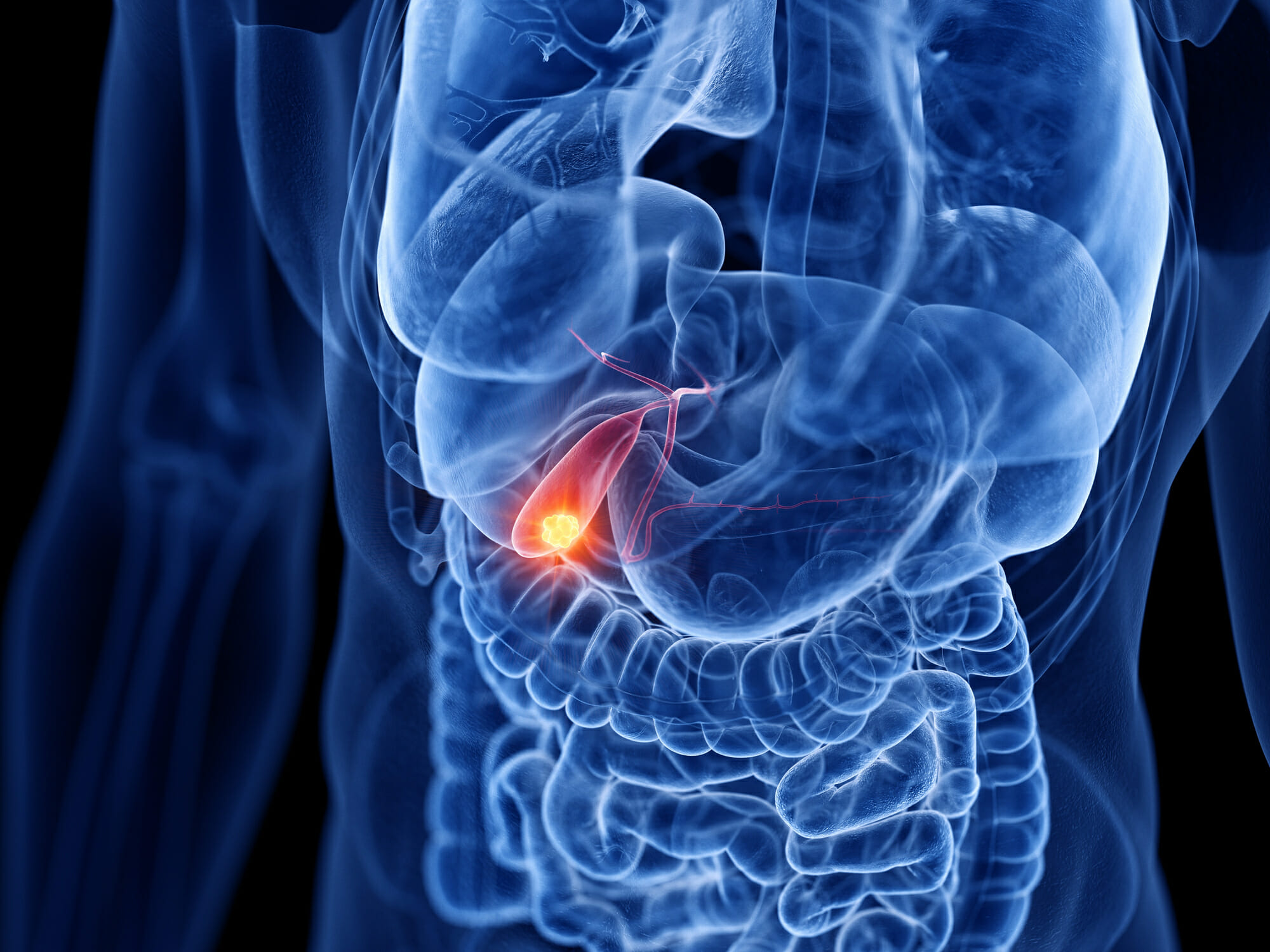
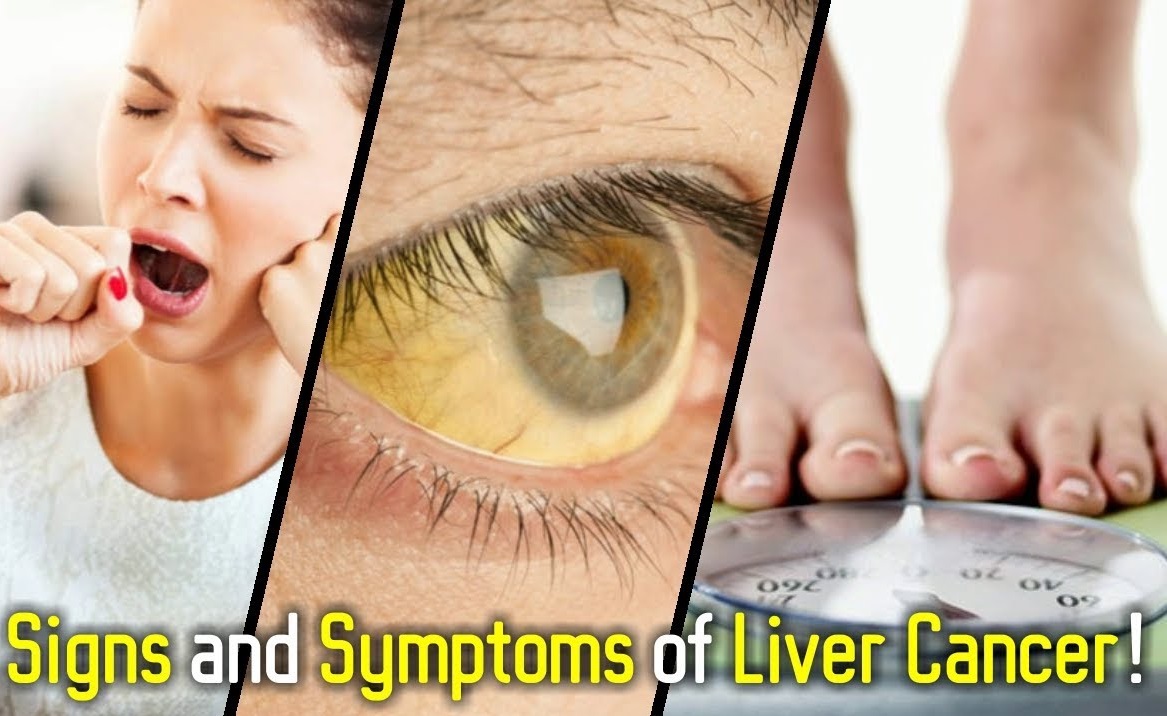
Liver Cancer
Liver Cancer- Things to know prior to Liver Cancer Surgery
When diagnosed with liver cancer, your doctor will suggest different treatment options depending upon the tumor’s size, location and other factors
This guide will help you learn more about liver cancer surgery. It will also help you understand what to expect during your recovery.

Overview
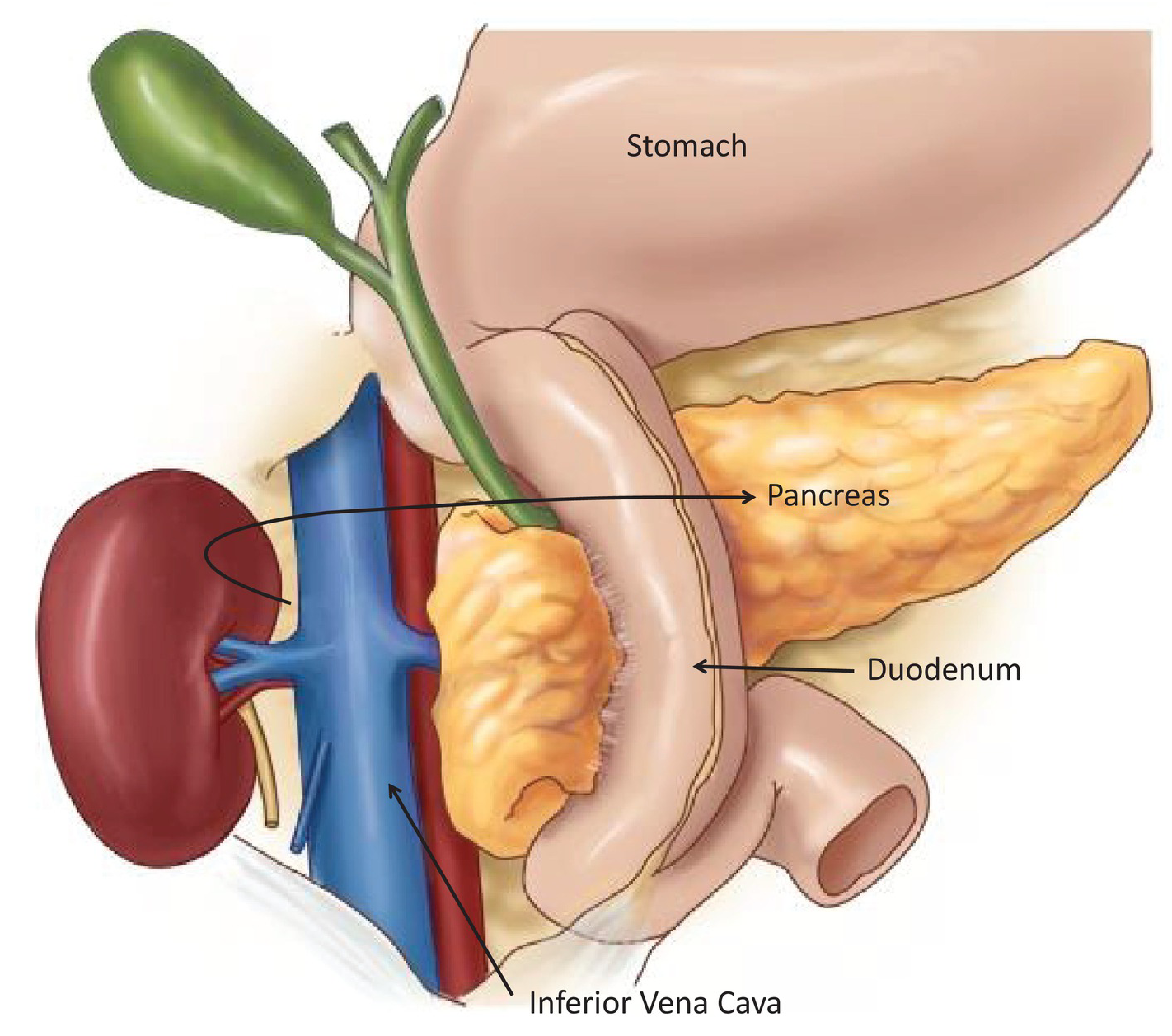
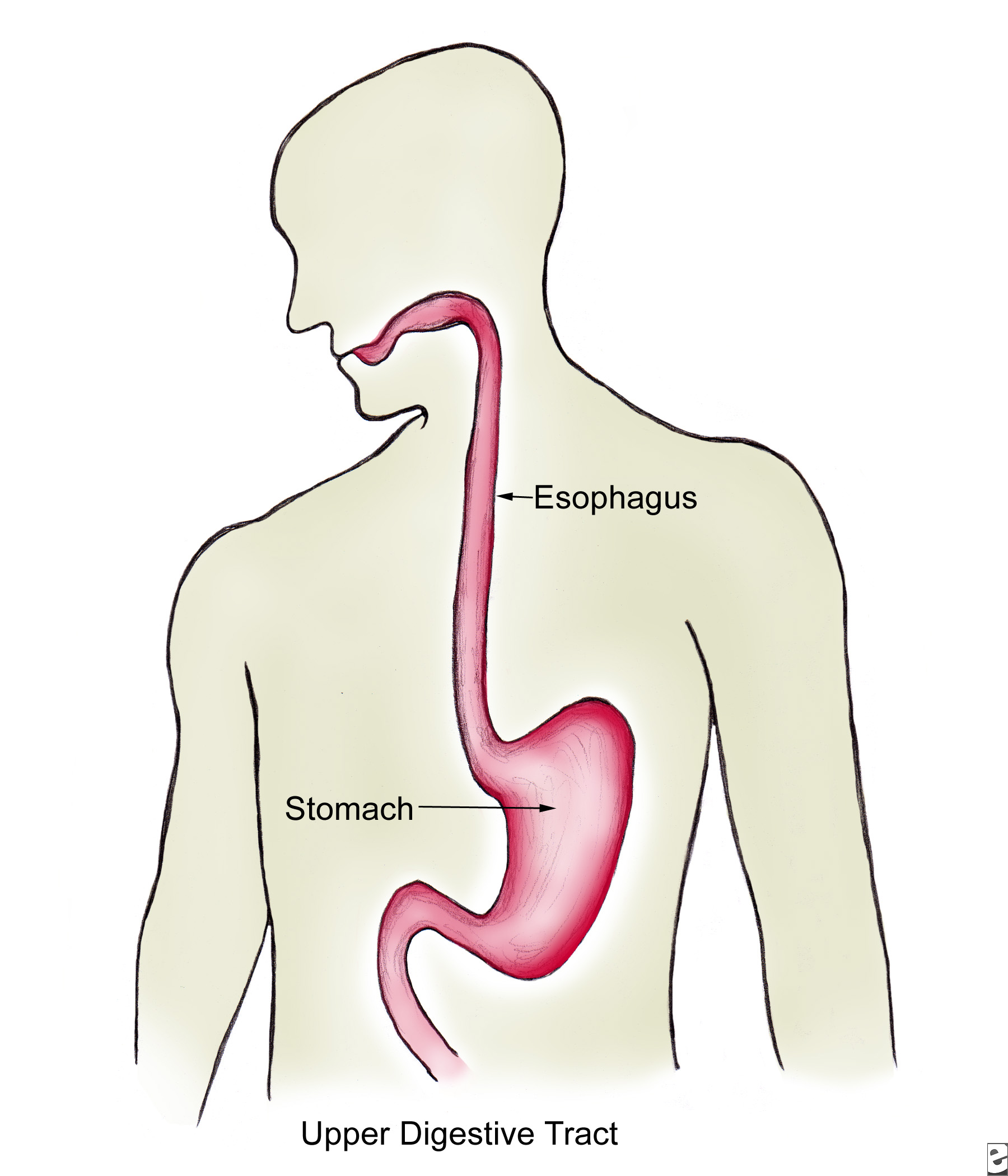
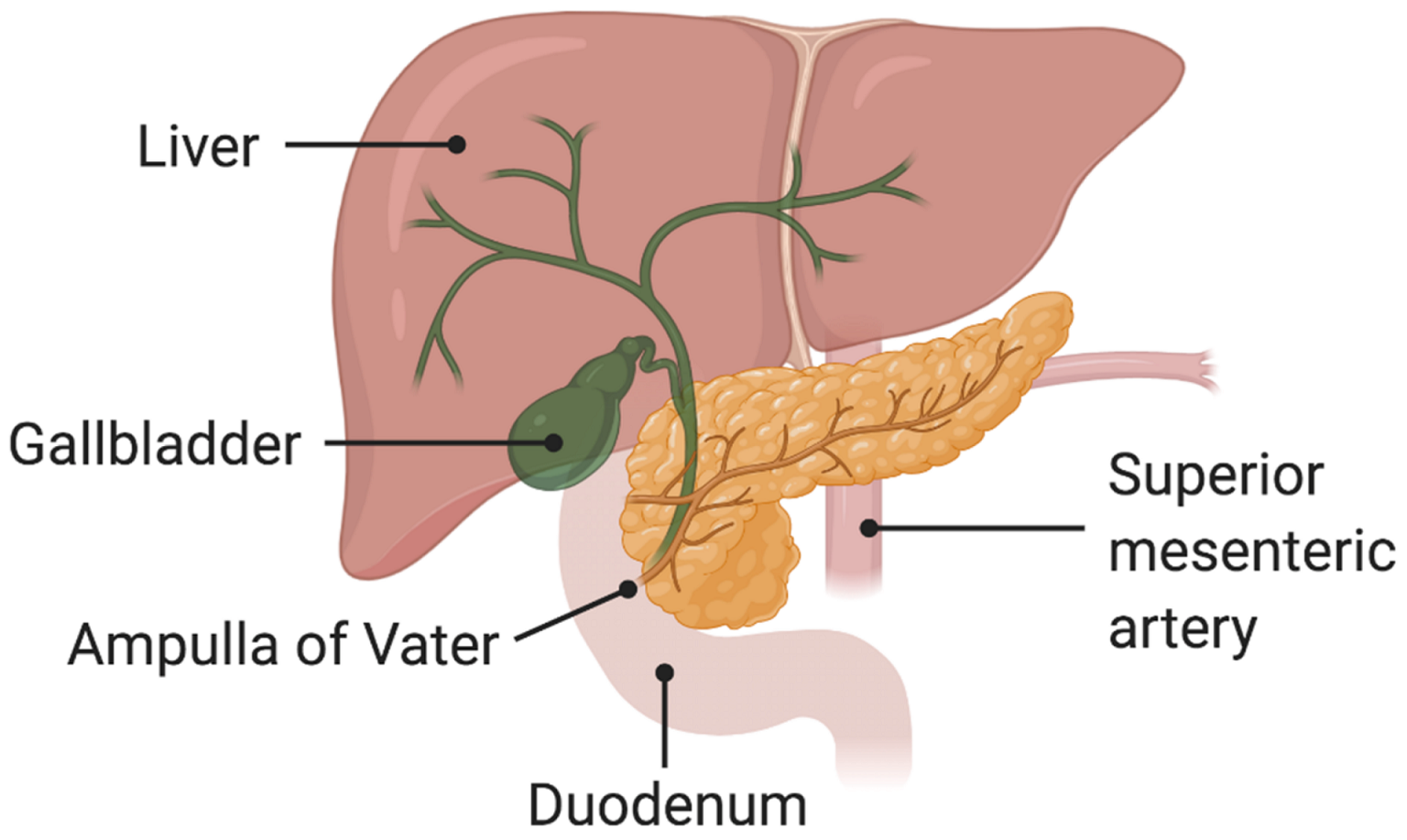
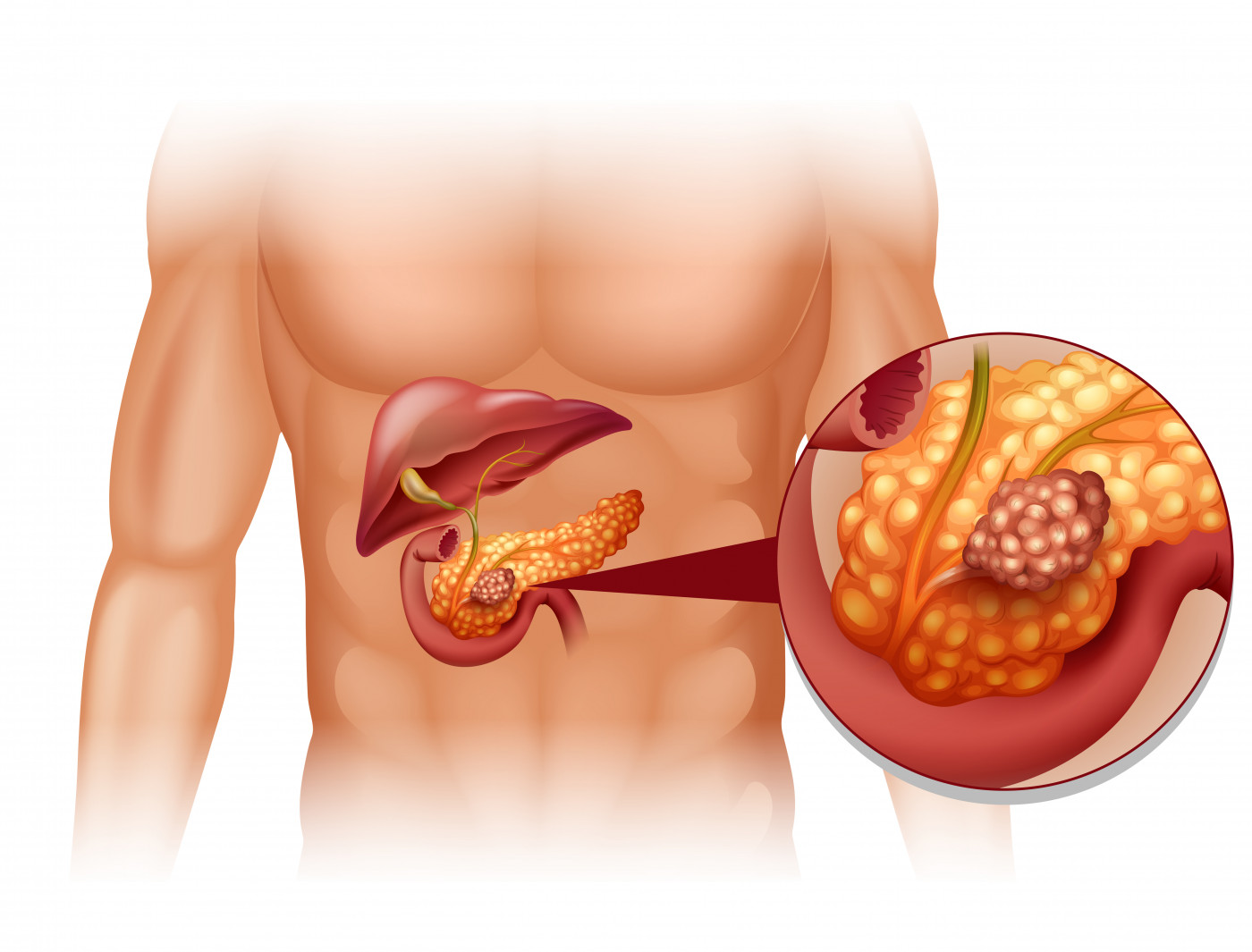
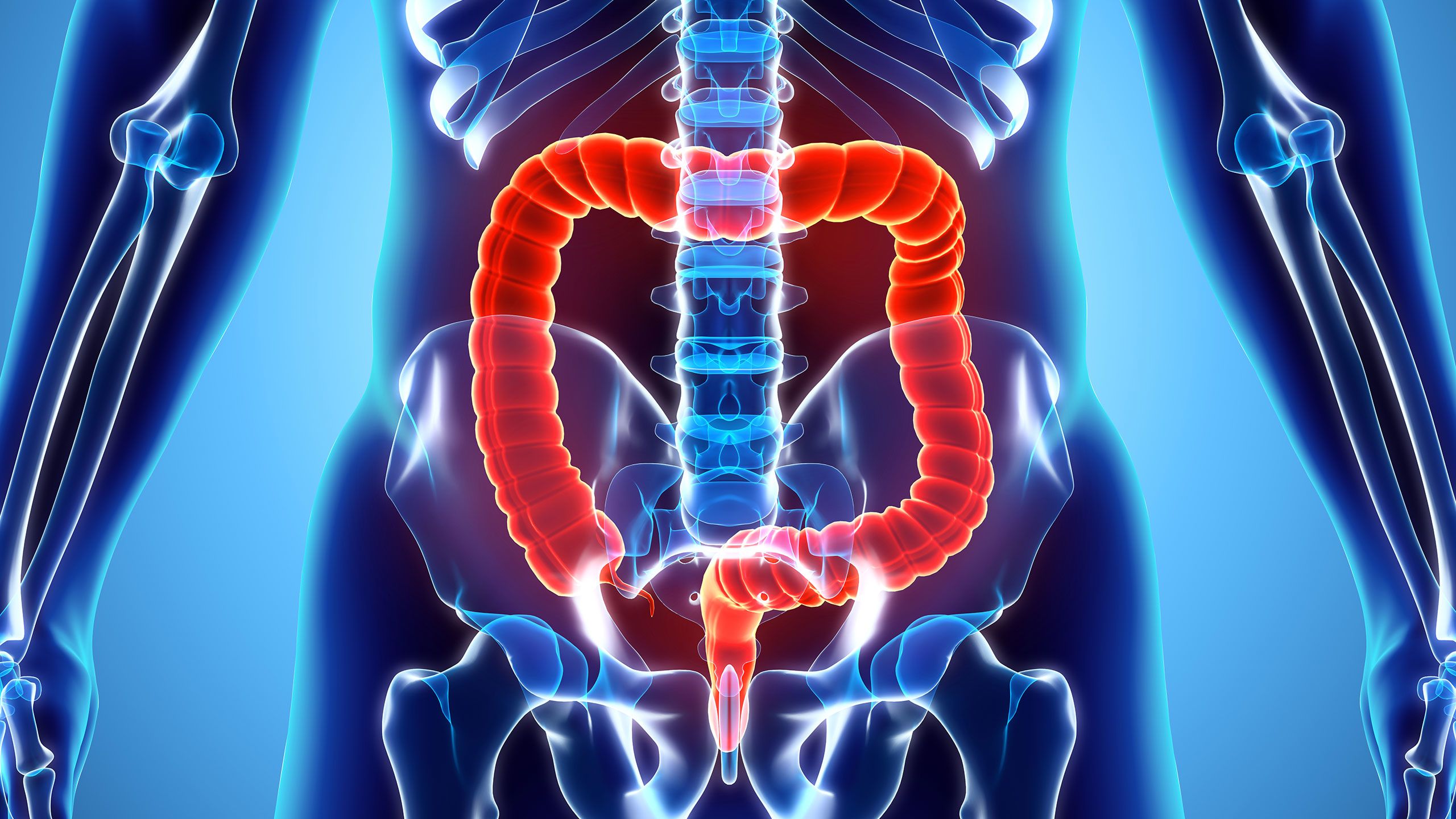
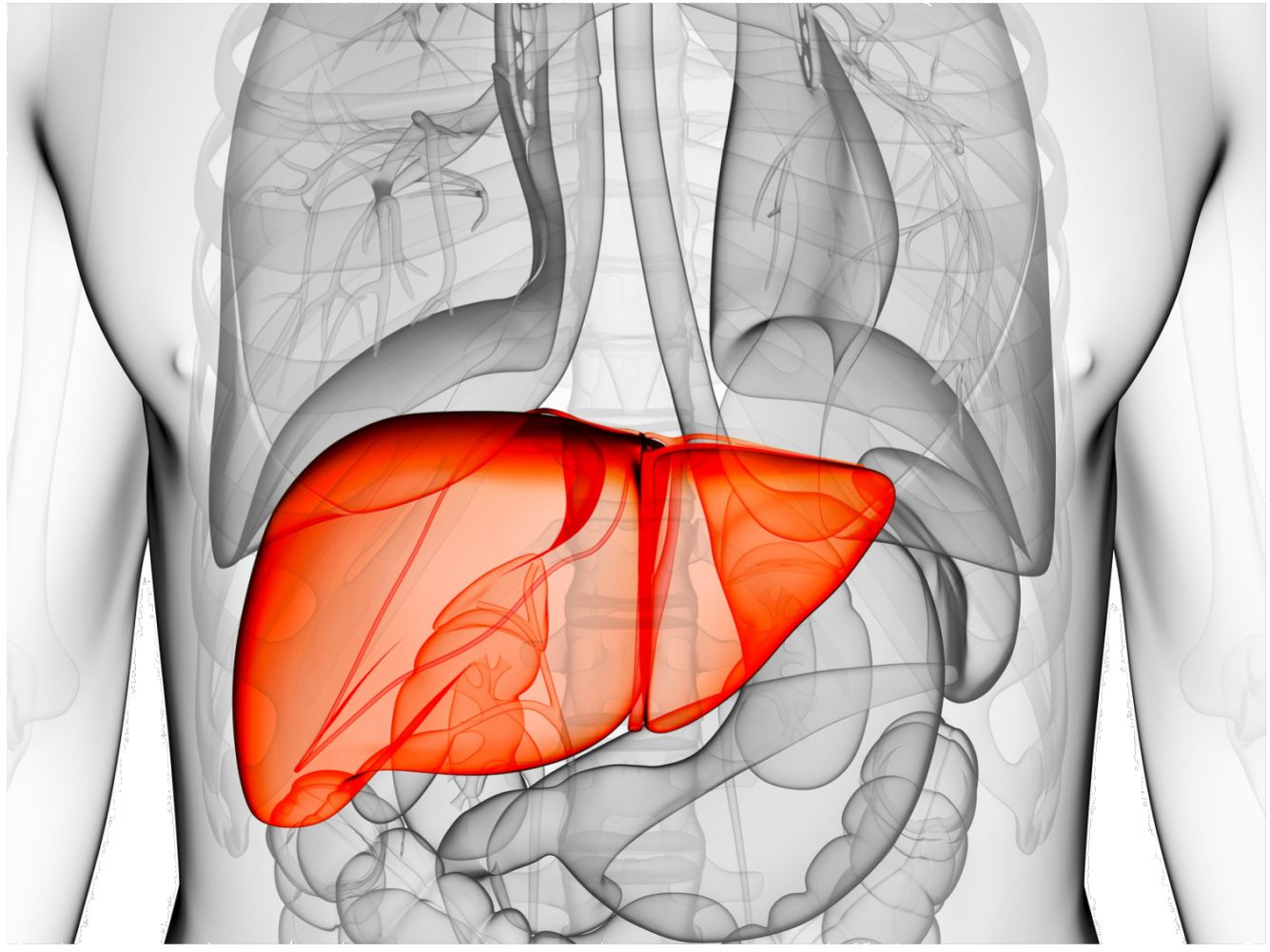
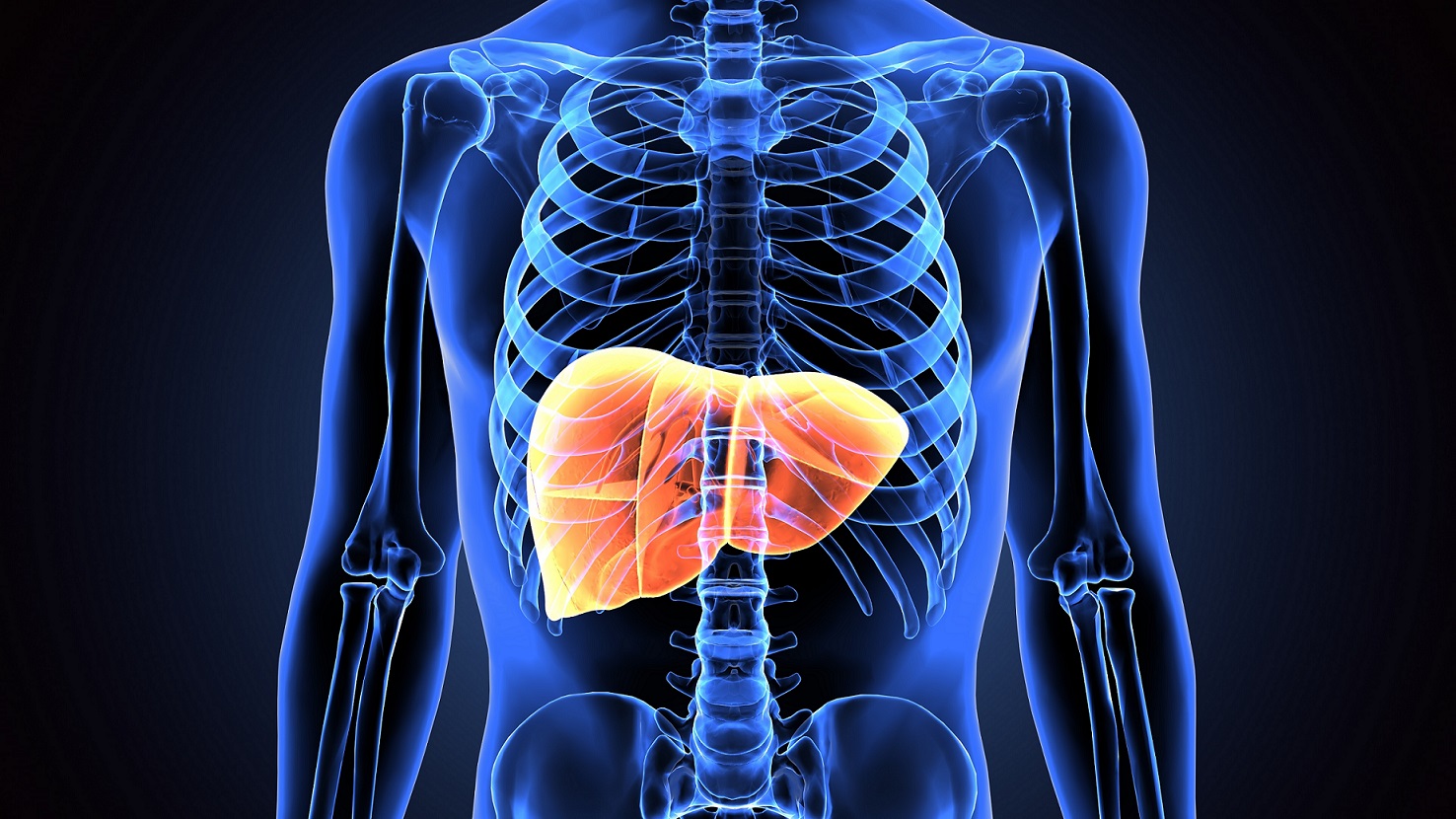
Your liver is a large organ located on the right side of your body, just under your ribs. Your liver has many functions, including:
- Storing and filtering blood.
- Making bile, which helps with digestion (the breakdown of food), especially of protein and fat.
- Changing sugar into a form your body can use for energy.
- Helping your body get rid of waste products.
- Making the substances that your blood needs to clot.
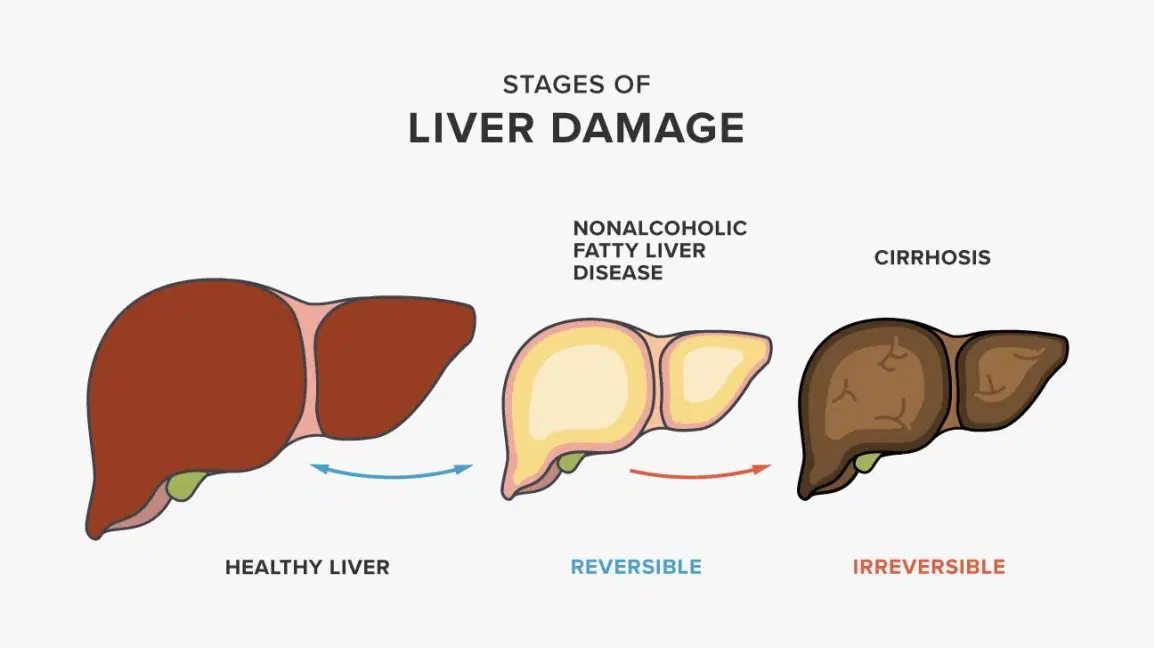
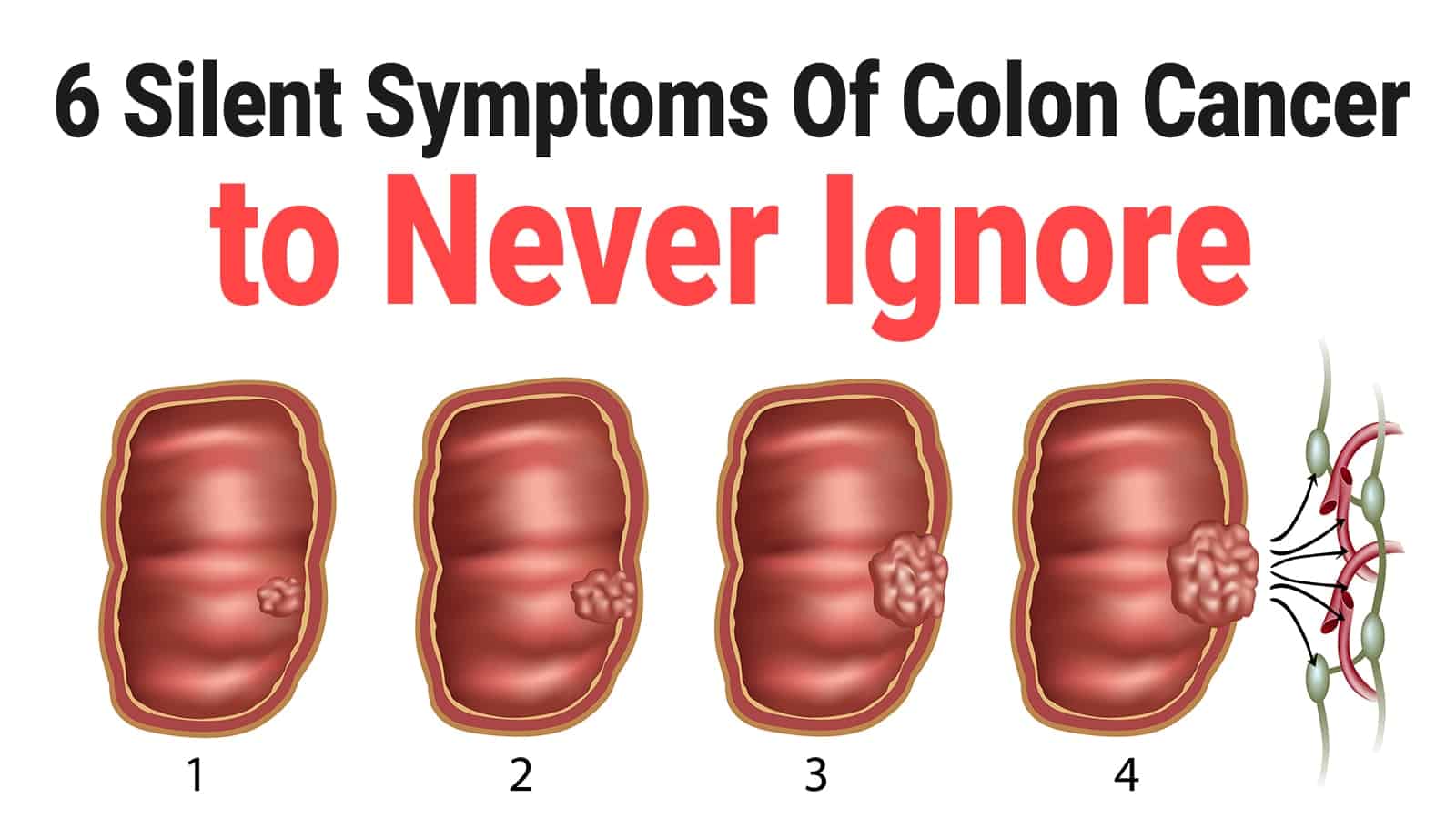
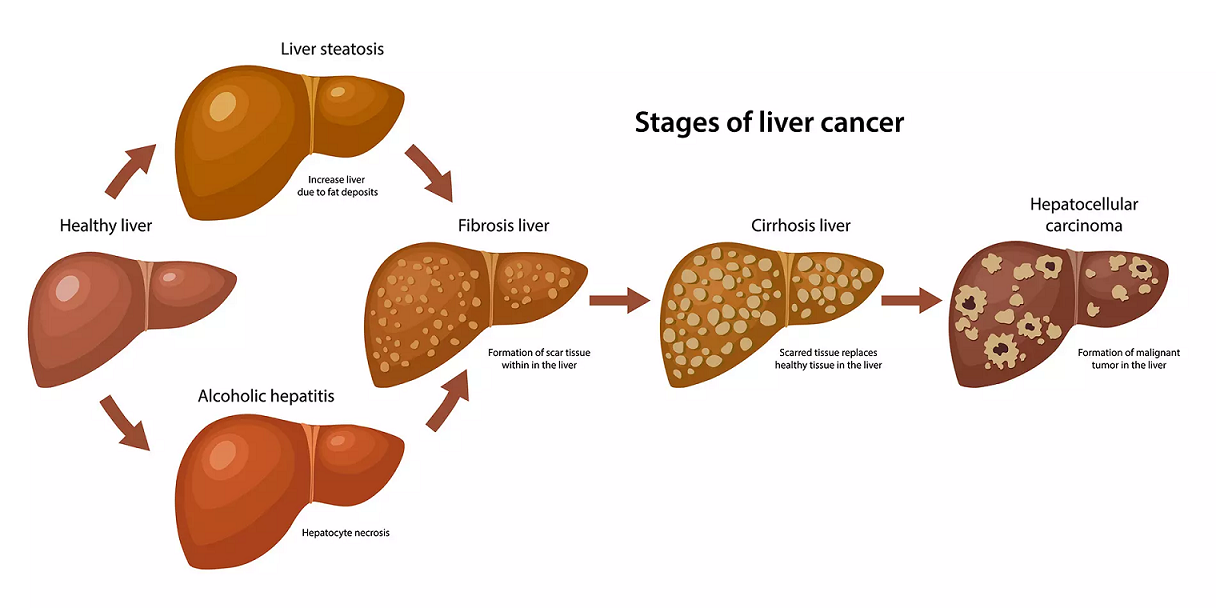
Most primary liver cancers begin in hepatocytes (liver cells). This type of cancer is called hepatocellular carcinoma or malignant hepatoma.
Liver cancer cells can spread by breaking away from the original tumor. They mainly spread by entering blood vessels, but liver cancer cells can also be found in lymph nodes. The cancer cells may attach to other tissues and grow to form new tumors that may damage those tissues.
Learn about liver cancer surgery
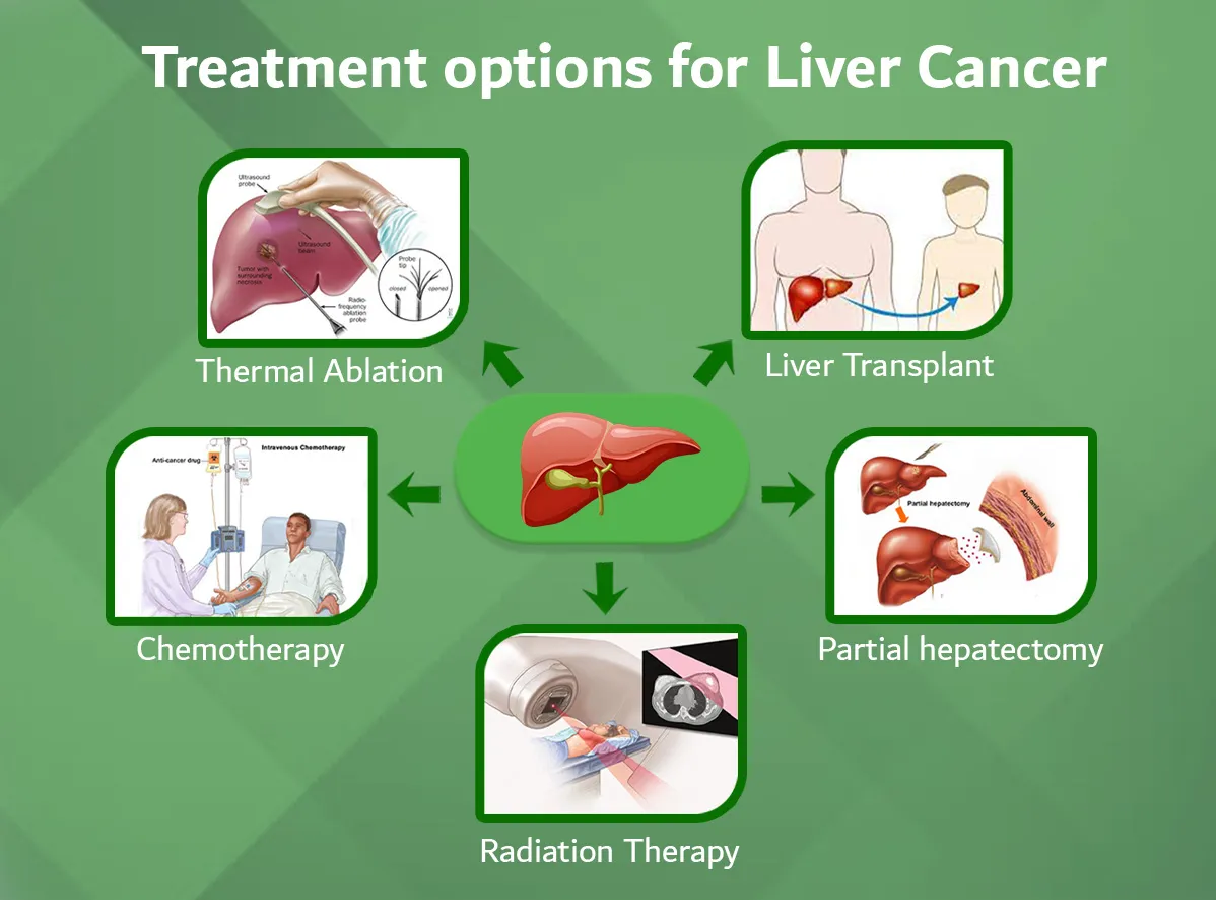
Treatment options for people with liver cancer are surgery (including a liver transplant), ablation, embolization, targeted therapy, radiation therapy, and chemotherapy. You may have a combination of treatments.
Surgery
Surgery is an option for people with an early stage of liver cancer. The surgeon may remove the whole liver or only the part that has cancer. If the whole liver is removed, it's replaced with healthy liver tissue from a donor.
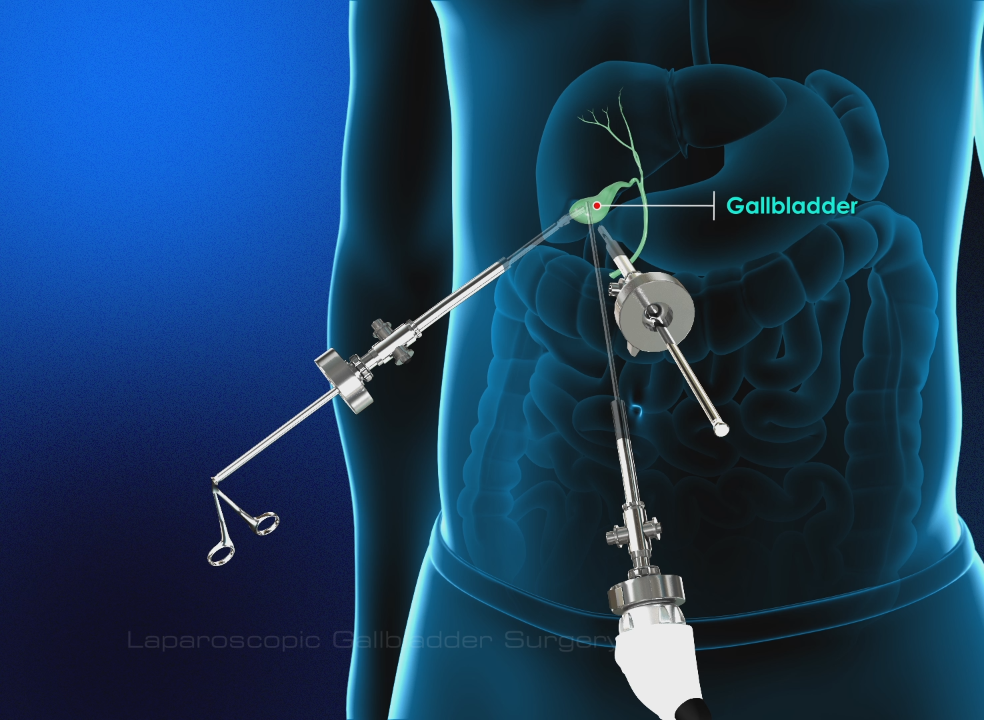
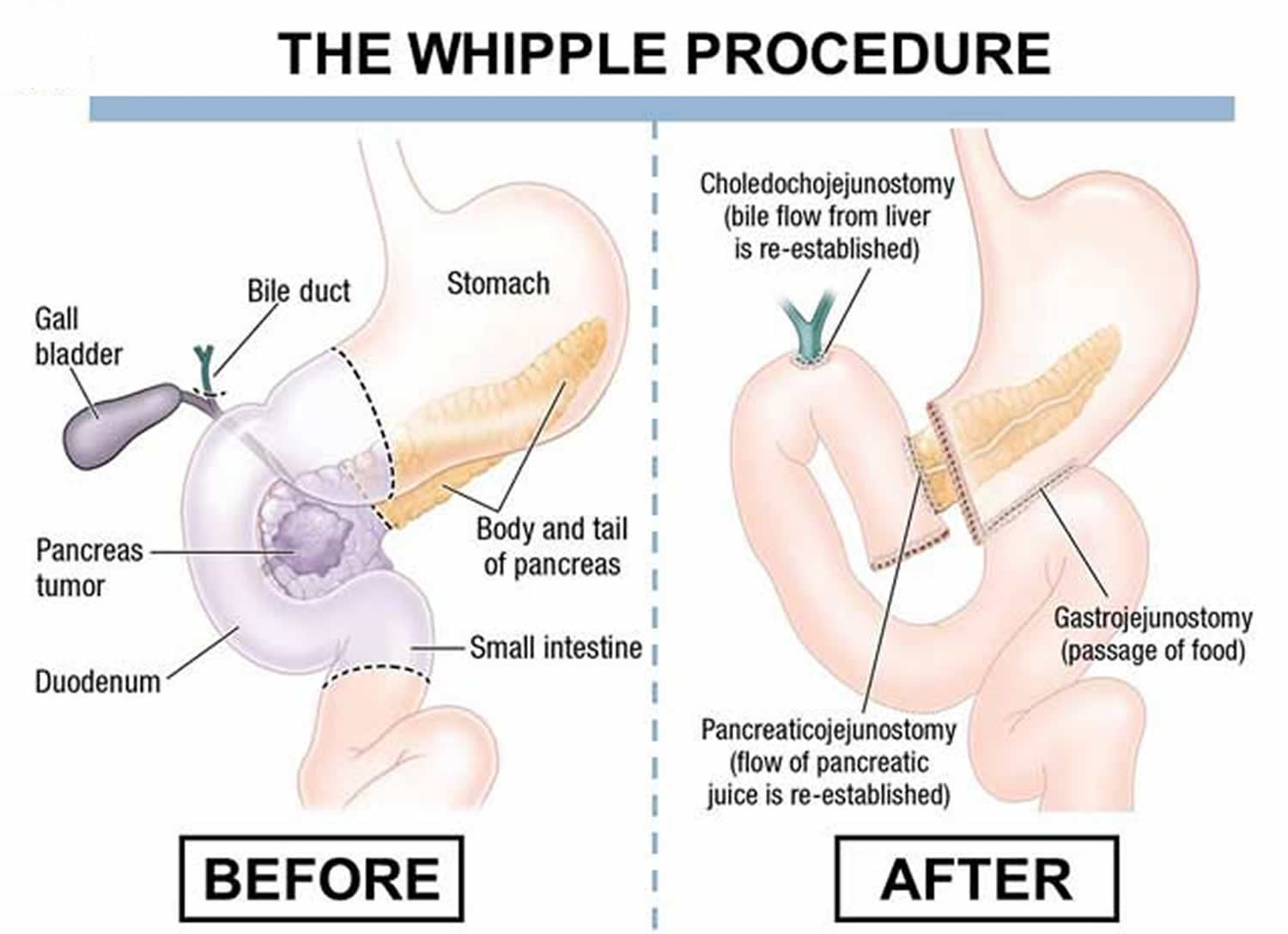
Removal of part of the liver (Hepatectomy)
Surgery to remove part of the liver is called partial hepatectomy. A person with liver cancer may have part of the liver removed if lab tests show that the liver is working well and if there is no evidence that the cancer has spread to nearby lymph nodes or to other parts of the body.
The surgeon removes the tumor along with a margin of normal liver tissue around the tumor. The extent of the surgery depends on the size, number, and location of the tumors. It also depends on how well the liver is working.
As much as 80 percent of the liver may be removed. The surgeon leaves behind normal liver tissue. The remaining healthy tissue takes over the work of the liver. Also, the liver can regrow the missing part. The new cells grow over several weeks.
Liver transplant
A liver transplant is an option if the tumors are small, the disease has not spread outside the liver, and suitable donated liver tissue can be found.
Donated liver tissue comes from a deceased person or a live donor. If the donor is living, the tissue is part of a liver, rather than a whole liver.
While you wait for donated liver tissue to become available, the health care team monitors your health and provides other treatments.
When healthy liver tissue from a donor is available, the transplant surgeon removes your entire liver (total hepatectomy) and replaces it with the donated tissue. After surgery, your health care team will give you medicine to help control your pain. You may need to stay in the hospital for several weeks. During that time, your health care team monitors how well your body is accepting the new liver tissue. You'll take medicine to prevent your body's immune system from rejecting the new liver.
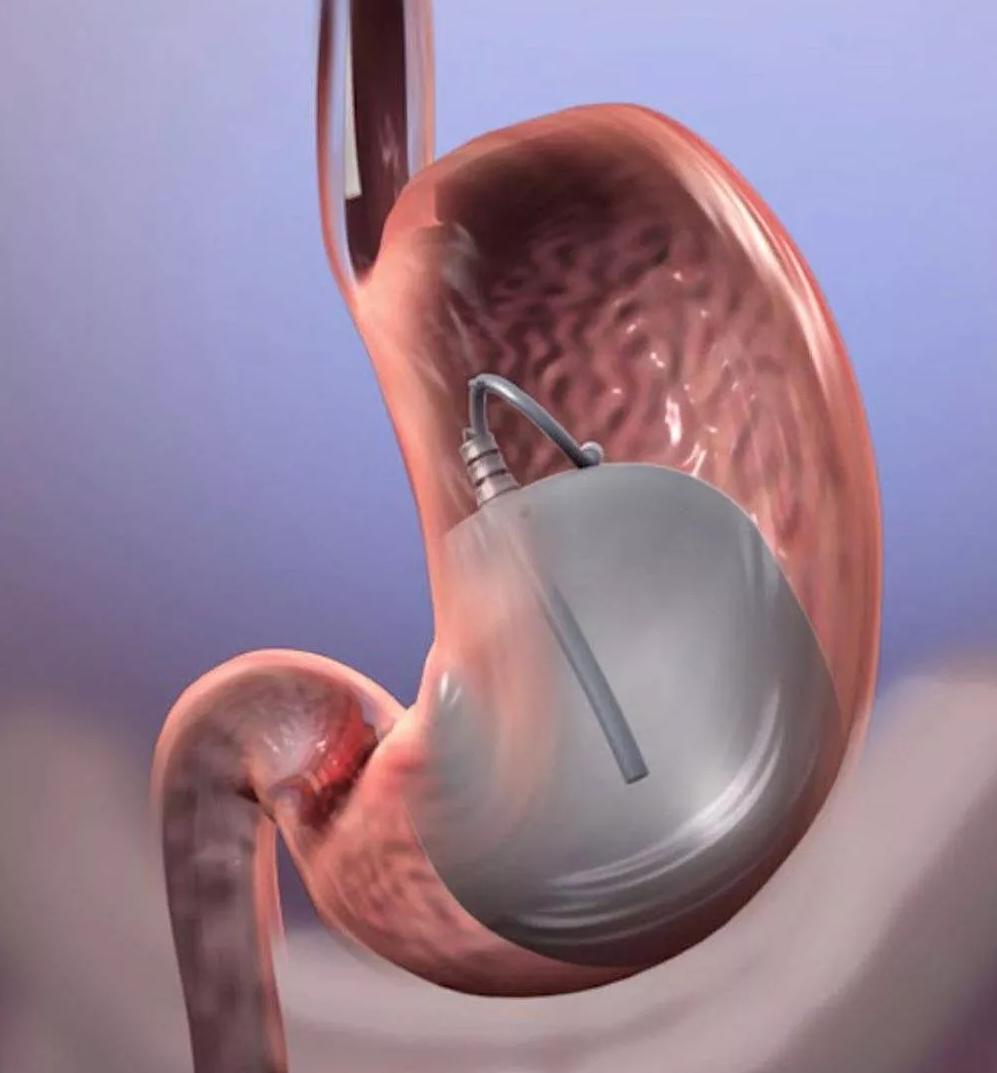
Ablation
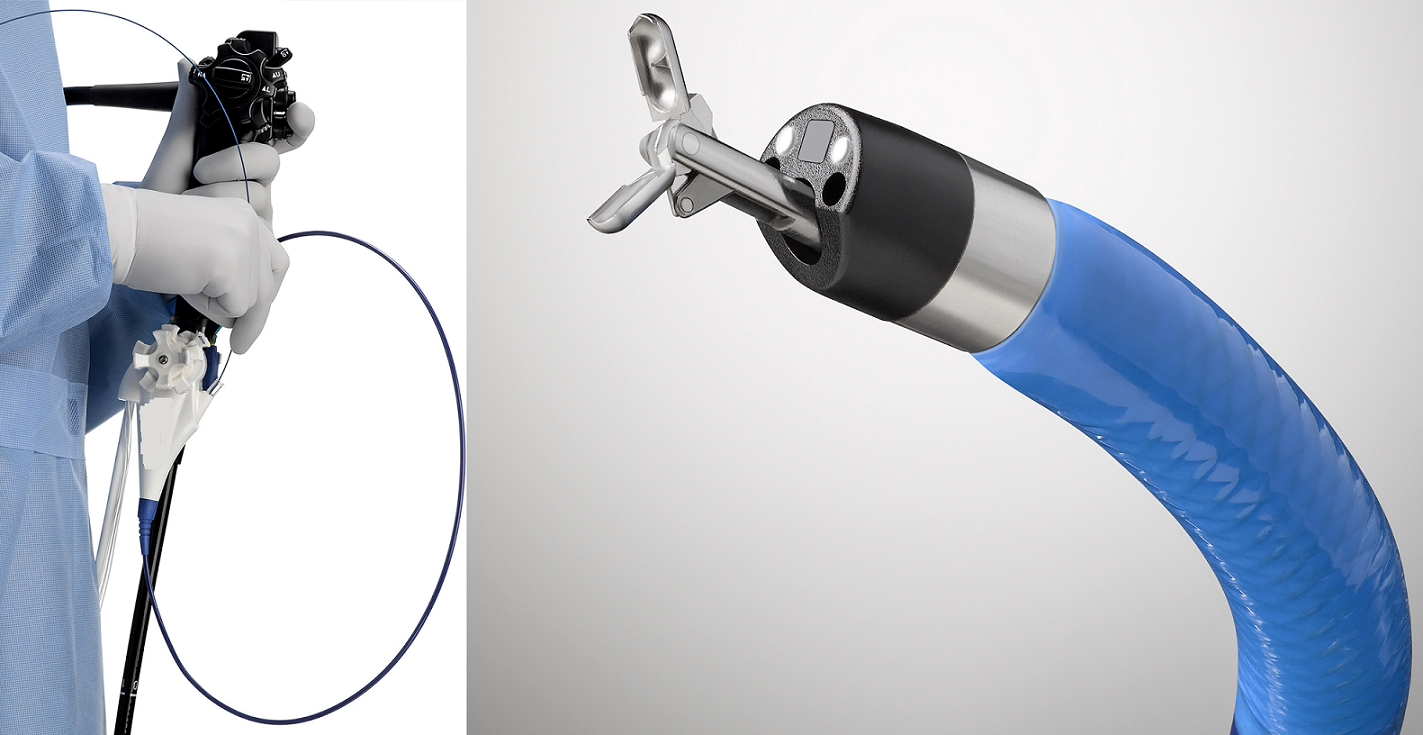
Methods of ablation destroy the cancer in the liver. They are treatments to control liver cancer and extend life. This may be used for people who can't have surgery or a liver transplant or for people waiting for a liver transplant . Surgery to remove the tumor may not be possible because of cirrhosis or other conditions that cause poor liver function, the location of the tumor within the liver, or other health problems.
Methods of ablation include the following:
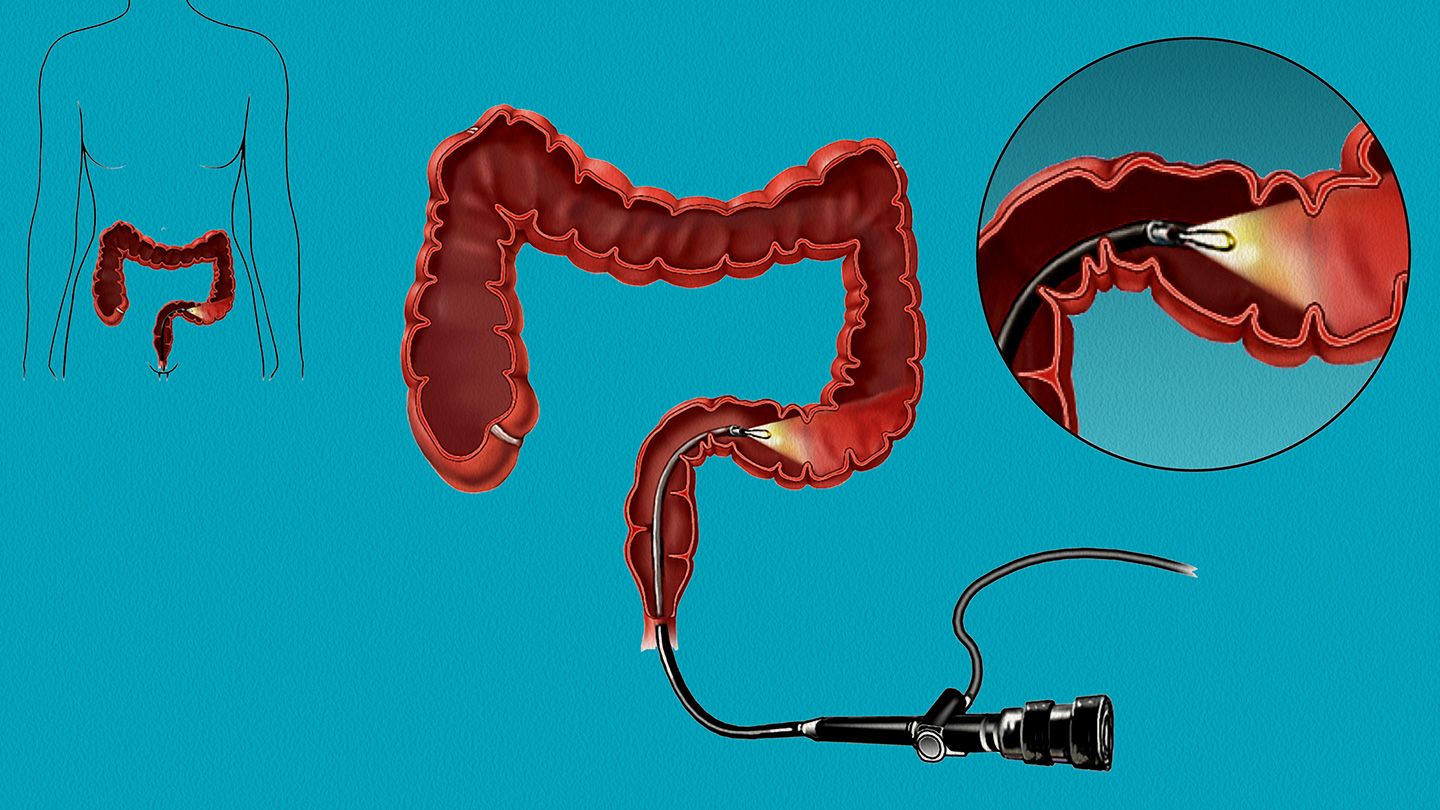
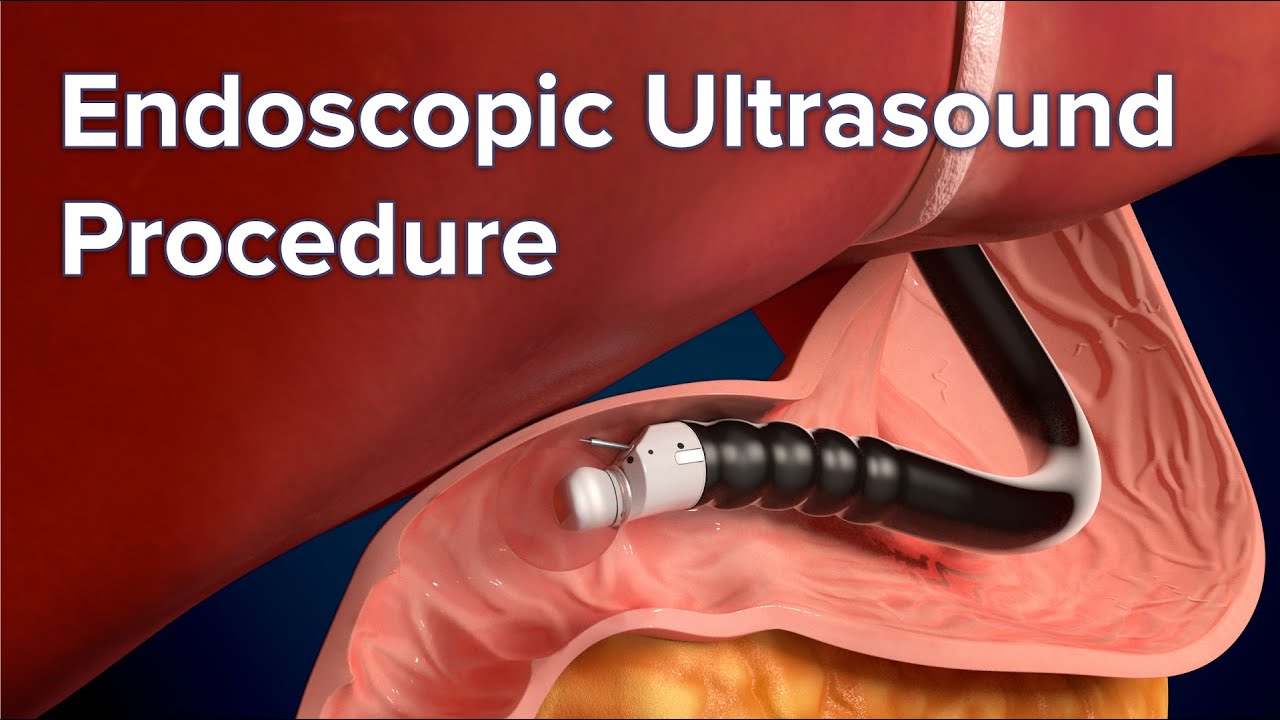
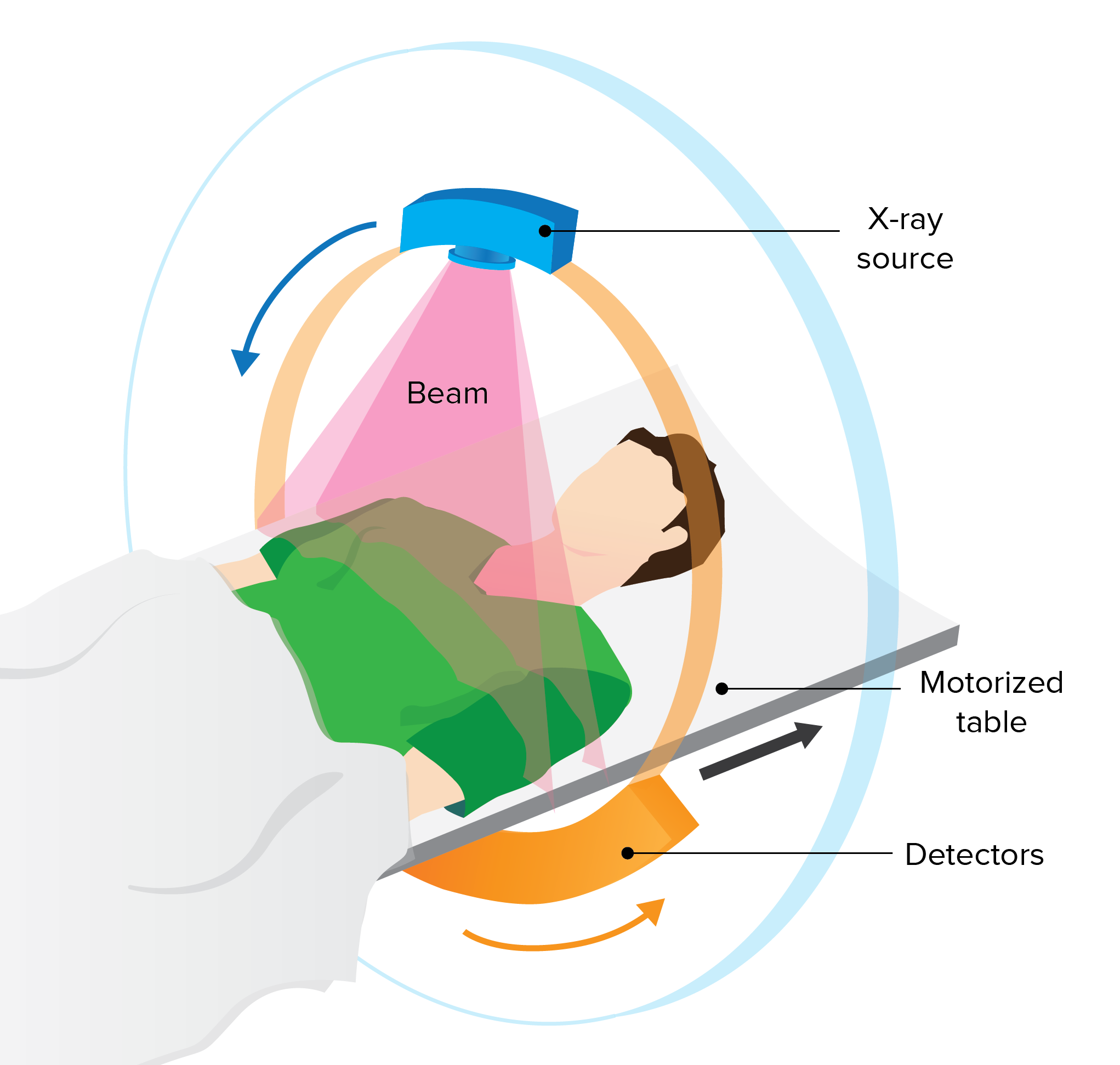
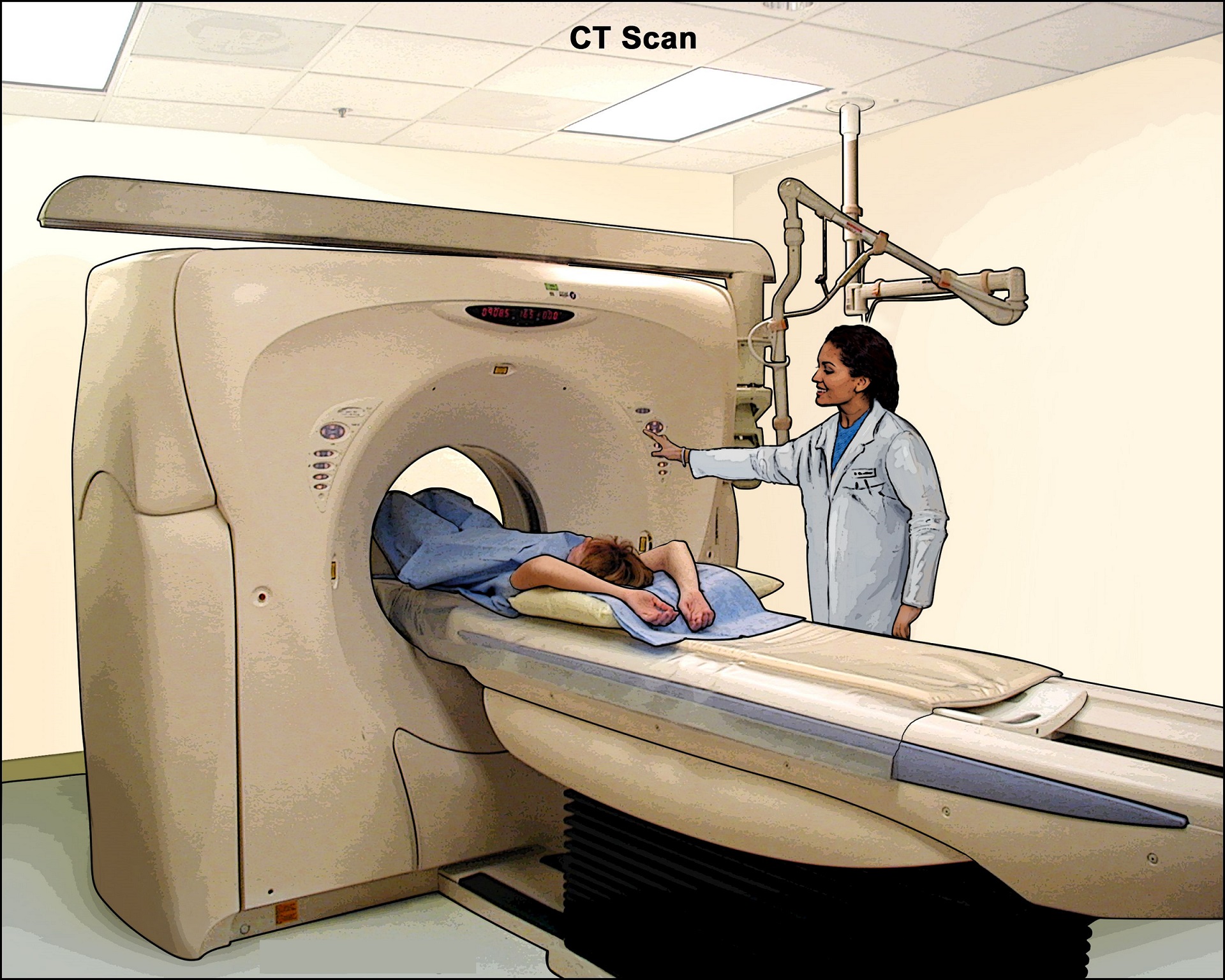
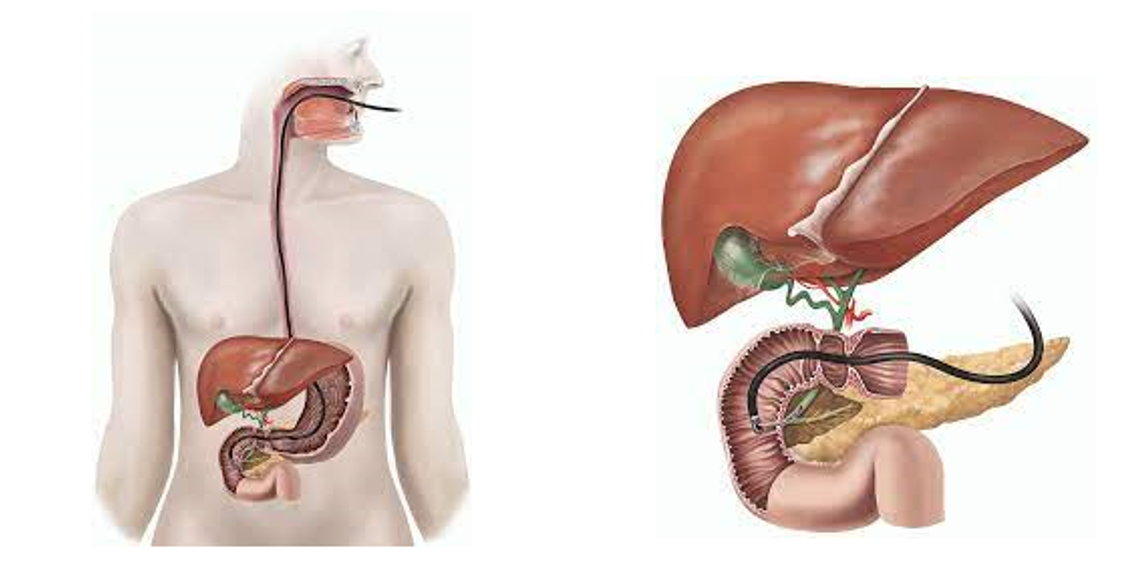
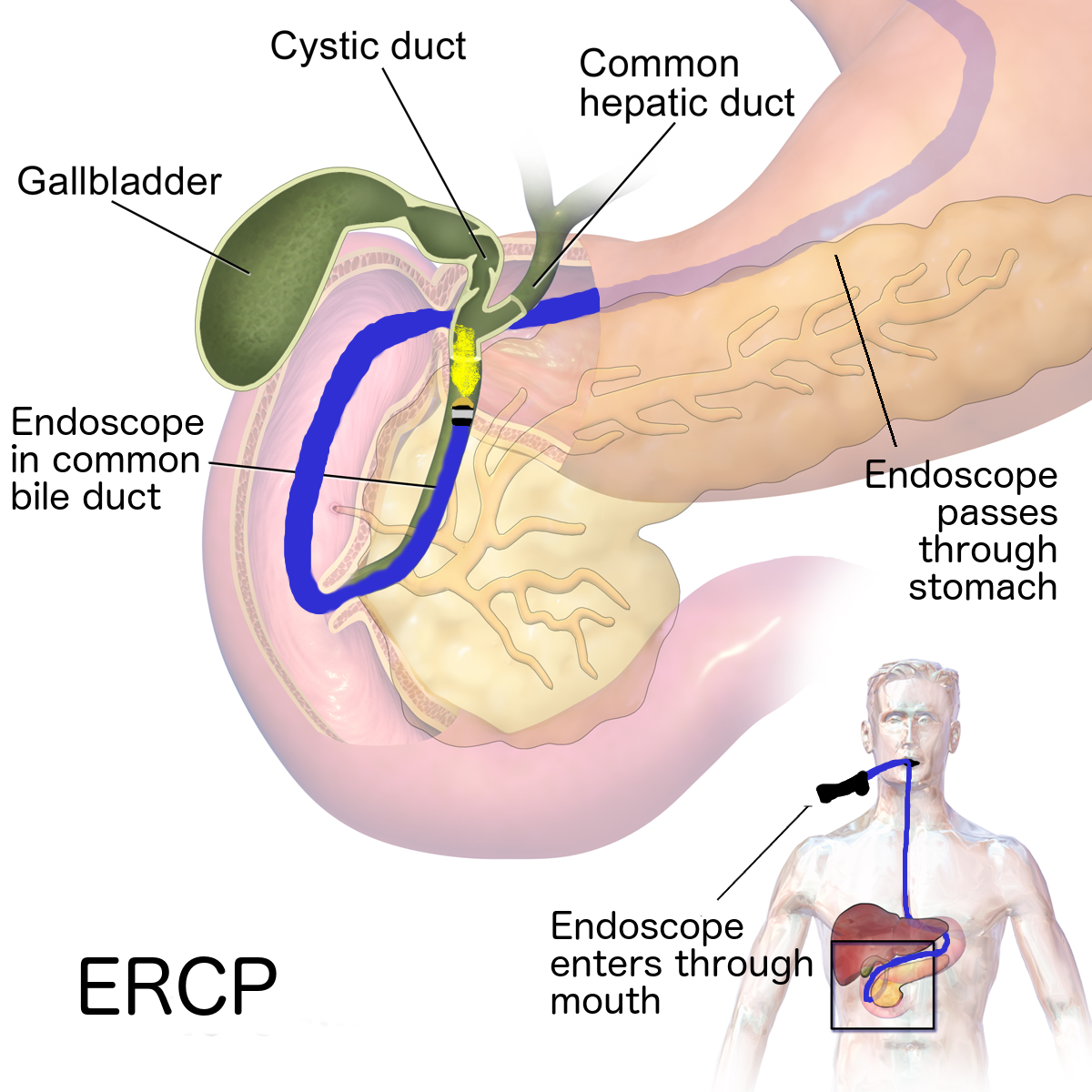
- Radiofrequency ablation: The doctor uses a special probe that contains tiny electrodes to kill the cancer cells with heat. Ultrasound, CT, or MRI may be used to guide the probe to the tumor. Usually, the doctor can insert the probe directly through your skin, and only local anesthesia is needed. Sometimes, surgery under general anesthesia is needed. The doctor inserts the probe through a small incision in your abdomen (using a laparoscope) or through a wider incision that opens your abdomen.Some people have pain or a slight fever after this procedure. Staying overnight in the hospital is not usually needed. Radiofrequency ablation is a type of hyperthermia therapy. Other therapies that use heat to destroy liver tumors include laser or microwave therapy. They are used less often than radiofrequency ablation.
- Percutaneous ethanol injection: The doctor uses ultrasound to guide a thin needle into the liver tumor. Alcohol (ethanol) is injected directly into the tumor and kills cancer cells. The procedure may be performed once or twice a week. Usually local anesthesia is used, but if you have many tumors in the liver, general anesthesia may be needed. You may have fever and pain after the injection.
Embolization
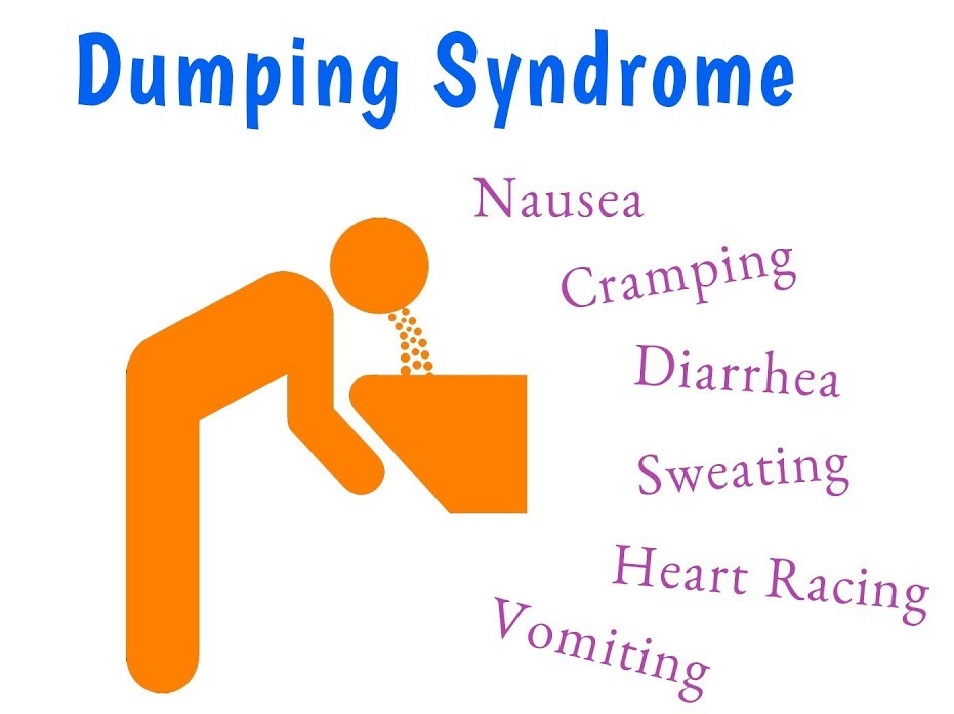
For those who can't have surgery or a liver transplant, embolization or chemoembolization may be an option. The doctor inserts a tiny catheter into an artery in your leg and moves the catheter into the hepatic artery. For embolization, the doctor injects tiny sponges or other particles into the catheter. The particles block the flow of blood through the artery. Depending on the type of particles used, the blockage may be temporary or permanent. Without blood flow from the hepatic artery, the tumor dies. Although the hepatic artery is blocked, healthy liver tissue continues to receive blood from the hepatic portal vein. For chemoembolization, the doctor injects an anticancer drug (chemotherapy) into the artery before injecting the tiny particles that block blood flow. Without blood flow, the drug stays in the liver longer. You'll need to be sedated for this procedure, but general anesthesia is not usually needed. You'll probably stay in the hospital for 2 to 3 days after the treatment. Embolization often causes abdominal pain, nausea, vomiting, and fever. Some people may feel very tired for several weeks after the treatment.
Targeted Therapy
People with liver cancer who can't have surgery or a liver transplant may receive a drug called targeted therapy. Sorafenib tablets were the first targeted therapy approved for liver cancer.Targeted therapy slows the growth of liver tumors. It also reduces their blood supply. The drug is taken by mouth. Side effects include nausea, vomiting, mouth sores, and loss of appetite. Sometimes, a person may have chest pain, bleeding problems, or blisters on the hands or feet. The drug can also cause high blood pressure. The health care team will check your blood pressure often during the first 6 weeks of treatment.
Radiation Therapy
Radiation therapy uses high-energy rays to kill cancer cells. It may be an option for a few people who can't have surgery. Sometimes it's used with other approaches. Radiation therapy also may be used to help relieve pain from liver cancer that has spread to the bones.
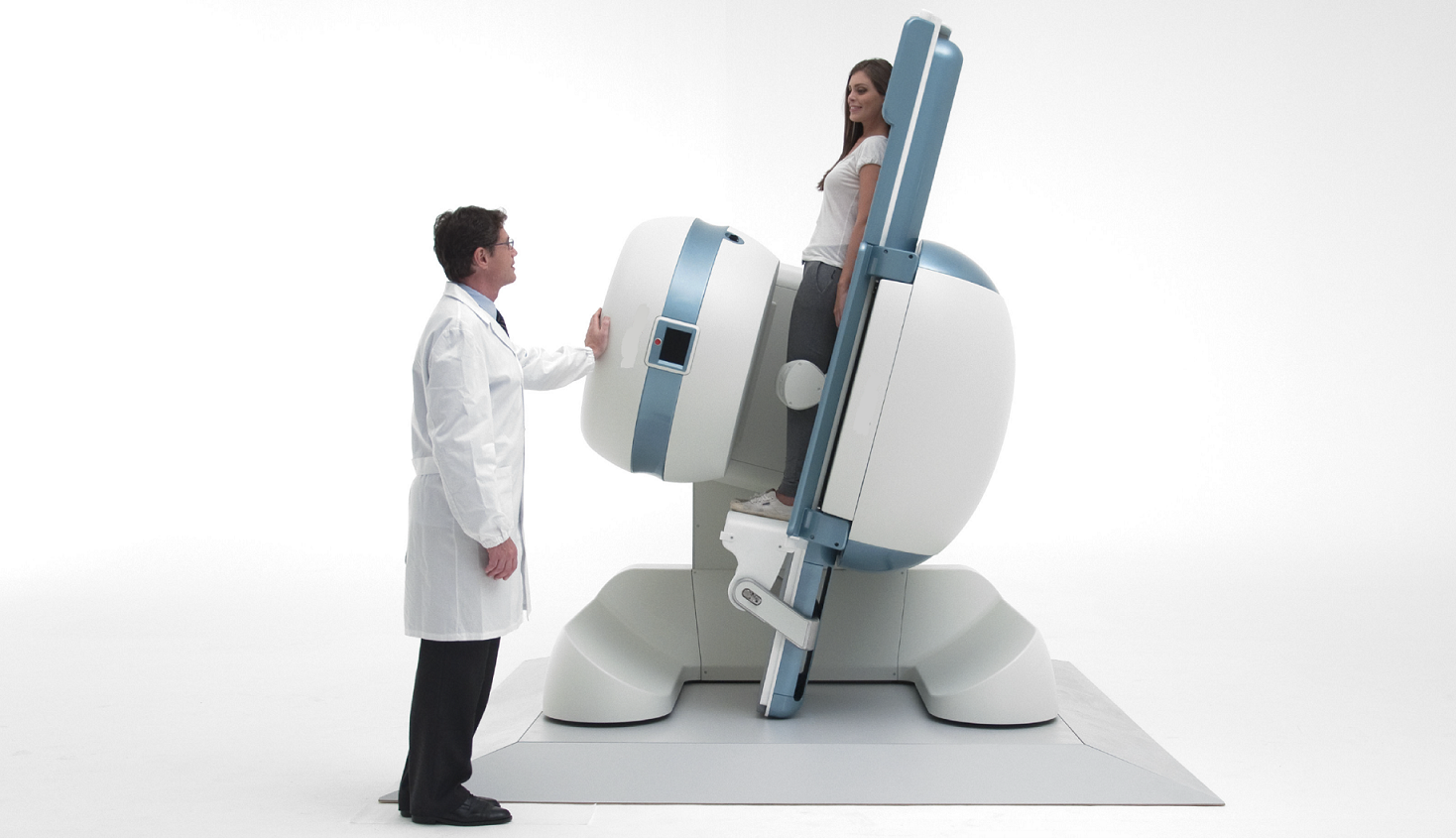
Doctors use two types of radiation therapy to treat liver cancer:
- External radiation therapy: The radiation comes from a large machine. The machine aims beams of radiation at the chest and abdomen.
- Internal radiation therapy: The radiation comes from tiny radioactive spheres. A doctor uses a catheter to inject the tiny spheres into your hepatic artery. The spheres destroy the blood supply to the liver tumor.
The side effects from radiation therapy include nausea, vomiting, or diarrhea. Your health care team can suggest ways to treat or control the side effects.
Chemotherapy
Chemotherapy, the use of drugs to kill cancer cells, is sometimes used to treat liver cancer. Drugs are usually given by vein (intravenous). The drugs enter the bloodstream and travel throughout your body. The side effects of chemotherapy depend mainly on which drugs are given and how much. Common side effects include nausea and vomiting, loss of appetite, headache, fever and chills, and weakness.
Some drugs lower the levels of healthy blood cells, and you're more likely to get infections, bruise or bleed easily, and feel very weak and tired. Your health care team will check for low levels of blood cells. Some side effects may be relieved with medicine.
RECOVERY FROM SURGERY
Your recovery right after surgery depends on many factors, including your state of health before the operation and how extensive the operation was performed.
Pain
You may feel pain at the site of surgery. We aim to keep you pain free after surgery with the help of latest and most effective technique or analgesic (pain relieving medicine).
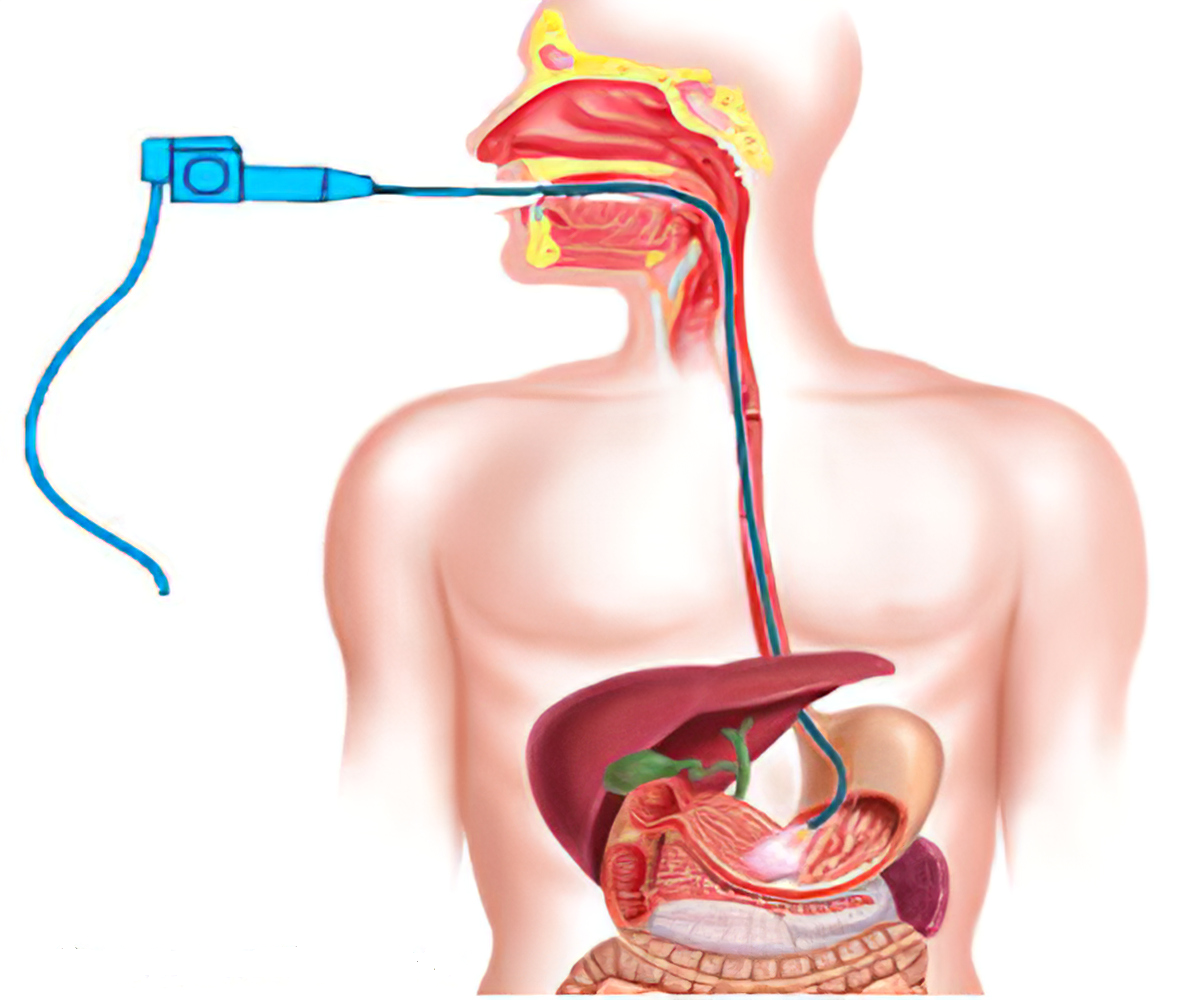
Tube/ Drains
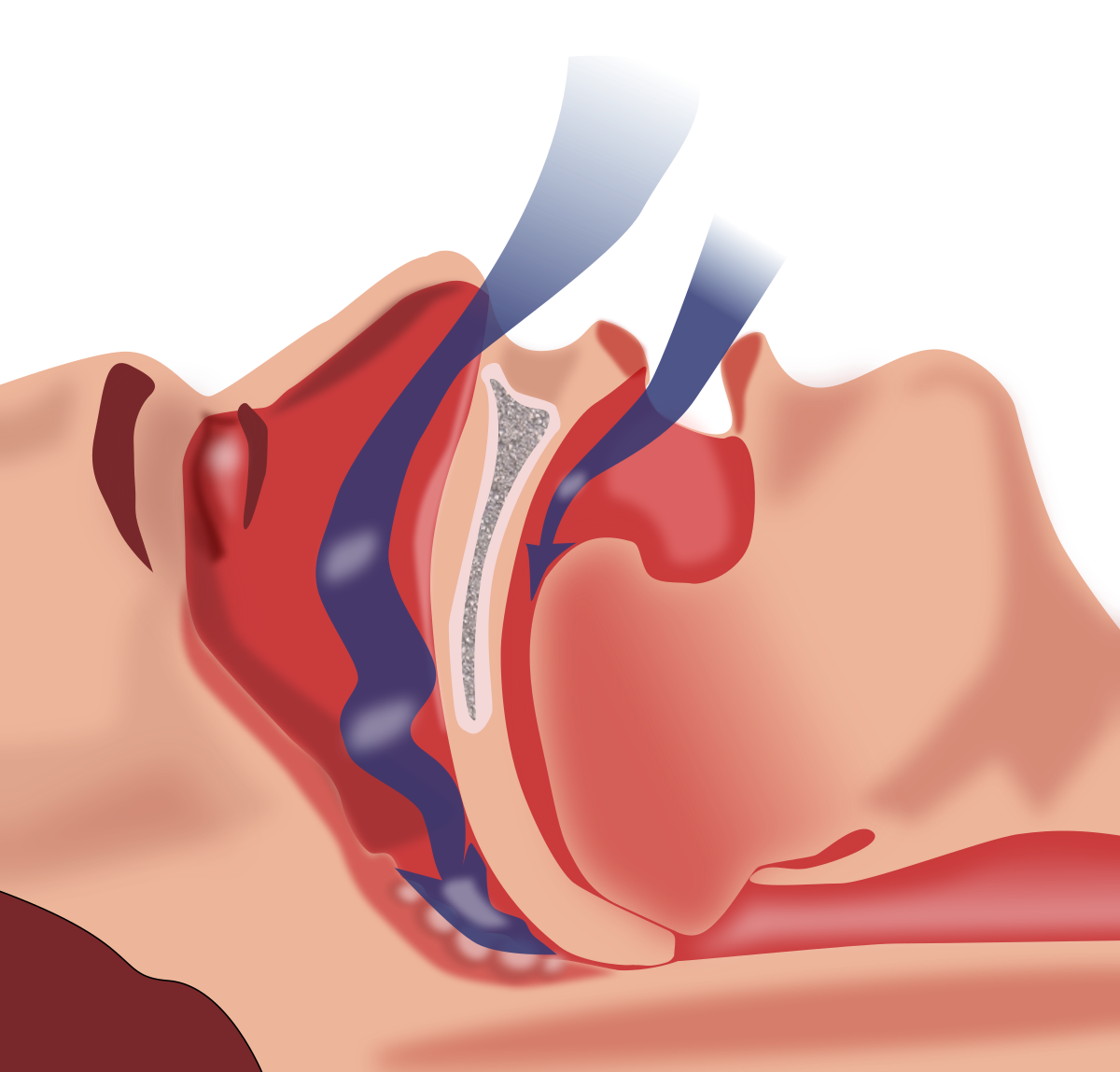
- You may also have Ryle’s Tube (tube going through nose to stomach) that drain out intestinal fluid. This tube helps to relieve nausea and vomiting after surgery and usually removed 1-2 day after surgery.
- You may also have “Tube” (called a Foley catheter) draining urine from your bladder into a bag. This will be taken out soon after surgery, once you are comfortable enough to go to bathroom.
- You may have a tube or tubes (called Drains) coming out of the surgical opening in your skin (incision site). Drains allow the excess fluid that collects at the surgery site to leave the body. Drain tube will also be removed once they stop collecting fluid, usually a few days after the operation.
Leg Stocking / Compression boot
As you are remains in bed on day of surgery, circulation of blood in leg become sluggish that may increase possibility of thrombo-embolism. To minimise it, you will be wearing leg stocking/ pneumatic compression boot to improve your leg circulation thus minimising the risk of thrombolism.
Eating and Drinking
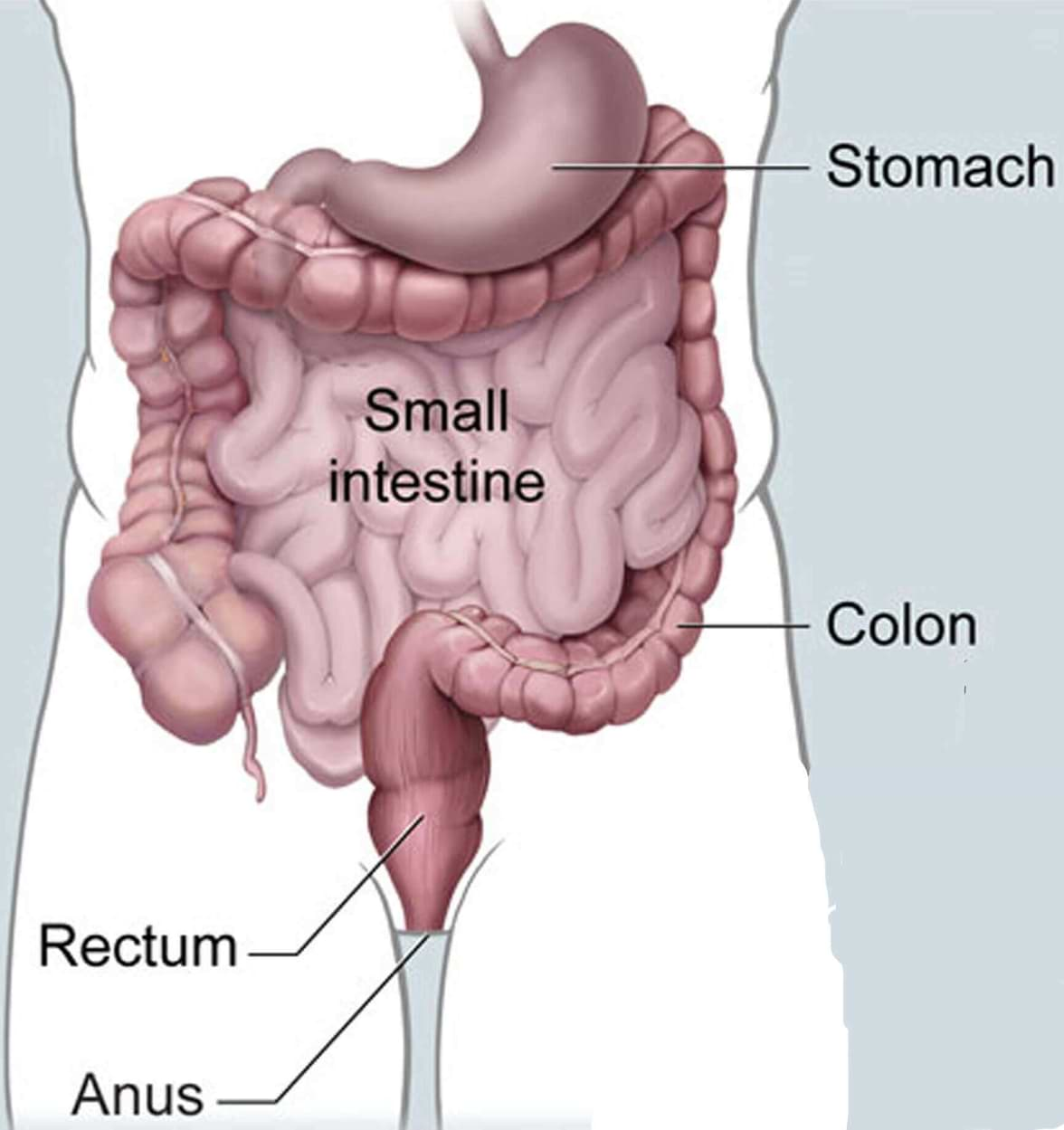
You may not feel much like eating or drinking, but this is an important part of the recovery process. Our health care team may start you out with ice chips or clear liquids. The stomach and intestines (digestive tract) is one of the last parts of the body to recover from the drugs used during surgery. You will need to have signs of stomach and bowel activity before you will be allowed to eat. You will likely be on a clear liquid diet until this happens. Once it does, you may get to try solid foods.
Activity
- Our health care team will try to have you move around as soon as possible after surgery. They may even have you out of bed and walking the same day. While this may be hard at first, it helps speed your recovery by getting your digestive tract moving. It also helps your circulation and helps prevent blood clots from forming in your legs.
- Our team shall also encourage you to do deep breathing exercises. This helps fully inflate your lungs and reduces the risk of pneumonia. You are advised to take deep breaths and cough every hour to help prevent lung infections. You will use an incentive spirometer (a small device used in breathing exercises to prevent complications after major surgery) 10-15 times every hour.
Going home
Once you are eating and walking, all tube/drains placed during surgery are removed, and then you may be ready to go home. Before leaving for home our health care team shall give you detailed guidance regarding diet, activities, medications & further plan of treatment.