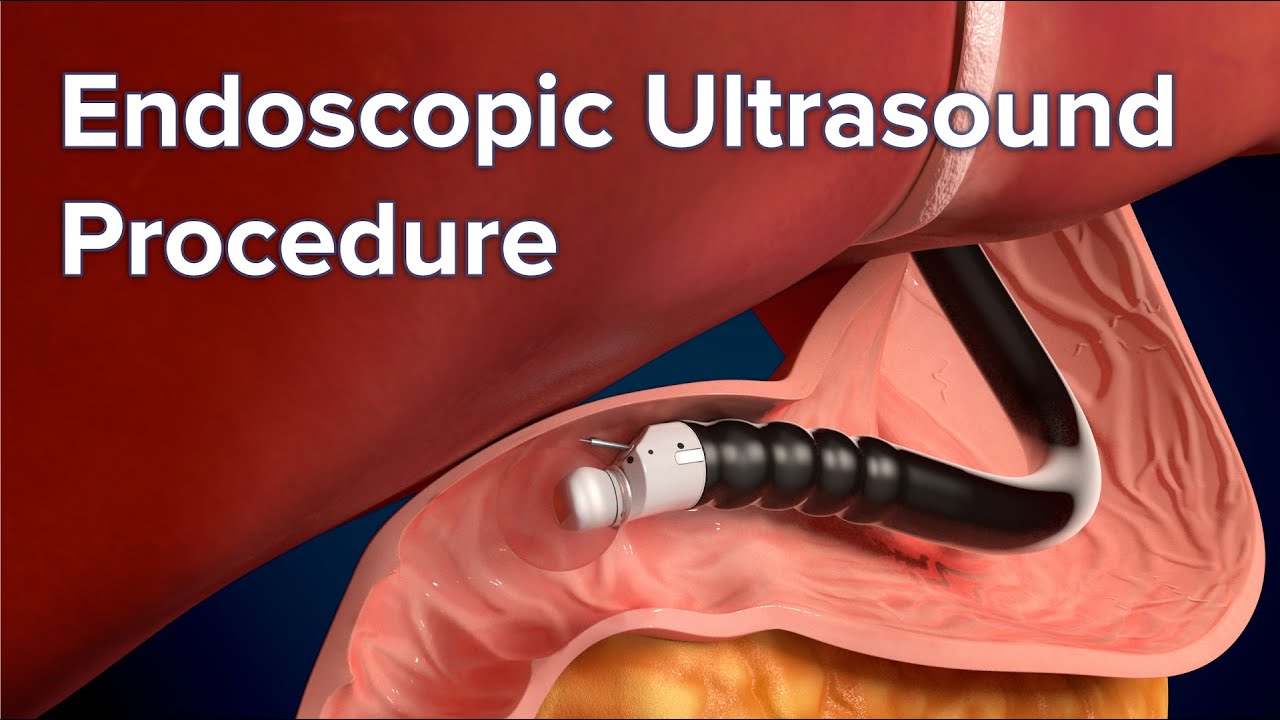
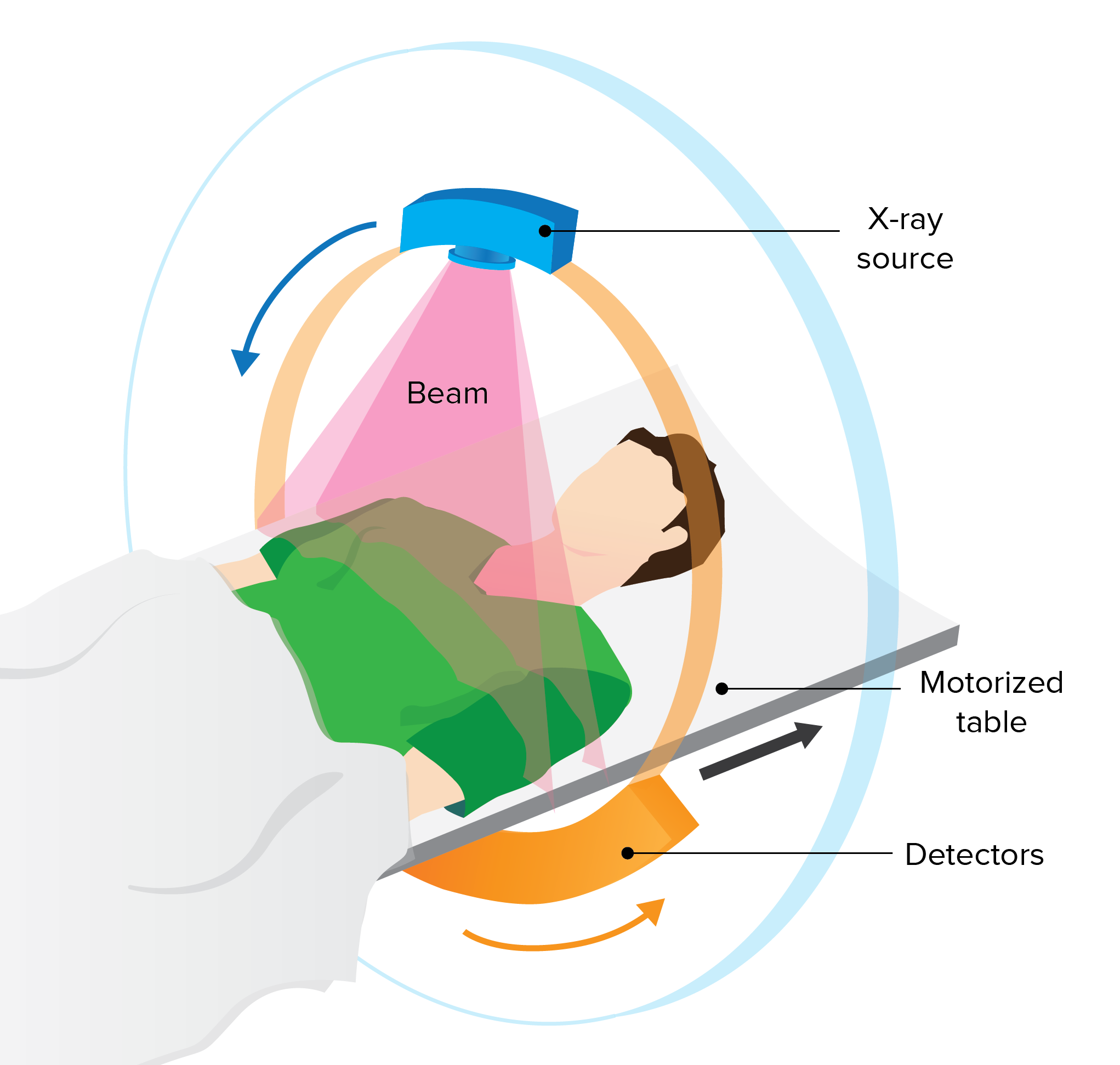
Several tests are commonly used to diagnose conditions of the duodenum, including duodenitis. These include:
- Blood or stool samples (to test for H. pylori)
- A urea breath test to test for H. pylori, done before and after a person drinks a solution
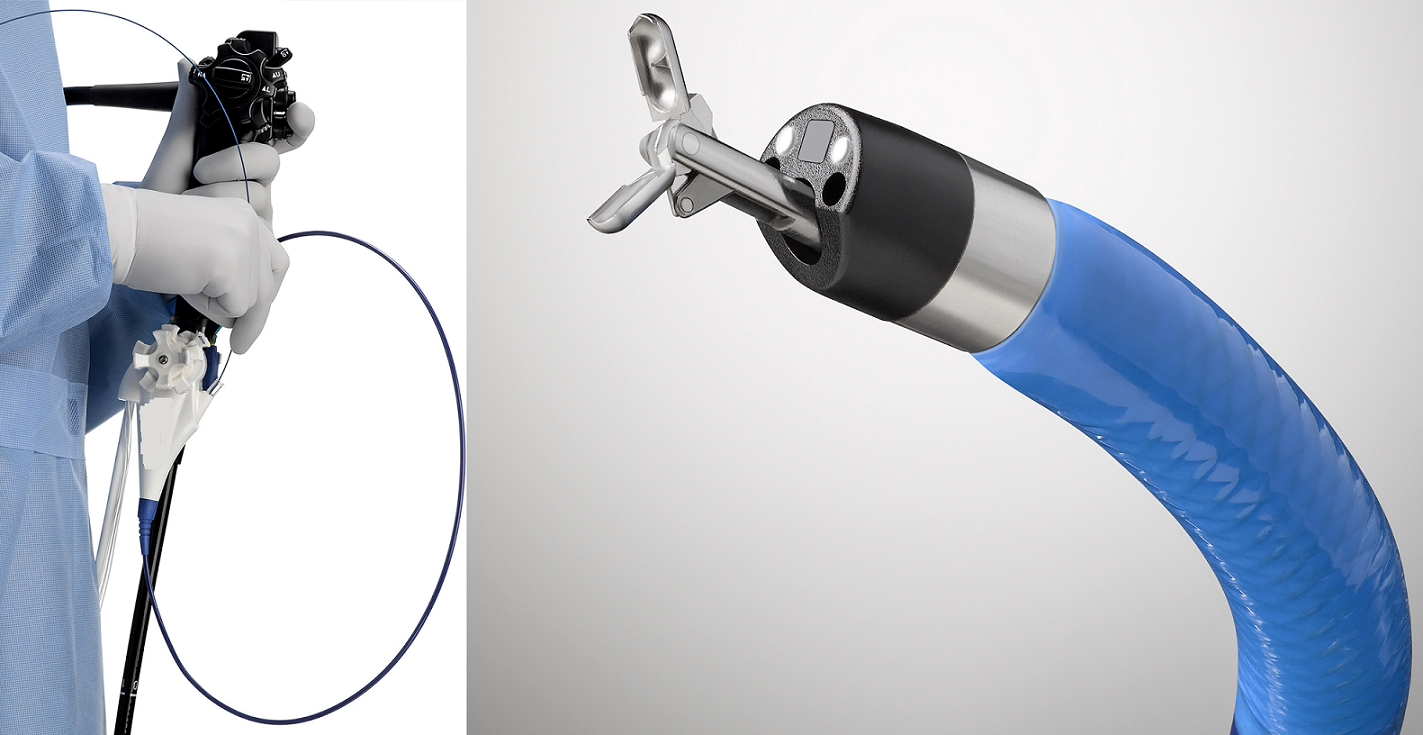
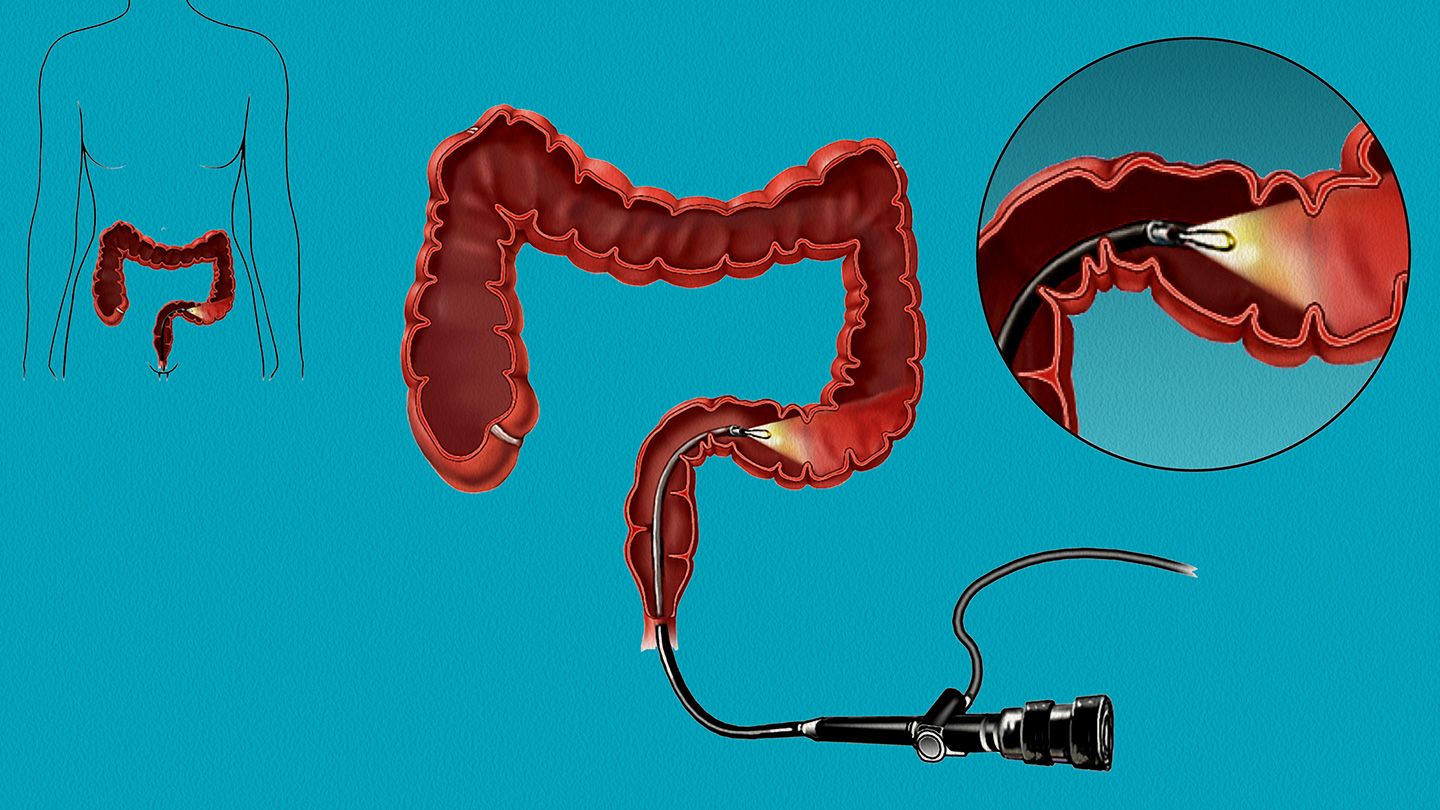
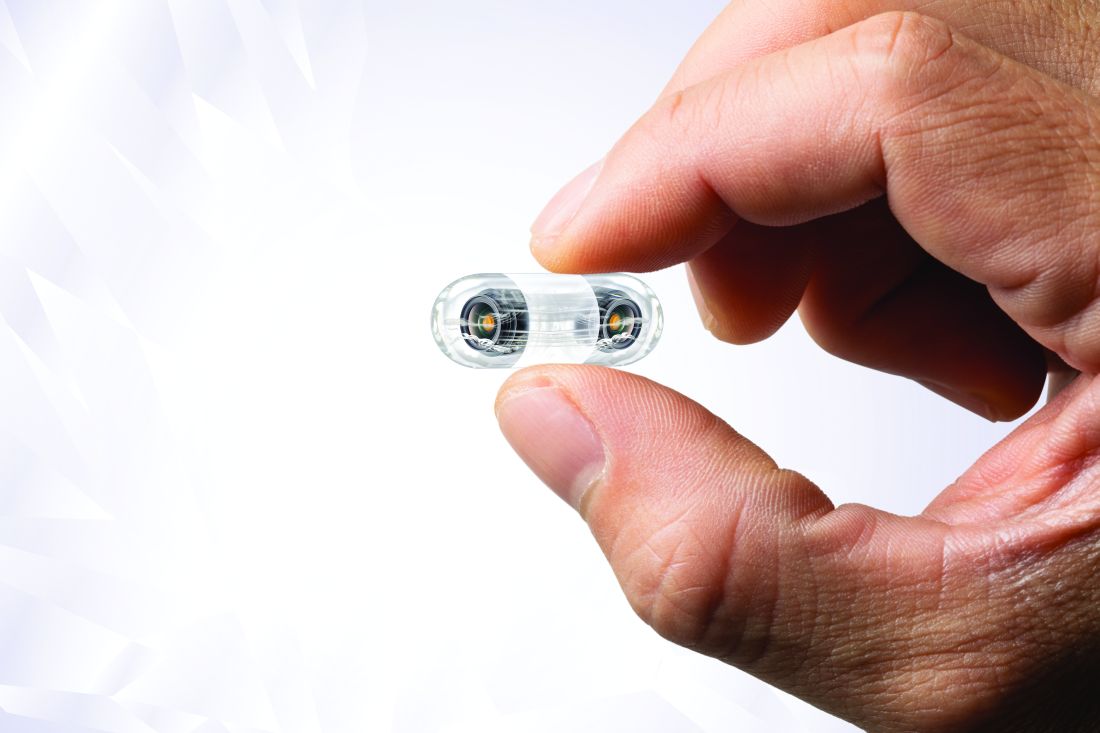
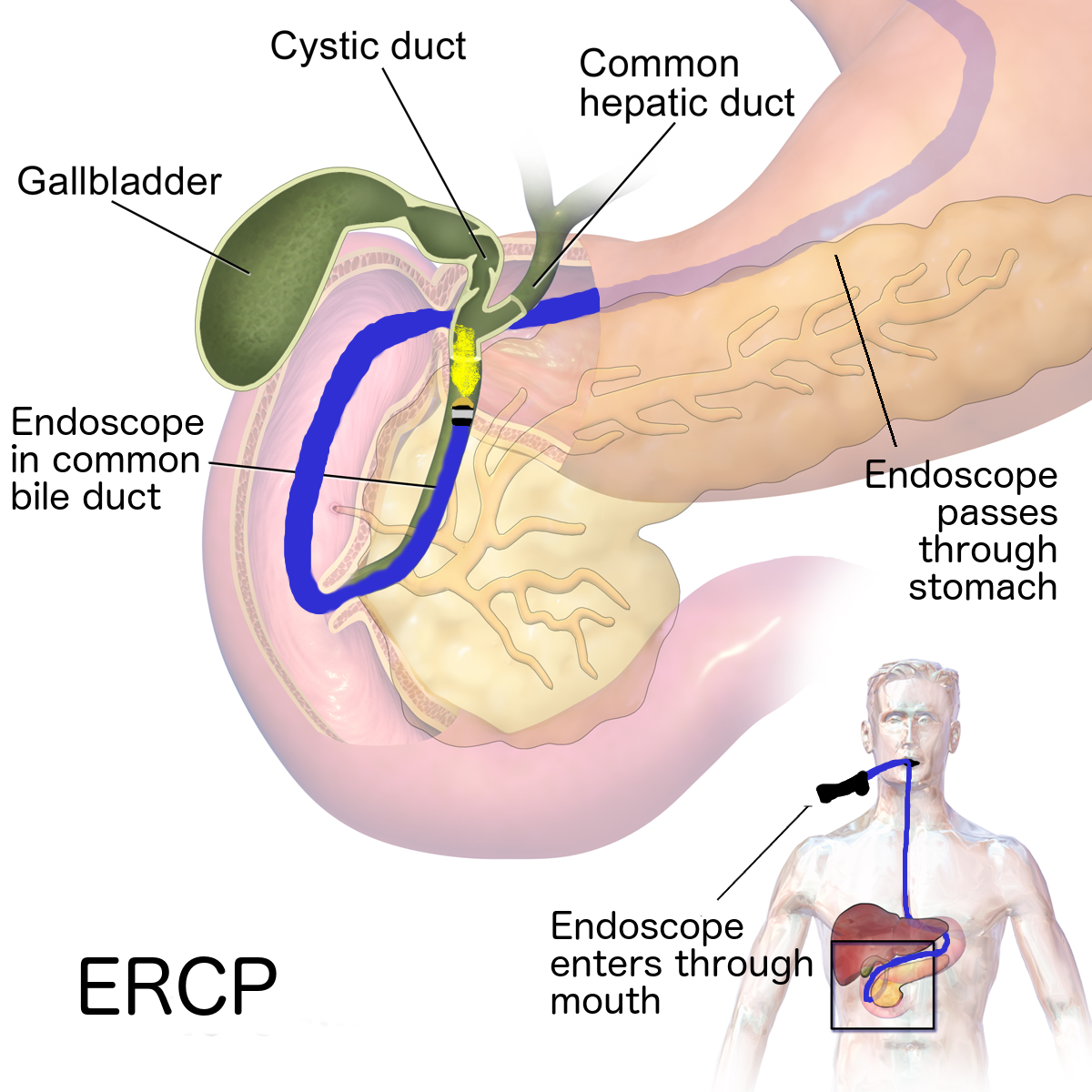
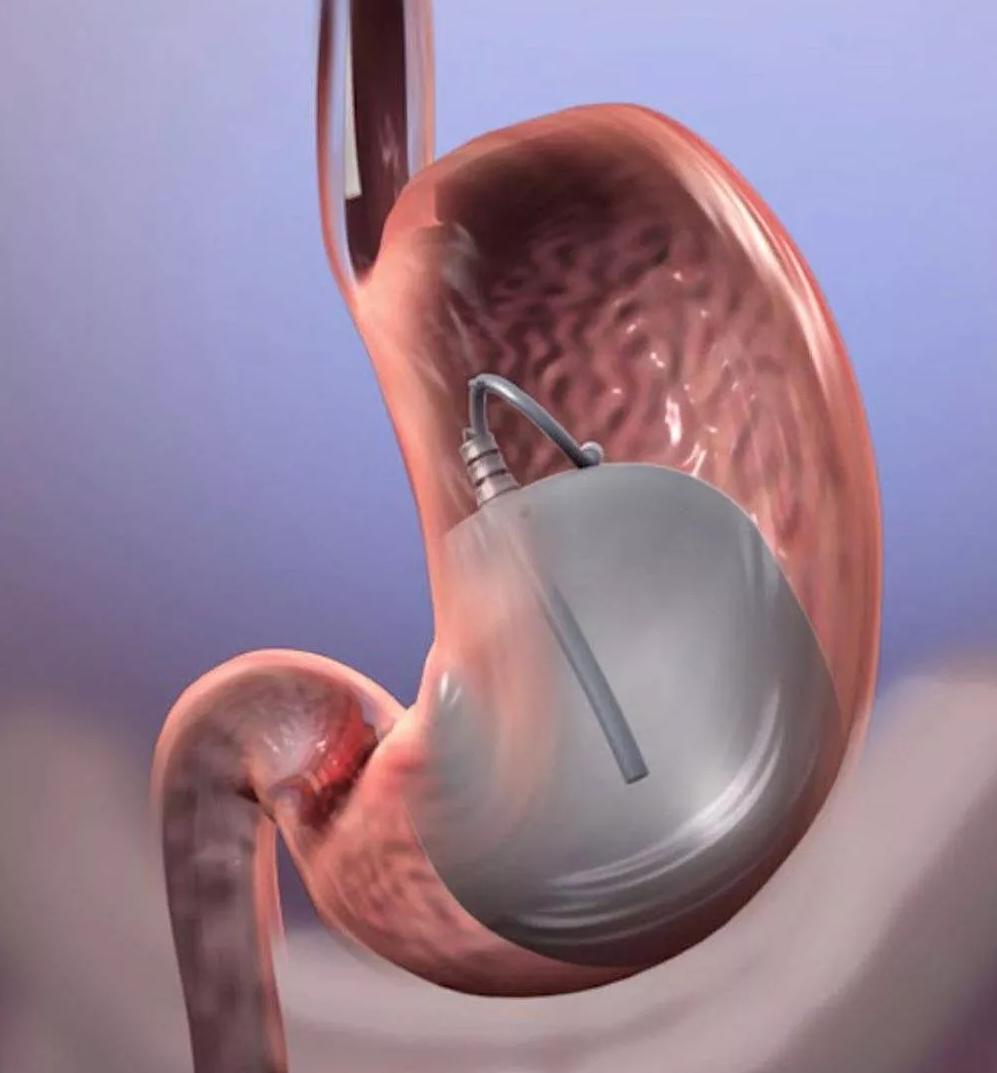
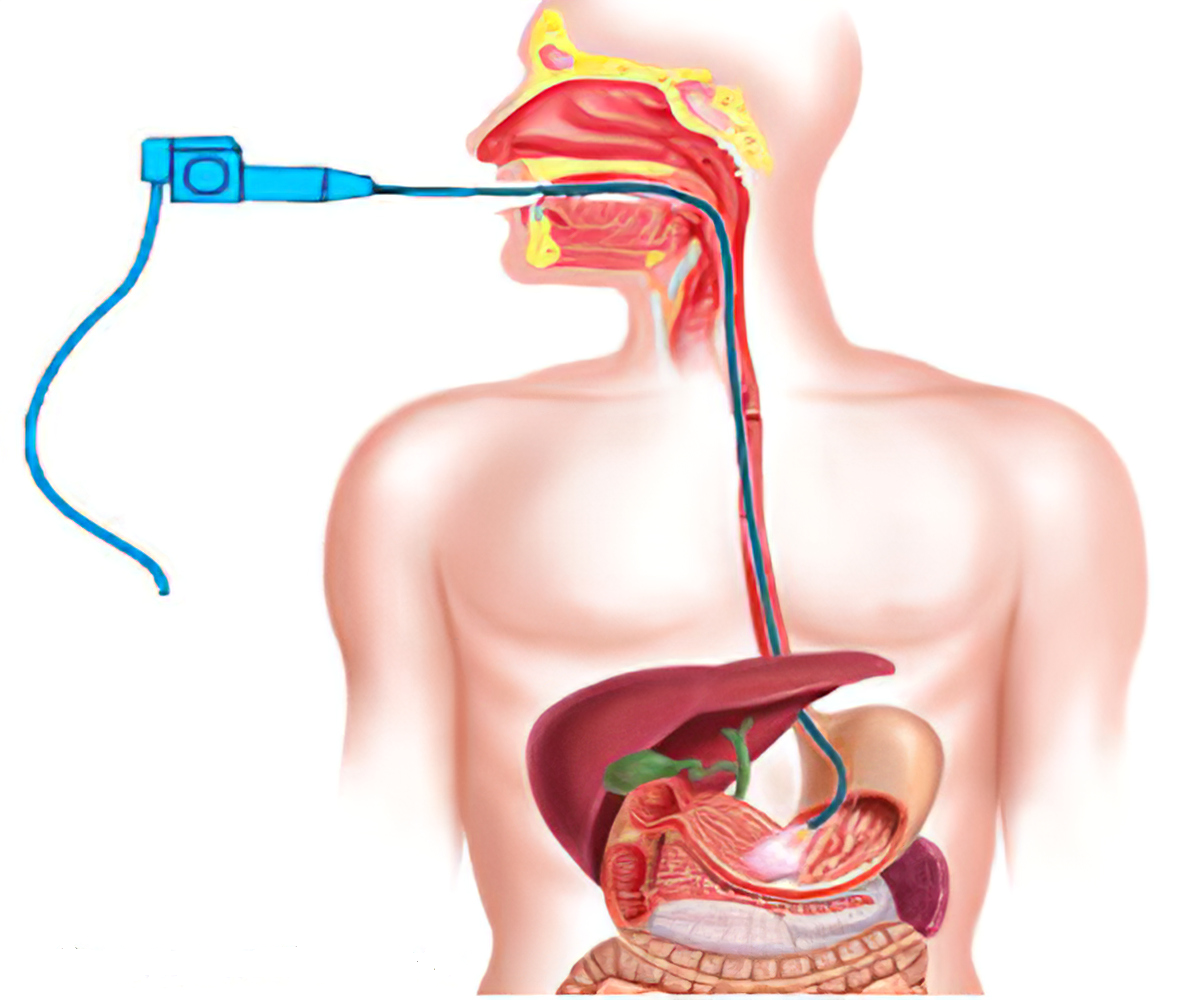
- Upper endoscopy, or EGD, a test used to diagnose the cause of abdominal pain or prolonged symptoms by enabling your healthcare provider to view the lining of the duodenum and check for the presence of ulcers or other symptoms, such as inflammation or bleeding
- A biopsy to check for cancer cells or to diagnose duodenal lymphocytosis
When to see a doctor
The duodenum is a key organ in digestion, and symptoms may suggest a health condition that requires treatment. See your healthcare provider for diagnosis and treatment when you face any of the above mentioned symptoms.
Reference
- https://www.cancer.gov/publications/dictionaries/cancer-terms/def/duodenum
- https://www.britannica.com/science/duodenum
- https://medlineplus.gov/ency/article/002347.htm
- https://emedicine.medscape.com/article/1898874-overview
- https://www.ncbi.nlm.nih.gov/books/NBK482390/
- https://www.sciencedirect.com/topics/medicine-and-dentistry/duodenum