Cholangitis
OVERVIEW | CAUSES | RISK FACTORS | SYMPTOMS | COMPLICATION | DIAGNOSIS | TREATMENT | PREVENTION | REFERENCES
OVERVIEW
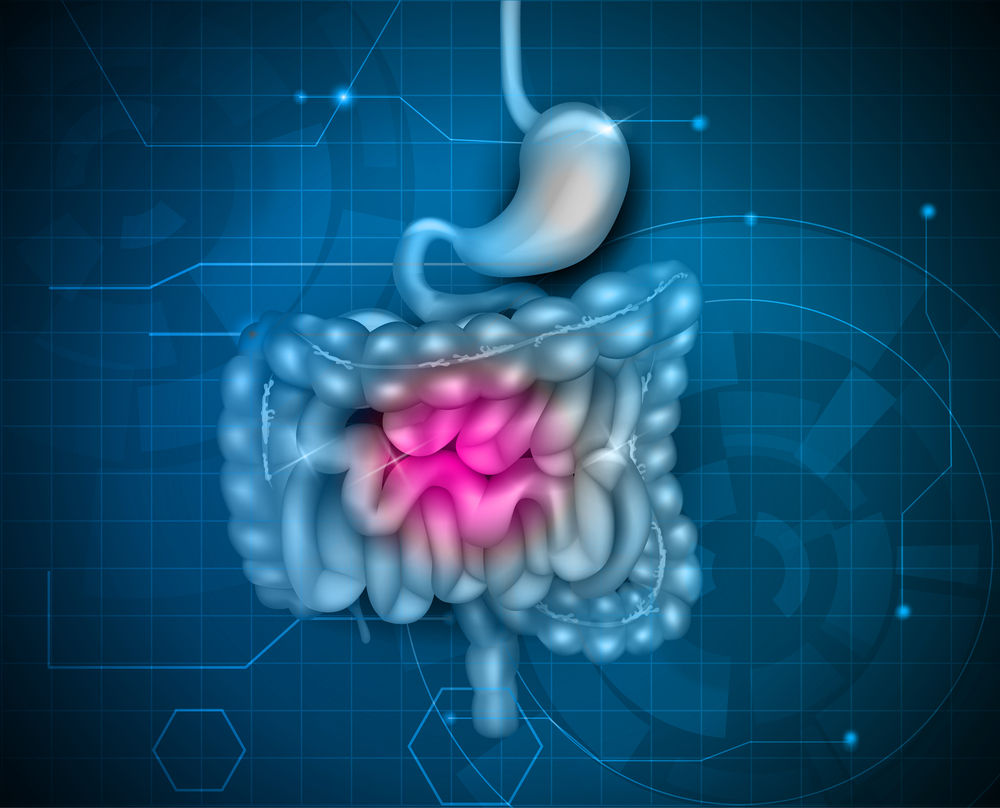
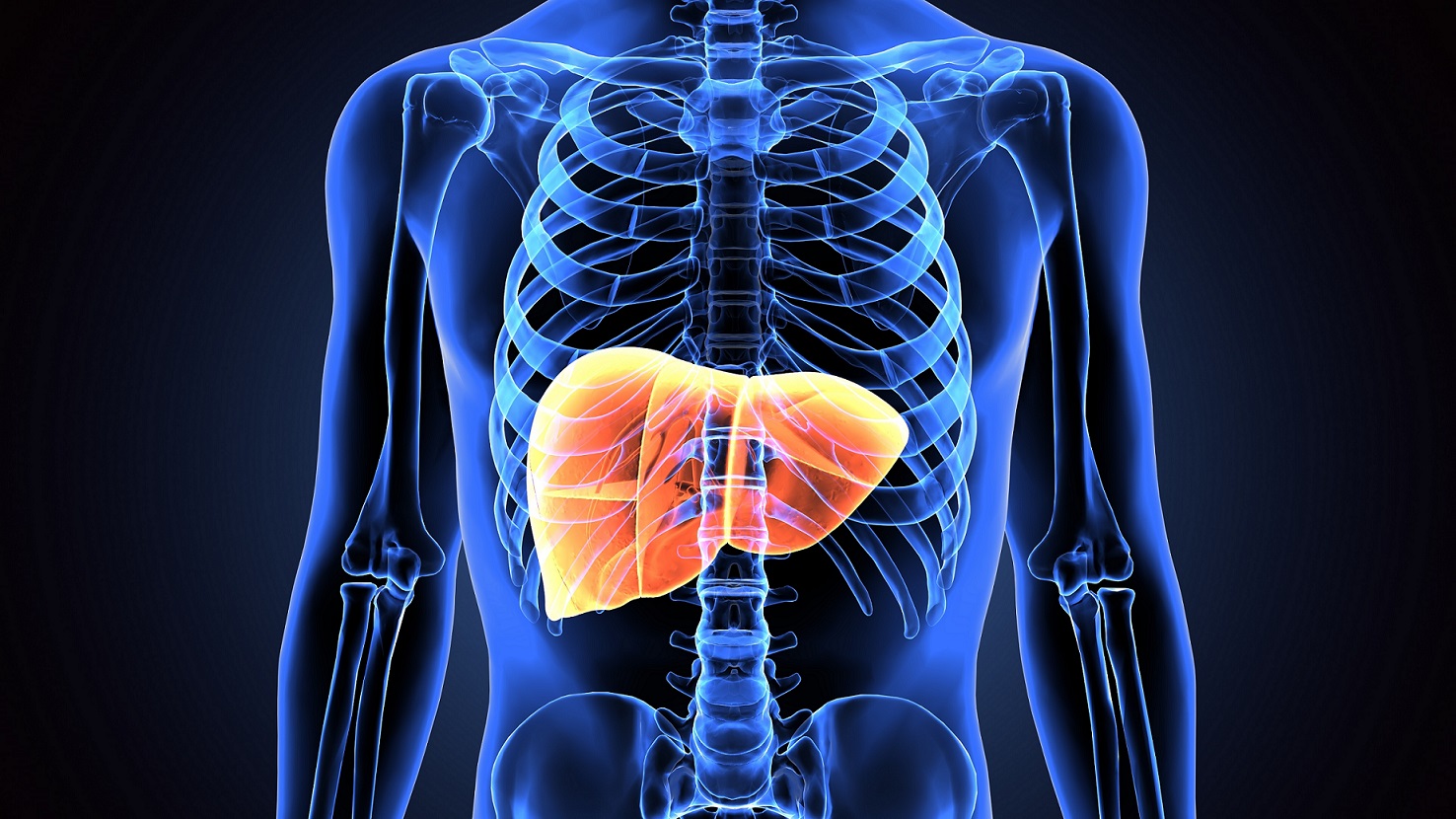
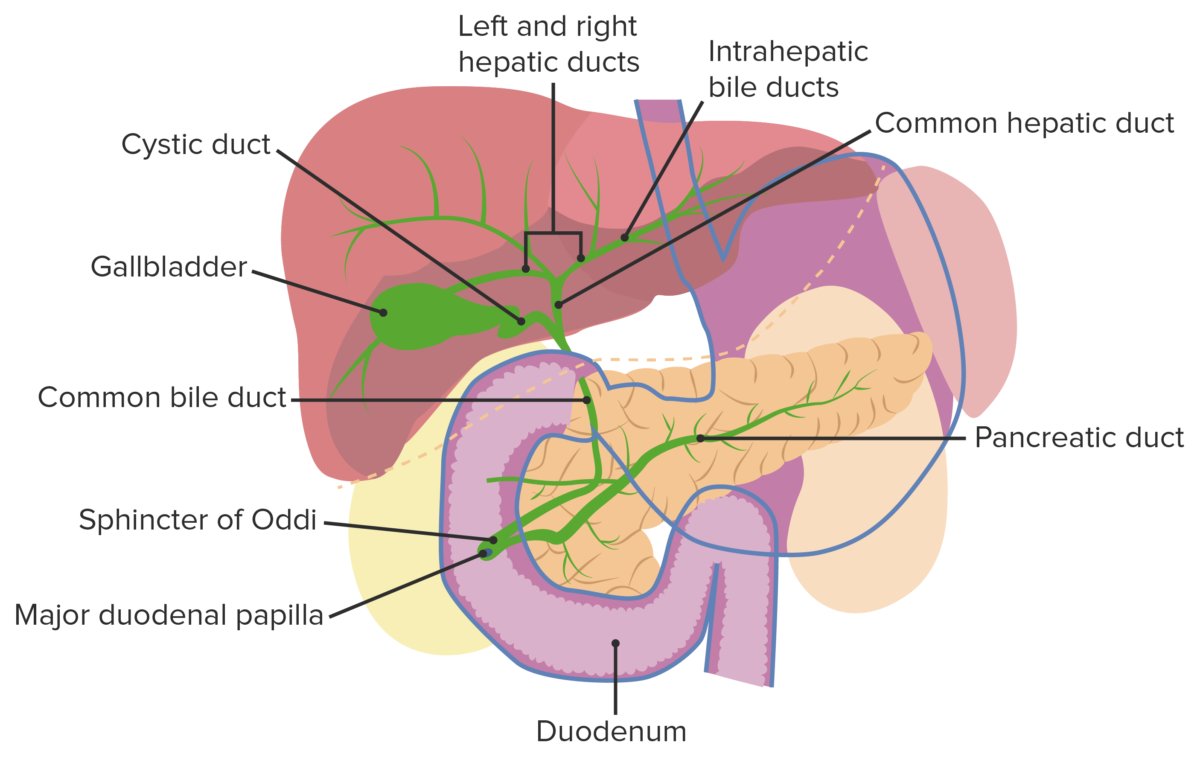
Cholangitis is an inflammation of the bile duct system. The bile duct system carries bile from your liver and gallbladder into the first part of your small intestine (the duodenum).
In most cases cholangitis is caused by a bacterial infection, and often happens suddenly. But in some cases it may be long-term (chronic). Some people develop inflammation and cholangitis as part of an autoimmune condition.
CAUSES
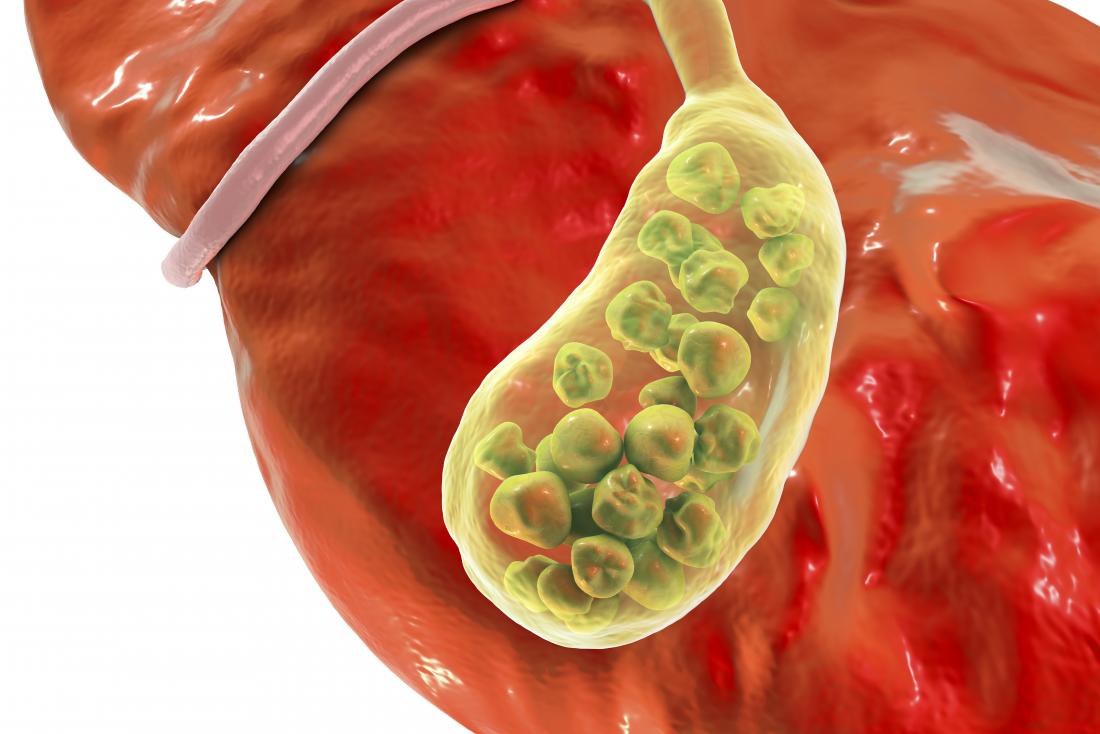
In most cases cholangitis is caused by a blocked duct somewhere in your bile duct system. The blockage is most commonly caused by gallstones or sludge impacting the bile ducts. Autoimmune disease such as primary sclerosing cholangitis may affect the system.
Other, less common causes of cholangitis include:
- A tumor
- Blood clots
- A narrowing of a duct that may happen after surgery
- Swollen pancreas
- A parasite infection
Cholangitis may also be caused when you have:
- A backflow of bacteria from your small intestine
- A blood infection (bacteremia)
- A test done to check your liver or gallbladder (such as a test where a thin tube or endoscope is put into your body)
The infection causes pressure to build up in your bile duct system, which can spread to other organs of the bloodstream if it is not treated.
RISK FACTORS
If you have had gallstones you are at greater risk for cholangitis. Other risk factors include:
- Having autoimmune diseases such as inflammatory bowel disease (ulcerative colitis or Crohn's disease)
- Recent medical procedures involving the bile duct area
- Having human immunodeficiency virus (HIV)
- Traveling to countries where you might be exposed to worms or parasites
SYMPTOMS
Each person’s symptoms may vary, and may be non-specific or severe, including:
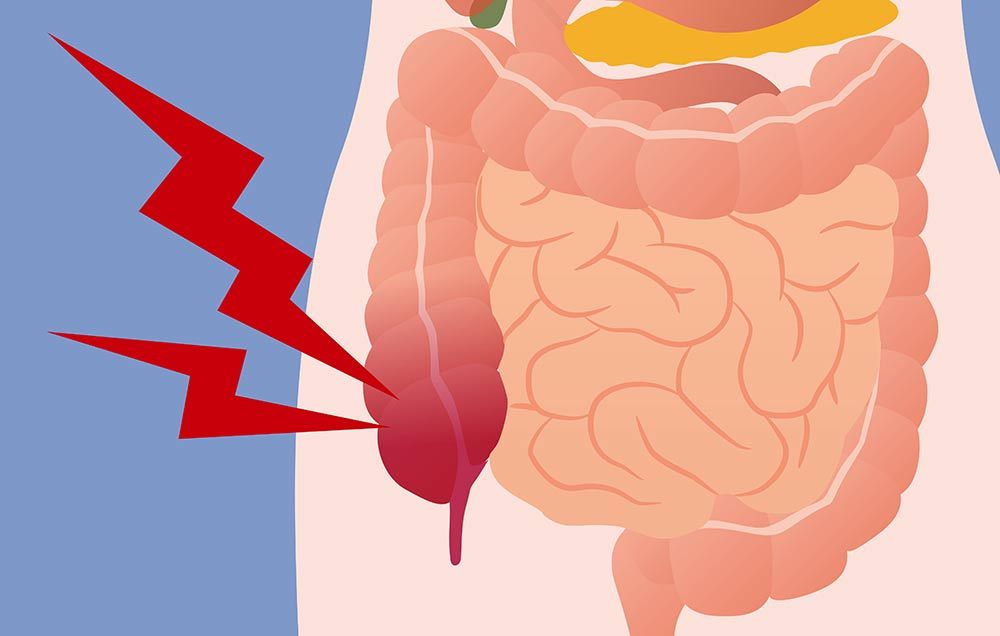
- Pain in the upper right part of your belly (abdomen)
- Fever
- Chills
- Yellowing of the skin and eyes (jaundice)
- Nausea and vomiting
- Clay-colored stools
- Dark urine
- Low blood pressure
- Lethargy
- Changes in alertness
The symptoms of cholangitis may look like other health problems. Always see your healthcare provider to be sure.
COMPLICATIONS
Cholangitis can lead to serious health problems if it isn’t treated. Complications include:
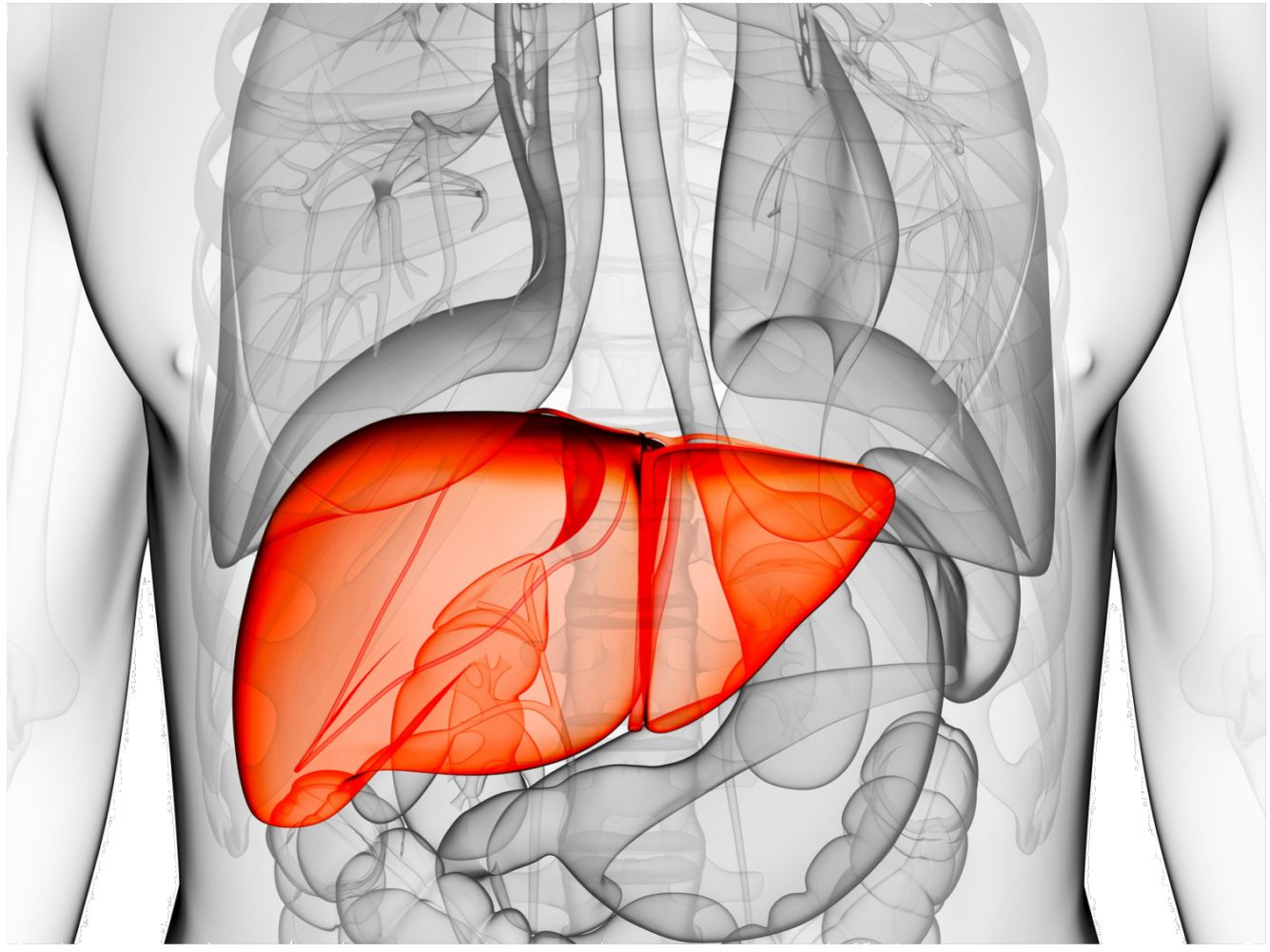
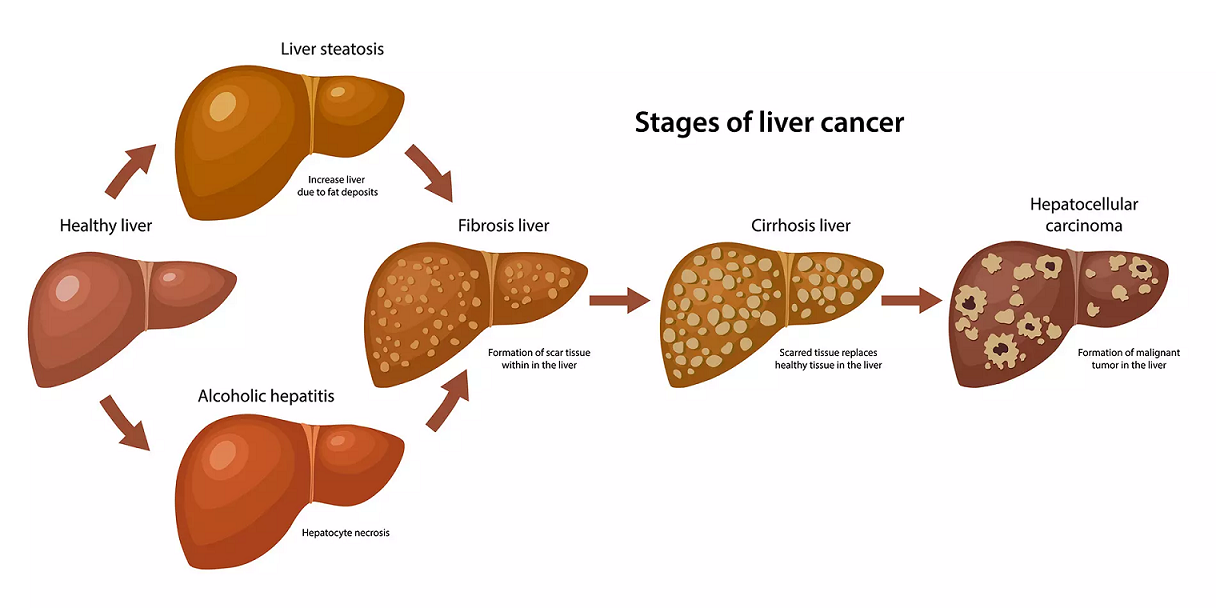
- Liver problems. Cholangitis can cause liver scarring (cirrhosis). This can slow liver function or lead to liver failure. It also increases the risk of liver cancer. It can cause liver swelling and high blood pressure.
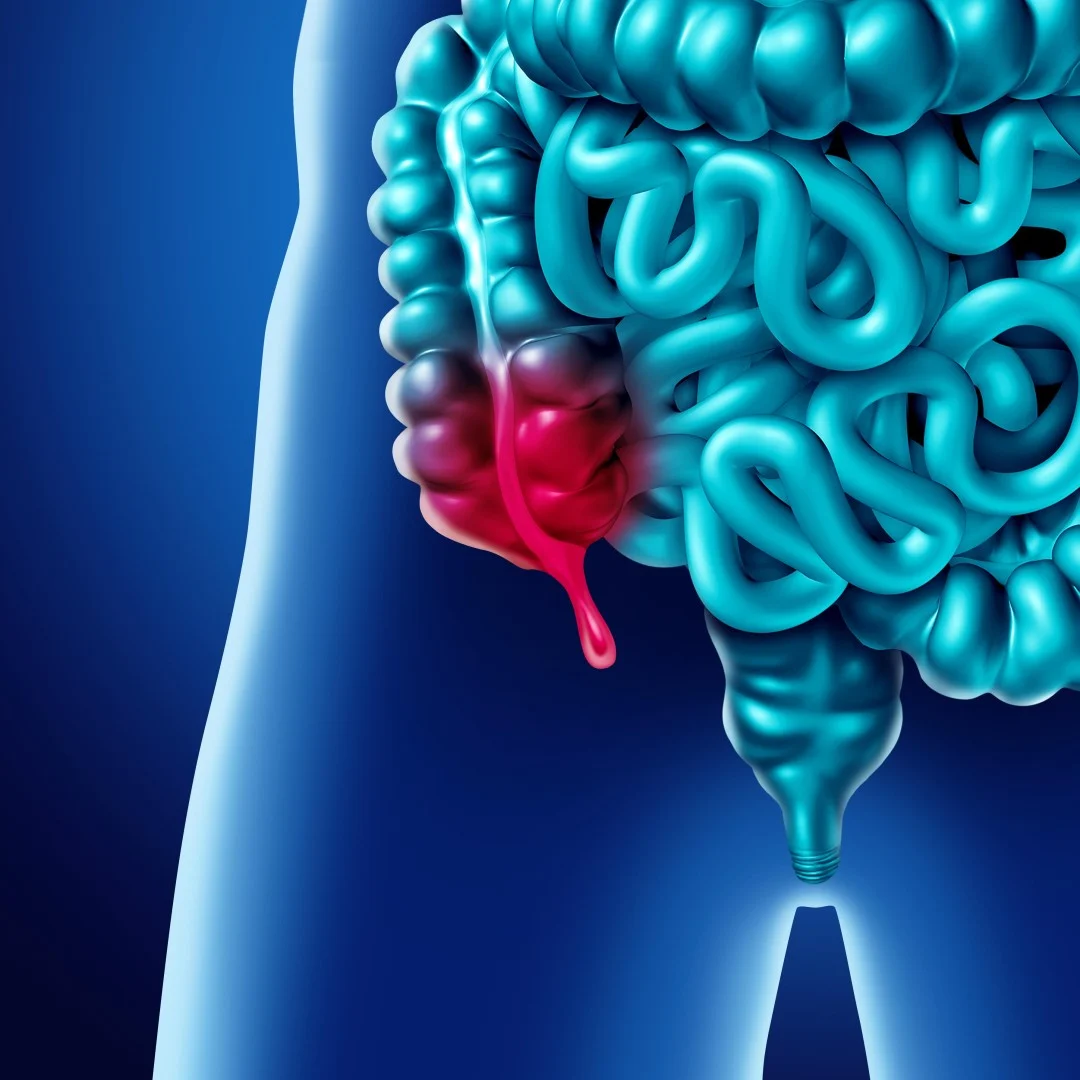
- Gallstones. Blocked bile can harden into stones. This may cause pain and infections.
- Enlarged spleen. If the liver isn’t working properly and can’t filter out wastes and toxins, old blood cells can collect in the spleen, causing it to swell.
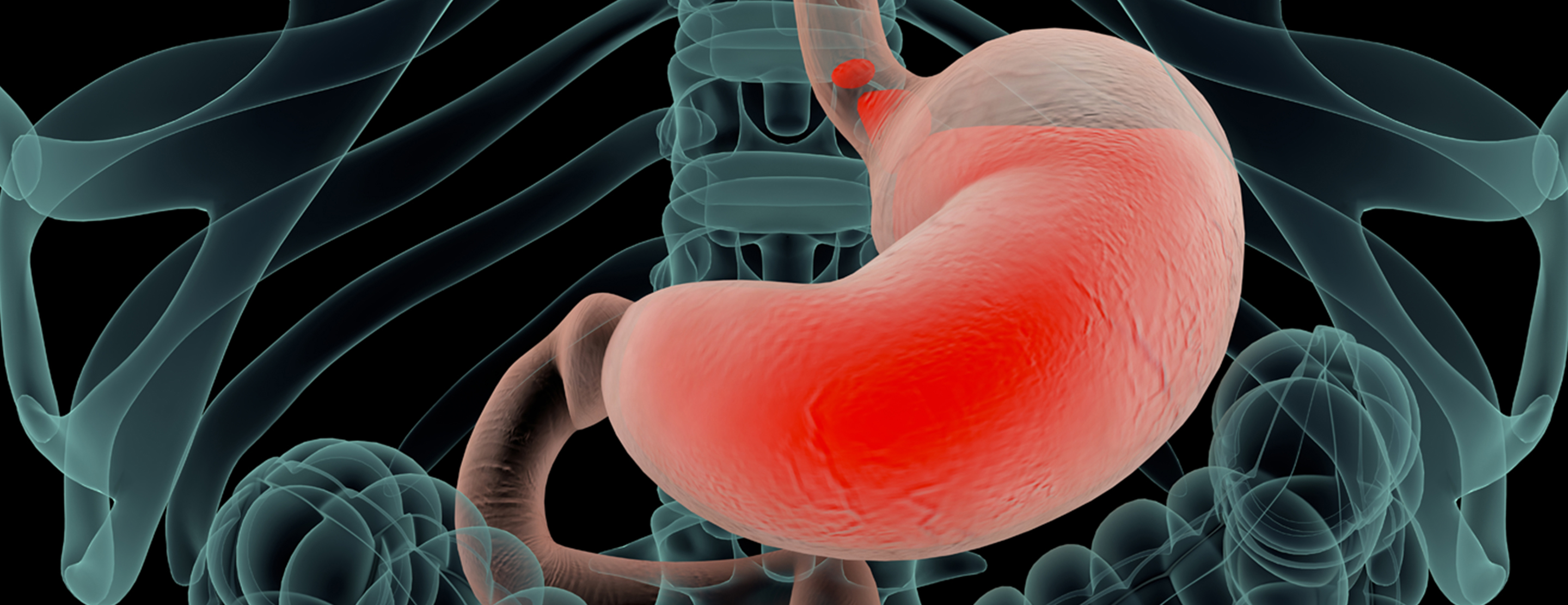
- Enlarged veins. High blood pressure in the liver may put too much pressure on veins in the stomach. This can lead to swollen and broken veins. It may also cause bleeding.
- Blood infection. Acute cholangitis can lead to sepsis (a blood infection). This can damage several parts of the body and may be life-threatening if not treated.
Chronic cholangitis is also linked to other conditions including thyroid problems, scleroderma, and rheumatoid arthritis.
DIAGNOSIS
The pain from cholangitis can feel a lot like the pain from gallstones.
To be sure you have cholangitis, your healthcare provider will look at your past health and give you a physical exam. He or she may also use other tests.
You may have blood tests including:
- Complete blood count (CBC). This test measures your white blood cell count. You may have a high white blood cell count if you have an infection.
- Liver function tests. A group of special blood tests that can tell if your liver is working properly.
- Blood cultures. Tests to see if you have a blood infection.
You may also have imaging tests including:
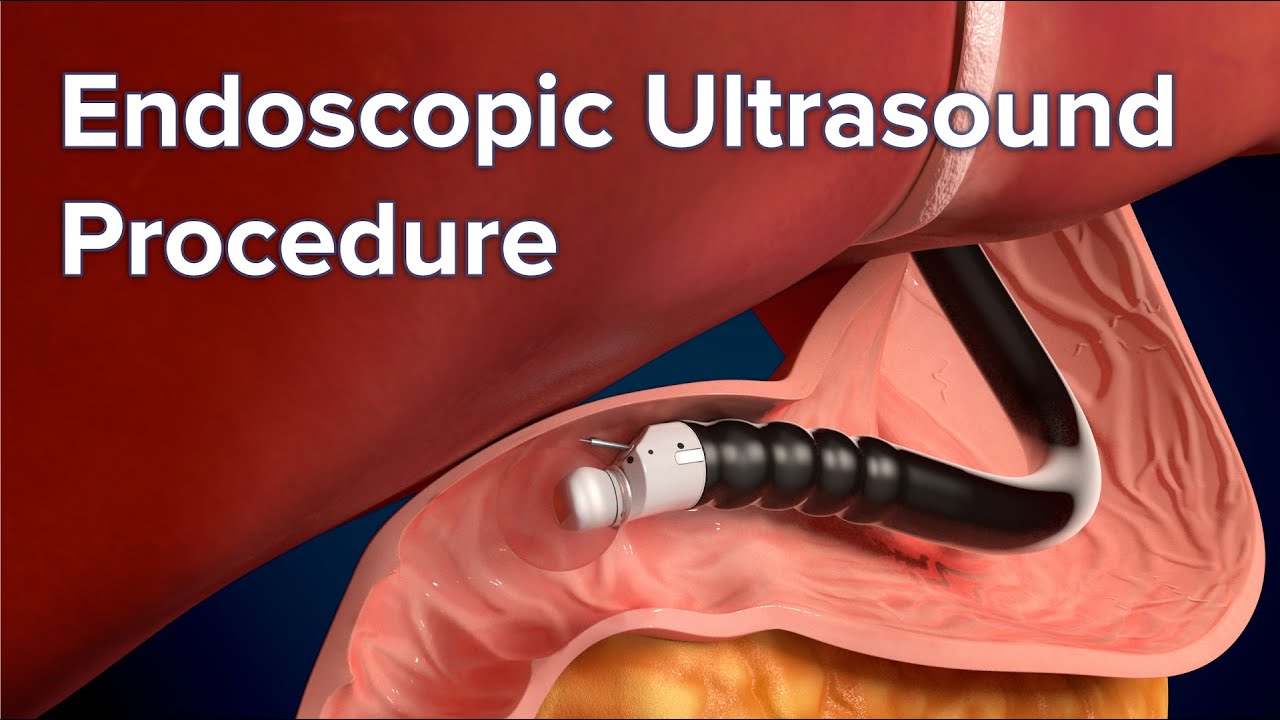
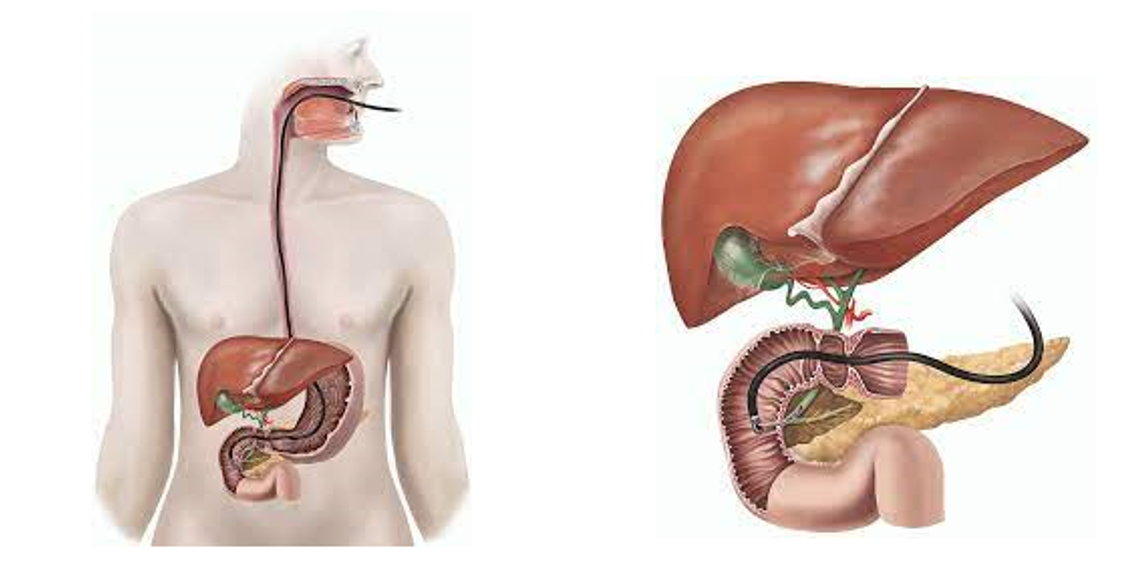
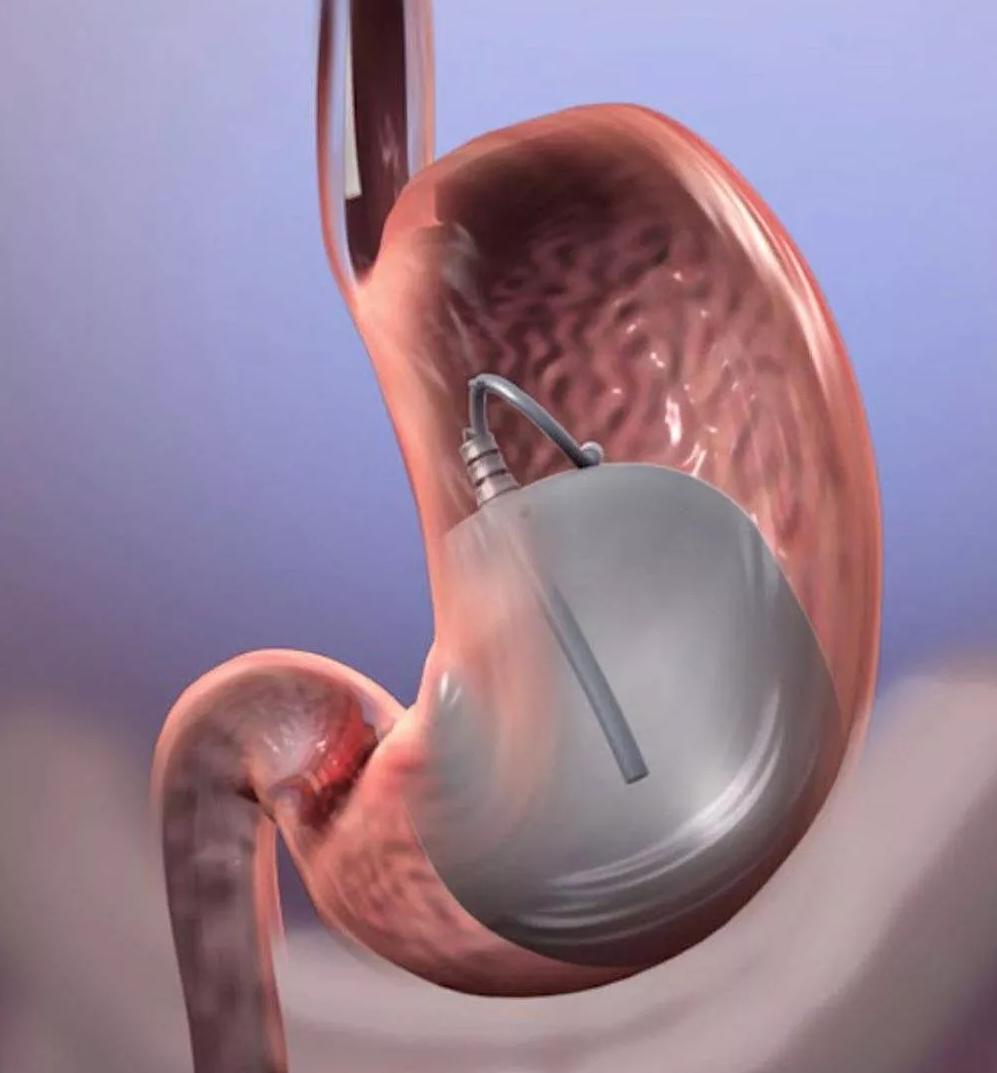
- Ultrasound (also called sonography). This test creates images of your internal organs on a computer screen using high-frequency sound waves. It is used to see organs in your belly such as the liver, spleen, and gallbladder. It also checks blood flow through different vessels. It can be done outside the body (external). Or it may be done inside the body (internal). If internal, it is called an endoscopic ultrasound (EUS).
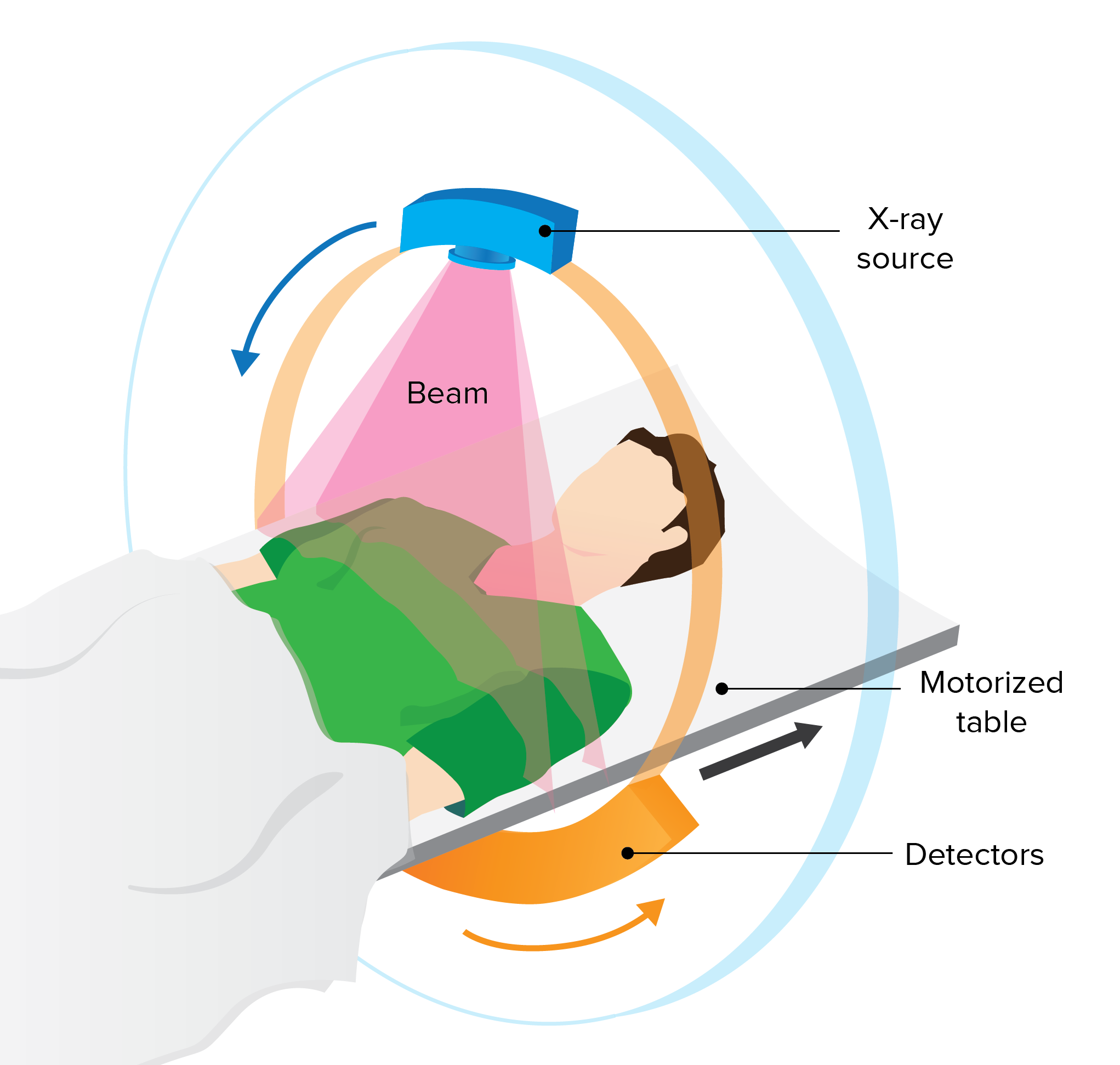
- CT scan. A CT scan may be done with a dye that is swallowed or injected through an IV. This will show the abdomen and pelvis including the bile drainage area. It can help determine why there is a blockage.
- Magnetic resonance cholangiopancreatography (MRCP). This test is used to look for any problems in your abdomen. It can show if there are gallstones in your bile duct. The test is done from outside your body. It does not involve putting a tube (endoscope) into your body. It uses a magnetic field and radio frequency to make detailed pictures.
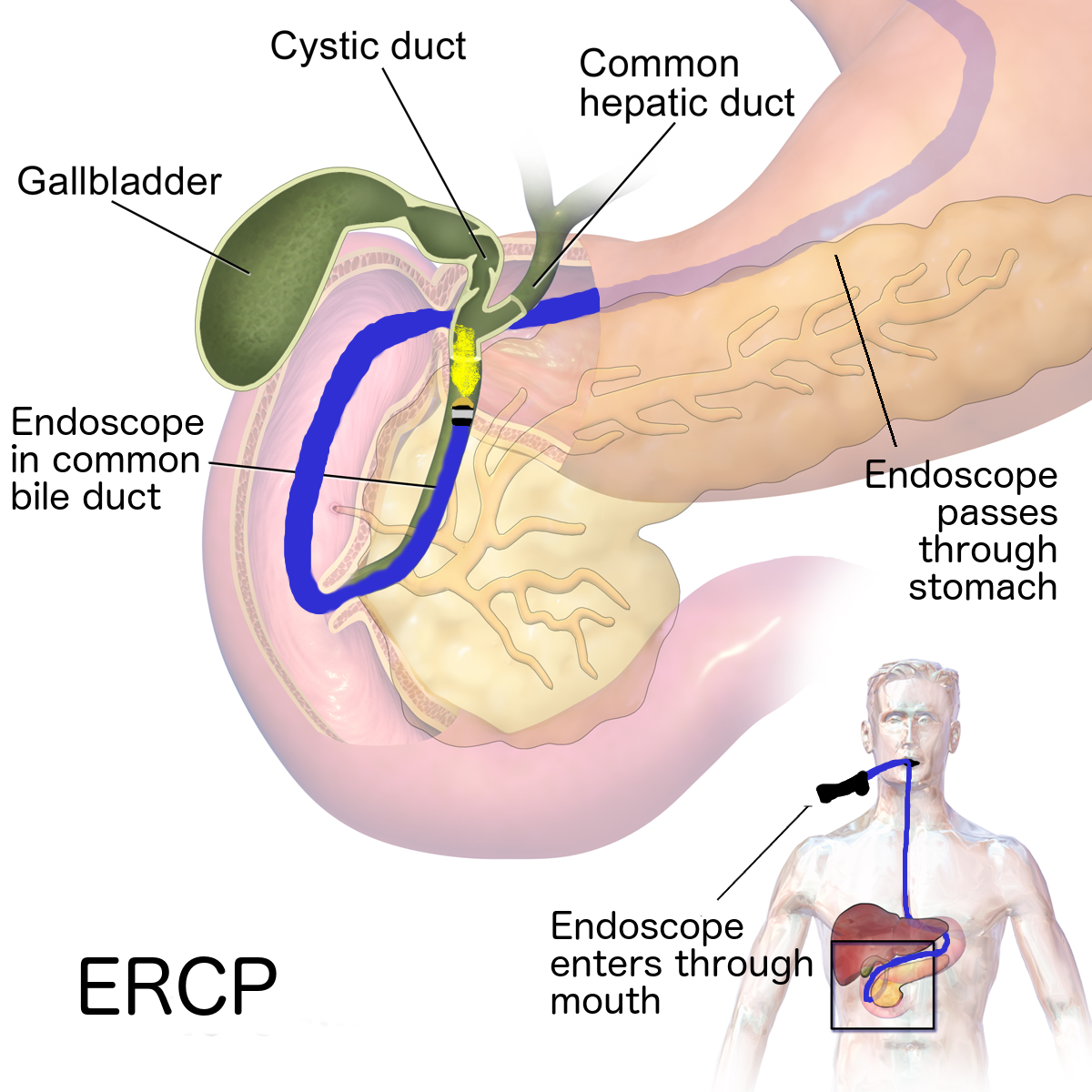
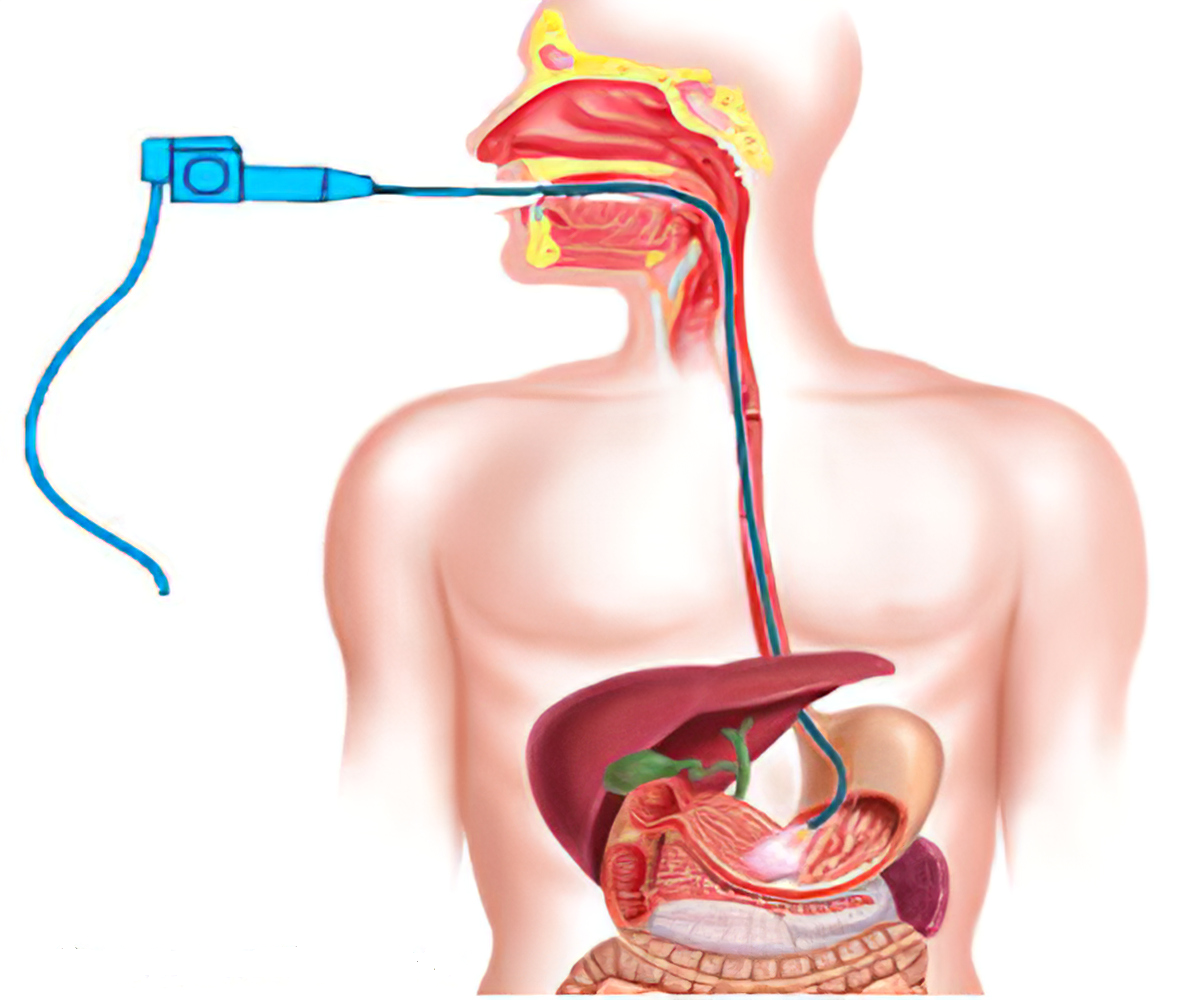
- ERCP (endoscopic retrograde cholangiopancreatography). This is used to find and treat problems in your liver, gallbladder, bile ducts, and pancreas. It uses X-ray and a long flexible tube with a light and camera at one end (an endoscope). The tube is put into your mouth and throat. It goes down your food pipe (esophagus), through your stomach, and into the first part of your small intestine (the duodenum). A dye is put into your bile ducts through the tube. The dye lets the bile ducts be seen clearly on X-rays. If required, this procedure can also help open up your bile ducts.
- Percutaneous transhepatic cholangiography (PTC). A needle is put through your skin and into your liver. Dye is put into your bile duct so that it can be seen clearly on X-rays. This procedure can also be used to open up the bile ducts if your physicians are unable to do it internally with an ERCP.
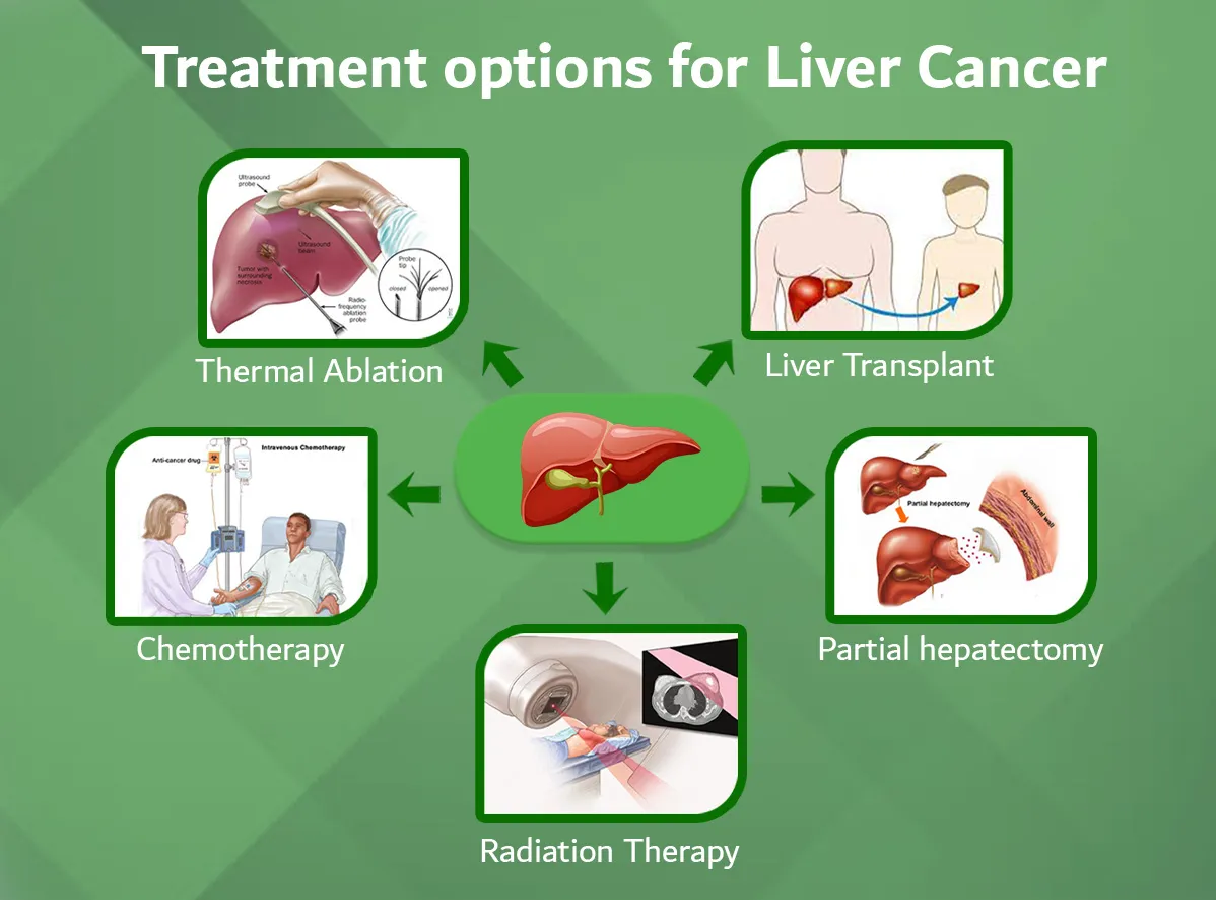
TREATMENT
It is important to get a diagnosis right away. Most people with cholangitis feel very sick. They see their healthcare provider or go to the emergency room.
If you have cholangitis, you will likely be in the hospital for a few days. You will be given fluids by IV (intravenous) line through a vein. You will also have pain medicine and bacteria-fighting medicine (antibiotics).
You may also need to drain the fluid in your bile duct and find the cause of any blockage. In most cases, this is done by a method called ERCP (endoscopic retrograde cholangiopancreatography).
To drain your bile duct using ERCP, a long thin flexible tube (endoscope) is put in your mouth. The scope goes down your food pipe (esophagus) and into your stomach. It passes into the first part of your small intestine (the duodenum) and into the bile ducts. The doctor can see the inside of these organs and ducts on a video screen. The video screen is connected to a camera in the scope. Sometimes a tube is left to the outside to drain bile. In this situation, a small tube is passed into the ducts to drain fluid. This tube is brought out through the skin, where it lets fluid drain out until the infection and inflammation clear up.
You may also have firm tubes (stents) put into the bile ducts to keep them open. Gallstones can also be removed. In most cases these things can be done using the ERCP scope.
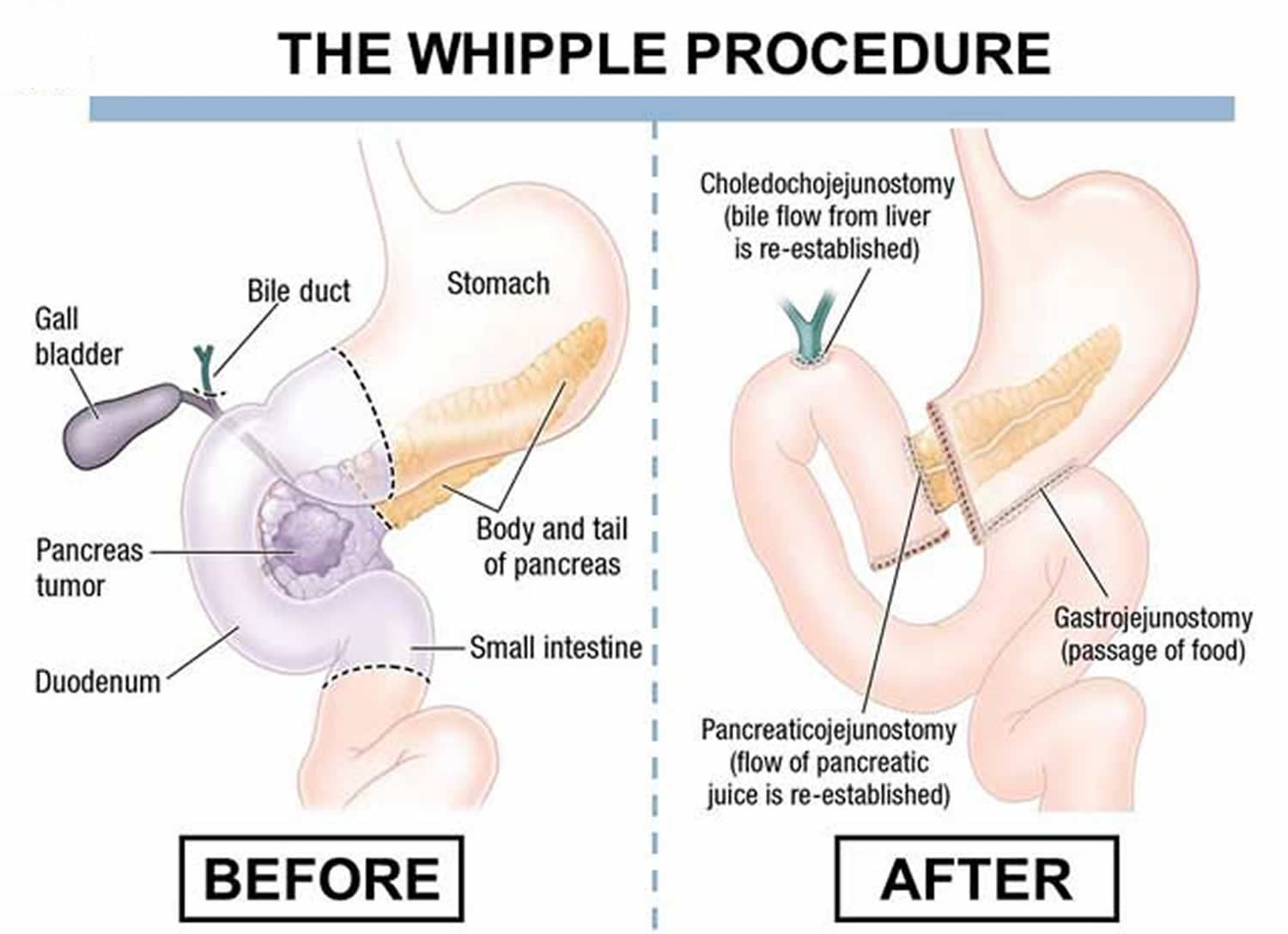
You may need surgery if treatment doesn’t work or if you are getting worse. Surgery will open your ducts to drain the bile and reduce the buildup of fluid.
PREVENTION
Because the exact cause of cholangitis cannot be identified, finding preventive measures can be difficult. However, you can take steps to lessen liver damage, including:
- Quit smoking, stop drinking alcohol and stop using illegal drugs
- Take all medicines as directed by your doctor.
- Eat a healthy, well balanced diet.
- Get regular exercise, such as walking.
Healthy food choices could include eating foods rich in vitamins A, D, E and K and/or supplements of these vitamins. Also, foods high in vitamin D and calcium could help prevent osteoporosis. Ask your doctor for specific foods high in these vitamins and minerals.
Foods to avoid include raw shellfish (because of possible bacteria presence); plus food high in salt, fat, and carbohydrates – especially added sugars.