Reflux in Children
OVERVIEW | CAUSES | RISK FACTORS | SYMPTOMS | COMPLICATION | DIAGNOSIS | TREATMENT | PREVENTION | REFERENCES

OVERVIEW
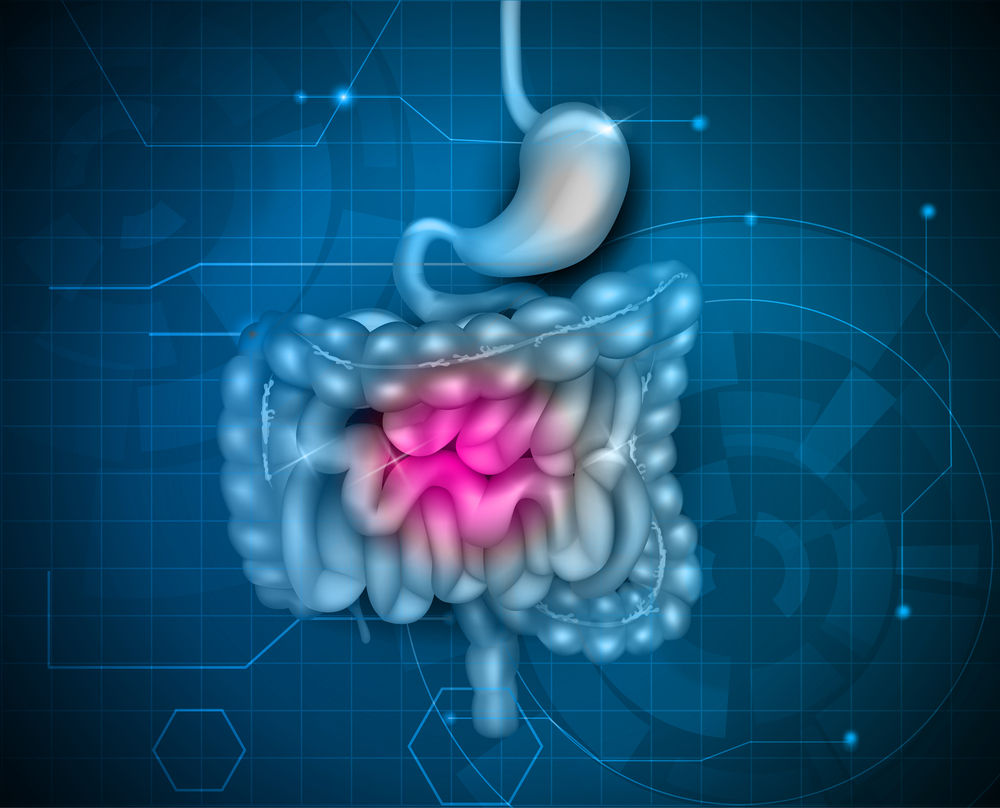
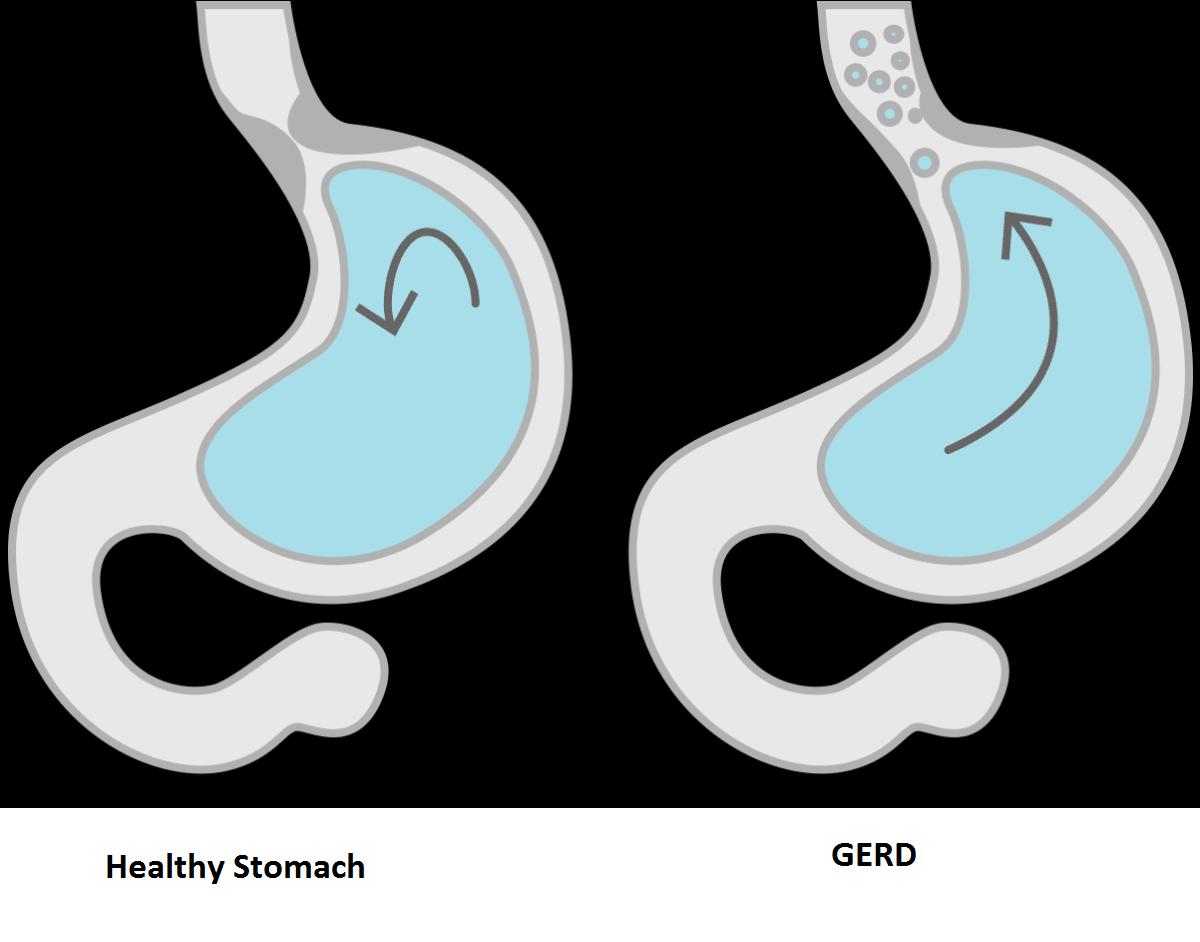
The esophagus is the tube that carries food from your mouth to your stomach. If your child has reflux, his or her stomach contents come back up into the esophagus. Another name for reflux is Gastroesophageal Reflux (GER).
GERD stands for Gastroesophageal Reflux Disease. It is a more serious and long-lasting type of reflux. If your child has reflux more than twice a week for a few weeks, it could be GERD.
CAUSES
There is a muscle (the lower esophageal sphincter) that acts as a valve between the esophagus and stomach. When your child swallows, this muscle relaxes to let food pass from the esophagus to the stomach. This muscle normally stays closed, so the stomach contents don't flow back into the esophagus.
In children who have reflux and GERD, this muscle becomes weak or relaxes when it shouldn't, and the stomach contents flow back into the esophagus. This can happen because of
- A hiatal hernia, a condition in which the upper part of your stomach pushes upward into your chest through an opening in your diaphragm
- Increased pressure on the abdomen from being overweight or having obesity
- Medicines, such as certain asthma medicines, antihistamines (which treat allergies), pain relievers, sedatives (which help put people to sleep), and antidepressants
- Smoking or exposure to secondhand smoke
- A previous surgery on the esophagus or upper abdomen
- A severe developmental delay
- Certain neurological conditions, such as cerebral palsy
RISK FACTORS
GERD is very common during a baby’s first year of life. It often goes away on its own. Your child is more at risk for GERD if he or she has:
- Down syndrome
- Neuromuscular disorders such as muscular dystrophy and cerebral palsy
SYMPTOMS
Your child might not even notice reflux. But some children taste food or stomach acid at the back of the mouth.
In children, GERD can cause
- Heartburn, a painful, burning feeling in the middle of the chest. It is more common in older children (12 years and up).
- Bad breath
- Nausea and vomiting
- Problems swallowing or painful swallowing
- Breathing problems
- The wearing away of teeth
COMPLICATIONS
Some babies and children who have GERD may not vomit. But their stomach contents may still move up the food pipe (esophagus) and spill over into the windpipe (trachea). This can cause asthma or pneumonia.
The vomiting that affects many babies and children with GERD can cause problems with weight gain and poor nutrition. Over time, when stomach acid backs up into the esophagus, it can also lead to:
- Inflammation of the esophagus, called esophagitis
- Sores or ulcers in the esophagus, which can be painful and may bleed
- A lack of red blood cells, from bleeding sores (anemia)
Adults may also have long-term problems from inflammation of the esophagus. These include:
- Narrowing, or stricture, of the esophagus
- Barrett’s esophagus, a condition where there are abnormal cells in the esophageal lining
DIAGNOSIS
In most cases, a doctor diagnoses reflux by reviewing your child's symptoms and medical history. If the symptoms do not get better with lifestyle changes and anti-reflux medicines, your child may need testing to check for GERD or other problems.
Several tests can help a doctor diagnose GERD. Sometimes doctors order more than one test to get a diagnosis. Commonly-used tests include
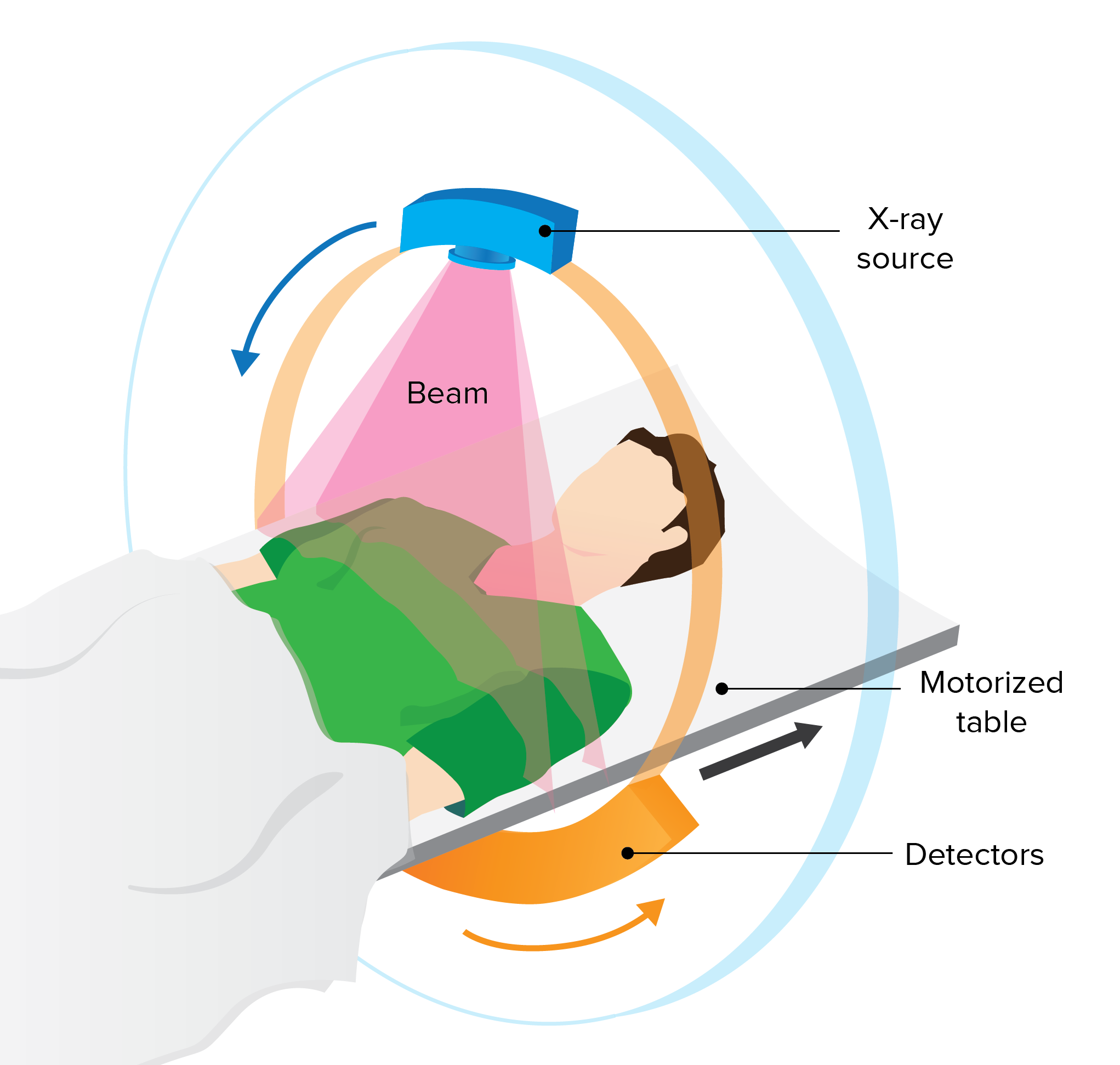
- Upper GI series, which looks at the shape of your child's upper GI (gastrointestinal) tract. You child will drink a contrast liquid called barium. For young children, the barium is mixed in with a bottle or other food. The health care professional will take several x-rays of your child to track the barium as it goes through the esophagus and stomach.
- Esophageal pH and impedance monitoring, which measures the amount of acid or liquid in your child's esophagus. A doctor or nurse places a thin flexible tube through your child's nose into the stomach. The end of the tube in the esophagus measures when and how much acid comes back up into the esophagus. The other end of the tube attaches to a monitor that records the measurements. Your child will wear the tube for 24 hours. He or she may need to stay in the hospital during the test.
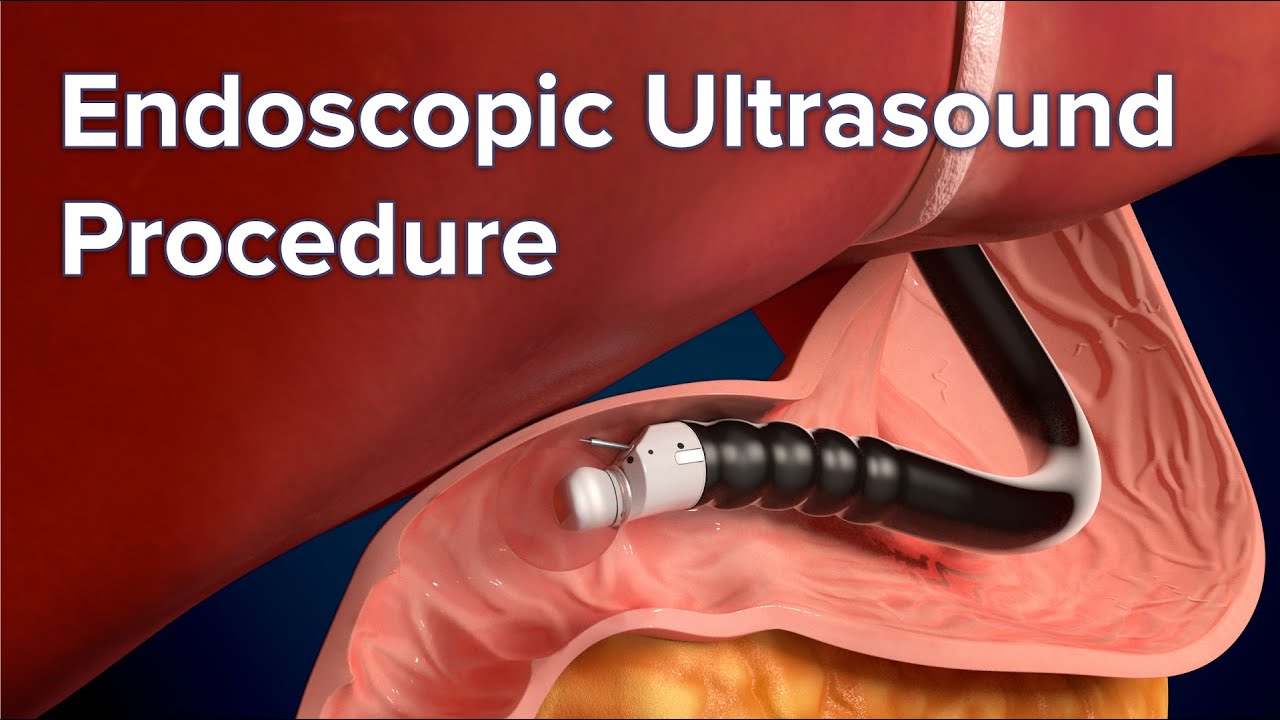
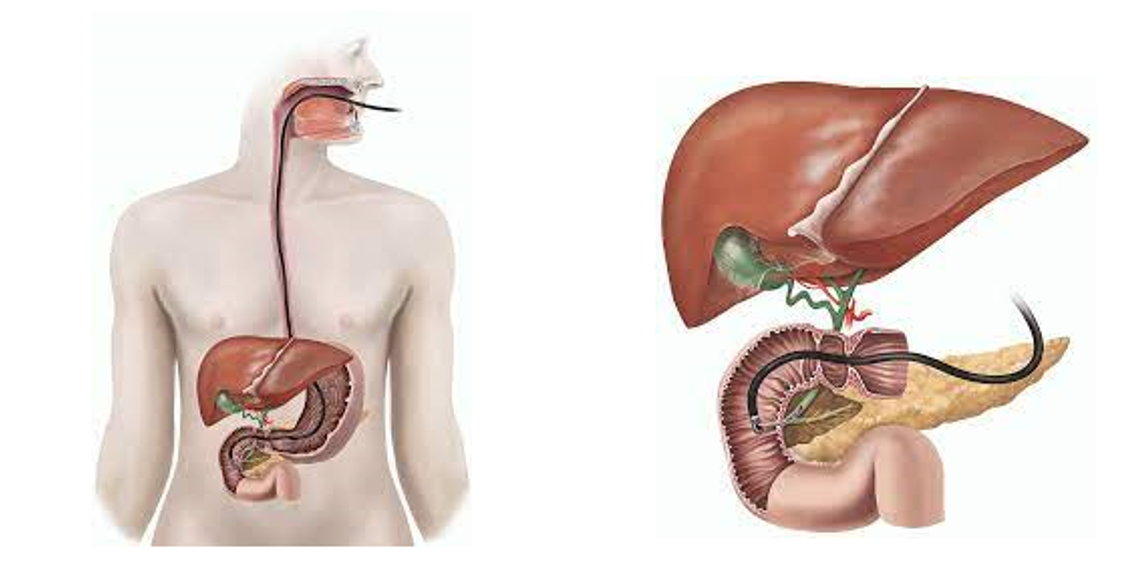
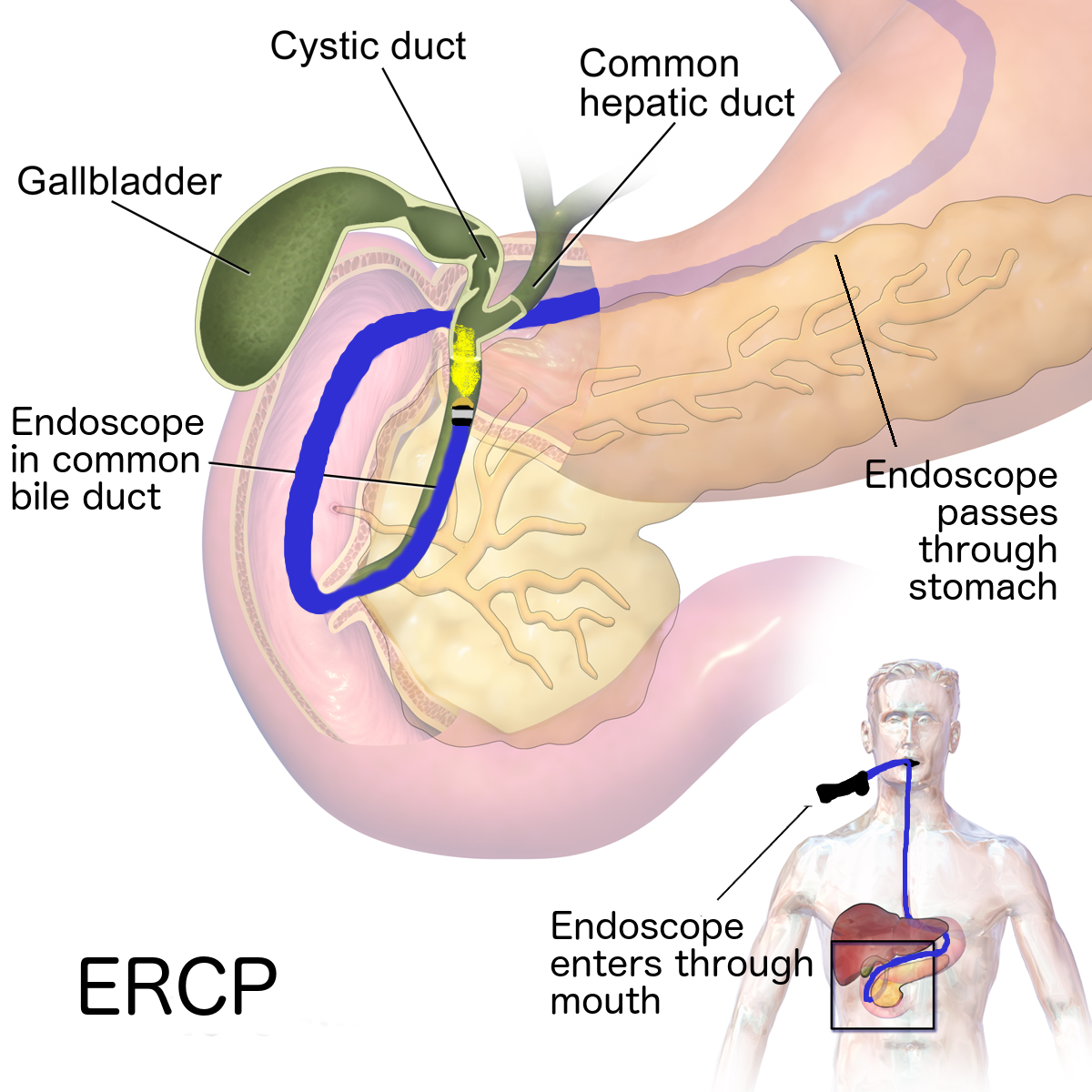
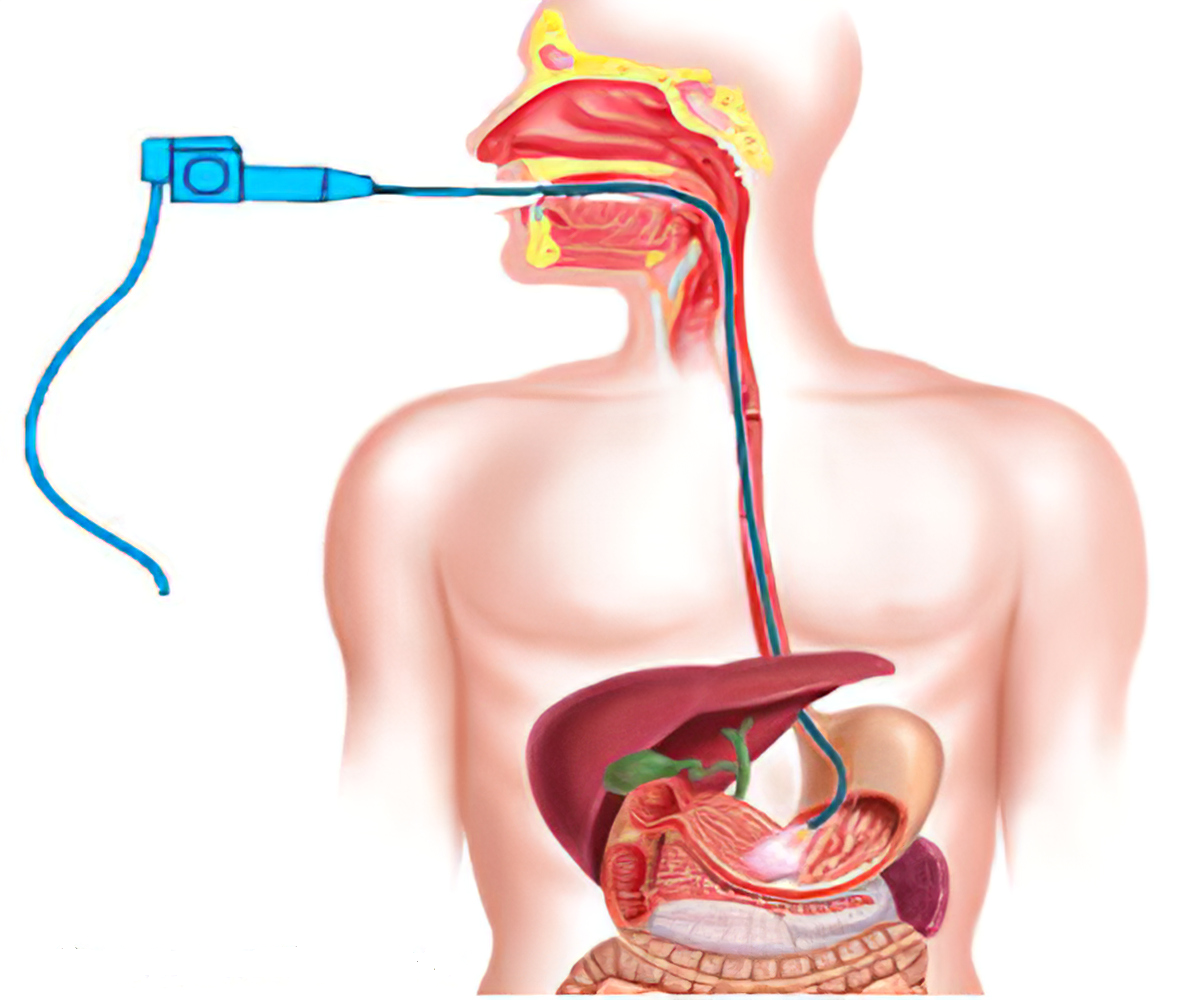
- Upper gastrointestinal (GI) endoscopy and biopsy, which uses an endoscope, a long, flexible tube with a light and camera at the end of it. The doctor runs the endoscope down your child's esophagus, stomach, and first part of the small intestine. While looking at the pictures from the endoscope, the doctor may also take tissue samples (biopsy).
TREATMENT
Sometimes reflux and GERD in children can be treated with lifestyle changes:
- Losing weight, if needed
- Eating smaller meals
- Avoiding high-fat foods
- Wearing loose-fitting clothing around the abdomen
- Staying upright for 3 hours after meals and not reclining and slouching when sitting
- Sleeping at a slight angle. Raise the head of your child's bed 6 to 8 inches by safely putting blocks under the bedposts.
If changes at home do not help enough, the doctor may recommend medicines to treat GERD. The medicines work by lowering the amount of acid in your child's stomach.
Some medicines for GERD in children are over-the-counter, and some are prescription medicines. They include
- Over-the-counter antacids
- H2 blockers, which decrease acid production
- Proton pump inhibitors (PPIs), which lower the amount of acid the stomach makes
- Prokinetics, which help the stomach empty faster
If these don't help and your child still has severe symptoms, then surgery might be an option. A pediatric gastroenterologist, a doctor who treats children who have digestive diseases, would do the surgery.
To minimize reflux:
- Feed your baby in an upright position. Also hold your baby in a sitting position for 30 minutes after feeding, if possible. Gravity can help stomach contents stay where they belong. Be careful not to jostle or jiggle your baby while the food is settling.
- Try smaller, more-frequent feedings. Feed your baby slightly less than usual if you're bottle-feeding, or cut back a little on nursing time.
- Take time to burp your baby. Frequent burps during and after feeding can keep air from building up in your baby's stomach.
- Put baby to sleep on his or her back. Most babies should be placed on their backs to sleep, even if they have reflux.
Remember, infant reflux is usually little cause for concern. Just keep plenty of burp cloths handy as you ride it out.
REFERENCE
- https://medlineplus.gov/refluxinchildren.html
- https://www.hopkinsmedicine.org/health/conditions-and-diseases/gerd-gastroesophageal-reflux-disease-in-children
- https://www.mayoclinic.org/diseases-conditions/infant-acid-reflux/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5578061/