Diabetes
Diabetes is home for 55+ other medical illness
New study suggests that People with type 2 diabetes are at higher risk of developing 57 health conditions compared with non-diabetics.

About the Study
A study of people with type 2 diabetes found that those with the condition were at a higher risk of developing up to 57 other health conditions compared with those who were not diabetic.
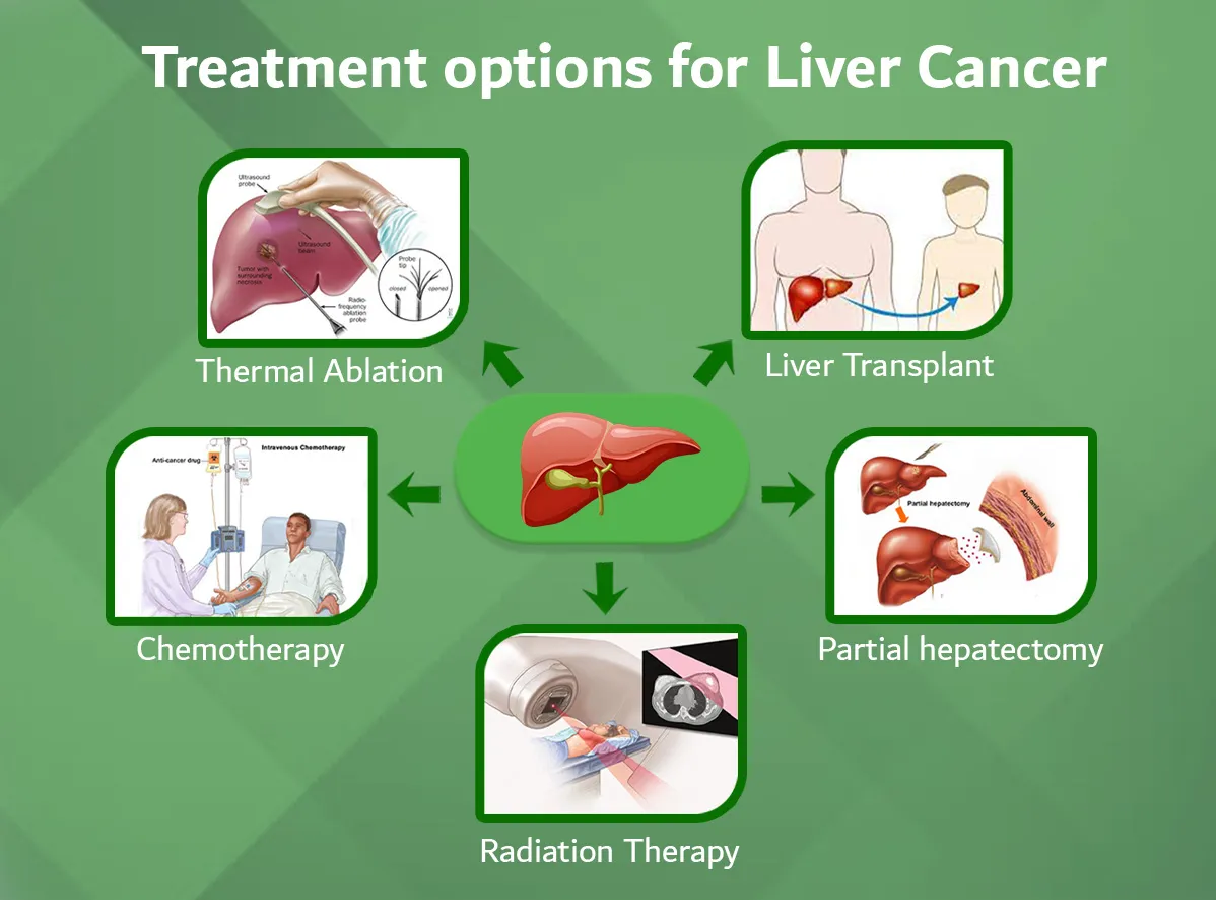
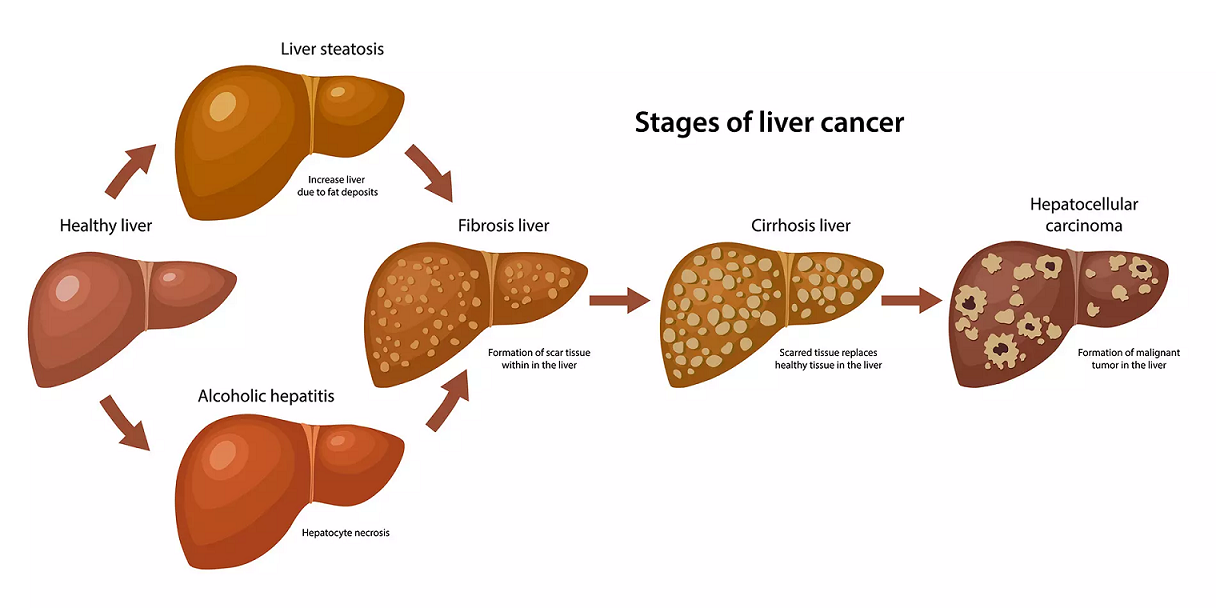
People with type 2 diabetes were 5.2 times more likely to have end-stage kidney disease, 4.4 times more likely to get liver cancer and 3.2 times more likely to develop a sight-threatening condition called macular degeneration, the scientists from Cambridge University said.
The study found that those with type 2 diabetes developed the conditions, on average, five years earlier than people who didn't have type 2 diabetes. The risks of developing circulatory, genitourinary, neurological and eye conditions were also "much higher" for people diagnosed with type 2 diabetes under the age of 50 than those diagnosed at "a later age," the authors of the study said.
It usually occurs in people older than 45, but increasing numbers of younger people are developing it, in part due to increasing rates of obesity, which makes people far more vulnerable to the condition.
The study said that delaying the onset of type 2 diabetes was "essential" to cut the risk of poor health in middle age.
The study's findings were "a stark reminder of the extensive and serious long-term effects of diabetes on the body."
Type 2 diabetes is a condition where there is too much sugar in the blood because the body can't regulate it properly due to problems with a hormone called insulin — either there isn't enough of it, or it can't work properly.
Most complications occur due to blood vessel damage in the major organs — most commonly the eyes, kidneys, heart, blood pressure, feet, and nervous system — which is made worse by poorly controlled blood sugar levels. There's no cure for the condition, but it can be treated with a healthy diet and increased physical activity. Medications or insulin injections may also be required.
The scientists used data from the UK Biobank and UK Clinical Practice Research from 3 million people in the UK to examine the link between diabetes and 116 health conditions that people normally get in middle age.
The study is the most comprehensive of its kind, according to the researchers, The new study, which has not yet been peer reviewed, is being presented at the Diabetes UK Professional Conference online and in London. It hasn't yet been published or formally scrutinized by other experts.
Health Conditions related to Diabetes
There are a number of conditions associated with diabetes. These include coeliac disease, thyroid disease and haemochromatosis.
Find out more about these conditions and how they're related to diabetes:
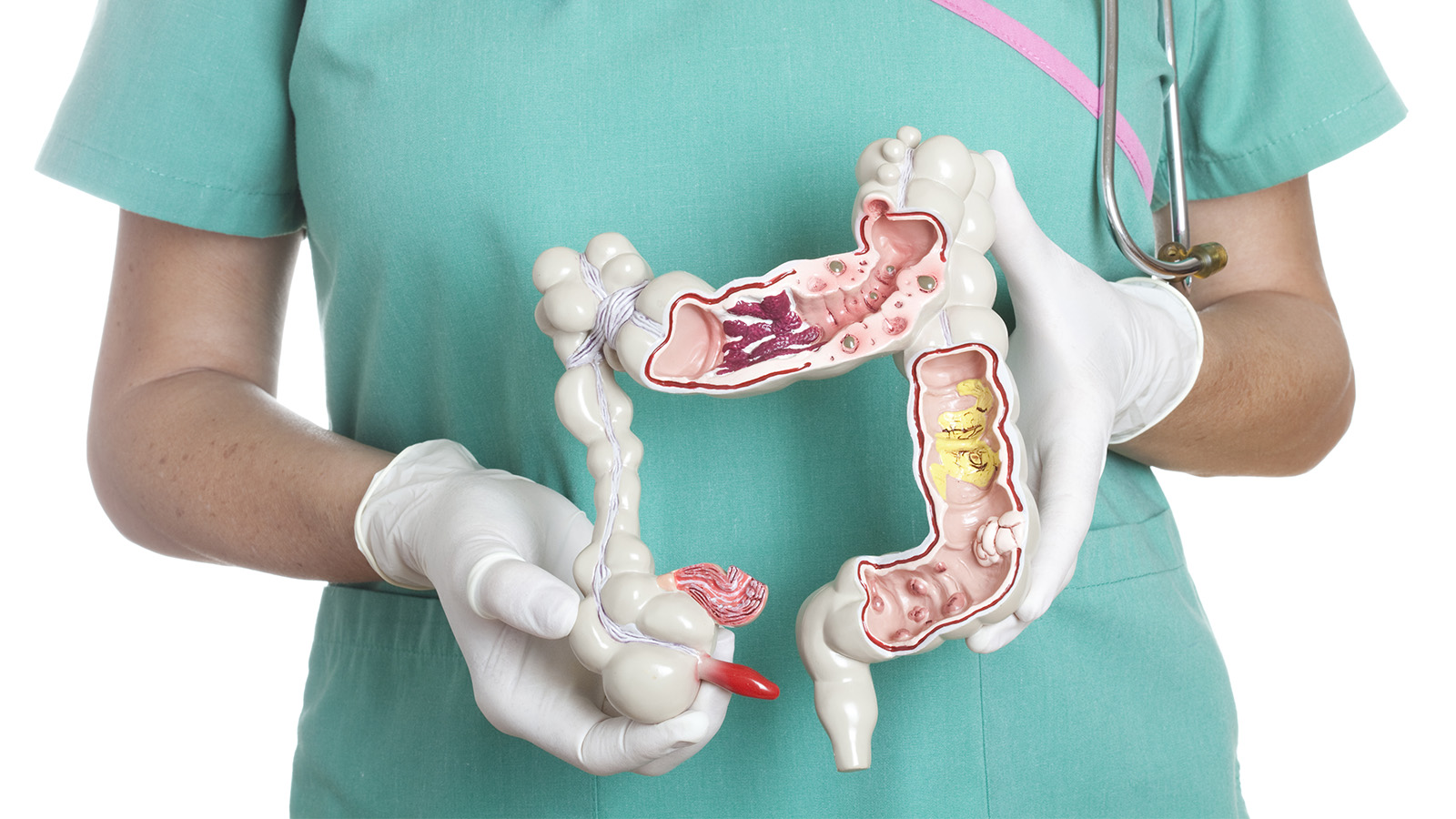
Coeliac disease
Coeliac disease is a common autoimmune disease that affects 1 in 100 people, but only 10–15% are diagnosed. Gluten triggers an immune reaction in people with coeliac disease and gluten damages the lining of the small intestine. Other parts of the body may be affected.
Coeliac disease is more common in people who already have type 1 diabetes, as both are autoimmune conditions and so are genetically linked. Some people with type 1 diabetes find it is only after starting insulin that the symptoms of coeliac disease become noticeable. Some people with type 1 diabetes have a ‘silent’ form of coeliac disease, which means no symptoms are apparent and it is only diagnosed by screening.
There is no link between coeliac disease and type 2 diabetes.
If you think you may have coeliac disease you should:
- Discuss your symptoms with your doctor
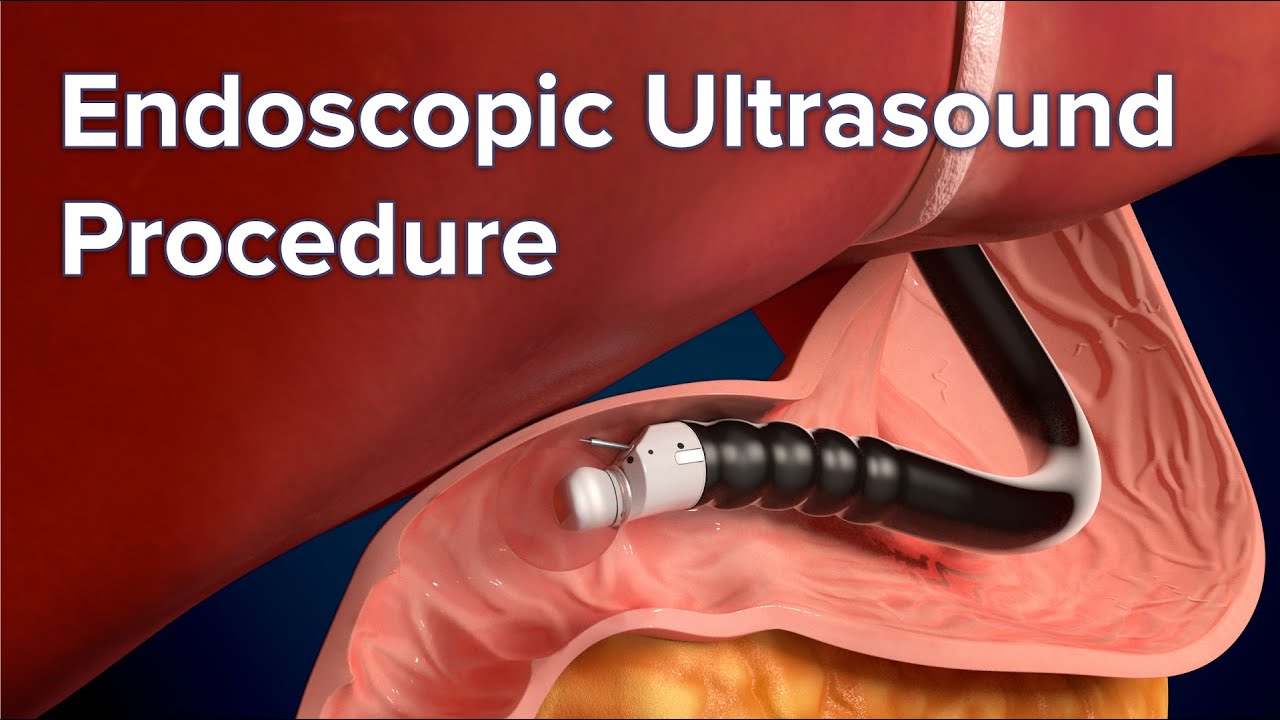
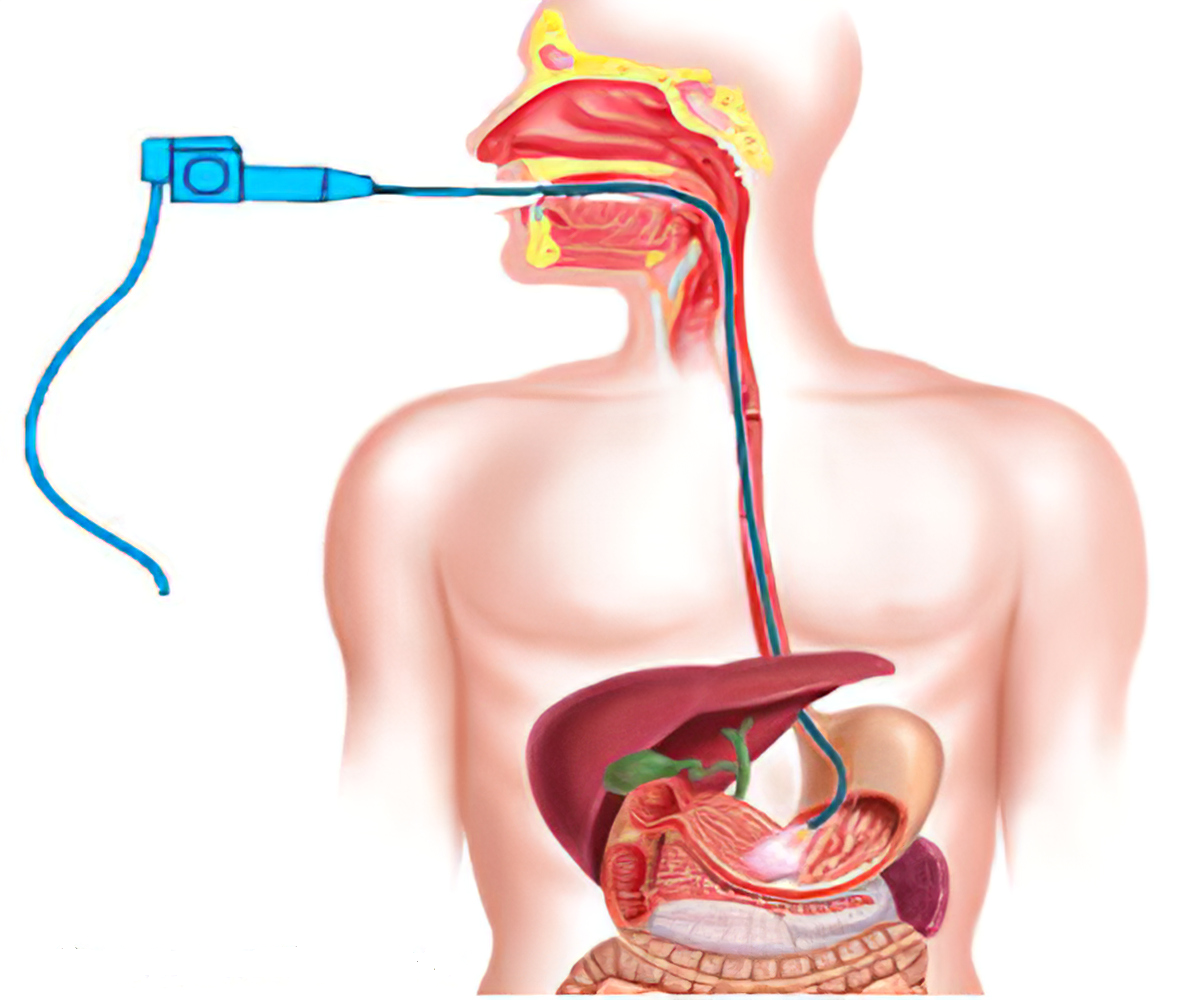
- Your doctor can then take a simple blood test to look for an antibody made by the body in response to eating gluten
- Your doctor can refer you to a gut specialist doctor (gastroenterologist) for a simple test called a ‘gut biopsy’. Small samples of gut lining are collected and later examined under a microscope to check for abnormalities that are typical in coeliac disease.
It is recommended that all children and young people with type 1 diabetes are screened for coeliac disease on diagnosis. It is also recommended that adults with type 1 diabetes are assessed for coeliac disease. Testing should also be offered to anyone if signs and symptoms of coeliac disease are present.
Thyroid disease
There are two types of thyroid disorder: hypothyroidism (where the body doesn’t produce enough thyroid hormones) and hyperthyroidism (where it produces too much).
Thyroid problems are more common in people with diabetes than those without diabetes, especially those with type 1, because the body’s cells can attack the thyroid and destroy the cells as they do the insulin producing cells in the pancreas. Adults and children can be affected, and hypothyroidism is more common in people with type 1. People with type 2 are more likely to develop thyroid problems too, but it’s not clear why this is.
Neither hypothyroidism nor hyperthyroidism can be cured, but both can be treated successfully with tablets.
Polycystic ovary syndrome
Polycystic ovary syndrome (PCOS) affects about 5–10% of women. It can cause an increased risk of developing type 2 diabetes and may increase your risk of heart disease. PCOS is associated with insulin resistance and high levels of insulin circulating in the blood. Around 10–20% of women with PCOS will go on to develop type 2 diabetes at some time.
PCOS is treatable but cannot be cured. Treatment options include maintaining a healthy weight and being physically active, and the drug metformin, which is often prescribed to people with type 2 diabetes.
Diabetes insipidus
Diabetes insipidus is caused when the pituitary gland has a problem producing the hormone vasopressin, also known as AVP, or when the action of AVP no longer works efficiently in the kidneys. This means the body produces increased amounts of urine because the kidneys are unable to retain water.
Diabetes insipidus and diabetes mellitus are separate conditions; very rarely a patient with diabetes mellitus may also develop diabetes insipidus.
Necrobiosis lipoidica diabeticorum
Necrobiosis lipoidica diabeticorum is a skin disorder also known as necrobiosis or NLD and can be associated with diabetes, although not exclusively so. NLD is very uncommon, affecting only 0.3% of all people with diabetes. It most commonly occurs in young adults or early middle age and is three times more common in women as in men. The cause is unknown and it can happen no matter how well the diabetes is managed. NLD usually appears as small, oval, dark red or browny yellow patches with a thick shiny surface, which may be raised above the surrounding skin.
There is no cure, and while there are options for treatment, including steroids, effects can be disappointing.
Mastopathy
Mastopathy is the name given to fibrous (tough) breast tissue, which can develop in people with diabetes. Diabetic mastopathy is uncommon. It is usually seen in women who are pre-menopausal, and who have had type 1 diabetes for many years. Often diabetic mastopathy is associated with other complications of diabetes. It’s not clear what causes diabetic mastopathy, but persistent high blood glucose levels may play a part.
If you notice any lumps or hardness in your breasts you should visit your GP as soon as possible so that s/he can investigate the cause.
Having diabetic mastopathy does not mean that you are at increased risk of breast cancer.
Muscular conditions
Muscular conditions can affect anyone, but people with diabetes are at an increased risk of the following.
Limited joint mobility
Limited joint mobility (also known as diabetic cheiroarthropathy) causes the joints to lose normal flexibility. Although most common in the hands, it can affect wrists, elbows, shoulders, knees, ankles, neck and lower back, and it is associated with microvascular complications of diabetes – nephropathy (kidney disease) and retinopathy (eye disease).
It is treated by keeping blood glucose levels as close to target as possible, but physiotherapy and steroid injections may also be helpful.
Frozen shoulder
Frozen shoulder causes pain, stiffness and limited mobility in the shoulder. It is more common in people who have had diabetes for a long time, are of older age, have had a heart attack or who have the microvascular complications of diabetes (retinopathy and nephropathy). It is treated with painkillers, steroid injections, physiotherapy and, in some cases, surgery.
Dupuytren’s contracture
Dupuytren’s contracture causes contraction of the fingers (particularly the ring and little finger) towards the palm so they cannot be straightened. It is most common in people who have had diabetes for a long time, are of older age, or have the microvascular complications of diabetes. It is generally treated by surgery.
Trigger finger
Trigger finger (also known as stenosing tenosynovitis) is a painful condition that affects the tendons in the hand. When the finger or thumb is bent towards the palm, the tendon gets stuck and the finger clicks or locks. It is most common in the ring finger. It is more common in people who have had diabetes for a long time, are of older age, or who have retinopathy or nephropathy. It is treated with steroid injections, splinting the finger or, in some cases, surgery.
Carpal tunnel syndrome
The symptoms of carpal tunnel syndrome include pain, numbness or pins and needles in the hand and wrist, particularly the thumb, forefinger and middle finger. The pain (often described as a tingling or burning sensation) is often worse at night. It is treated by splinting the wrist, steroid injections and, in some cases, surgery.
Dental health problems
Dental problems are more common in people with diabetes. It is estimated that people with type 2 diabetes are three times more likely to develop dental problems than people without diabetes, and the risk is also increased for people with type 1.
Oral problems can occur in people with diabetes for a number of different reasons, which is why it is especially important to visit a dentist regularly and tell them about your diabetes. People with diabetes who have persistent high blood glucose levels are more likely to have dental problems.
Haemochromatosis
Haemochromatosis is when there’s too much iron in the blood and that can lead to diabetes. This type of diabetes is secondary diabetes and is like type 1.
Insulin resistance and severe insulin resistance
Insulin resistance (IR) occurs when the cells of the body do not respond properly to insulin. This means the insulin produced by the pancreas cannot be used effectively. People with IR may need a much larger amount of insulin or other insulin sensitising medications to reach and stay within their blood glucose (sugar) targets.
The most common cause of IR is obesity, but some other rare conditions can cause IR and sometimes even severe insulin resistance (SIR). Rare conditions causing SIR include insulin receptor mutations, insulin receptor antibodies and lipodystrophy (abnormal fat distribution). Both IR and SIR are more severe in puberty and pregnancy and may be picked up at these times.
Whilst IR and SIR doesn’t always lead to diabetes, diabetes is a common outcome of the condition because the pancreas is unable to produce enough insulin and blood sugar levels rise. Despite this, it is important to recognise that IR and SIR is not the same as diabetes. If the pancreas is able to produce enough insulin to overcome the resistance, then diabetes does not develop.
Weight loss, healthy eating and exercise and the medications metformin and pioglitazone can improve IR and SIR. Some patients with SIR need specialised therapies including metreleptin therapy, immunosuppression, highly concentrated insulin therapy or a combination of the three.
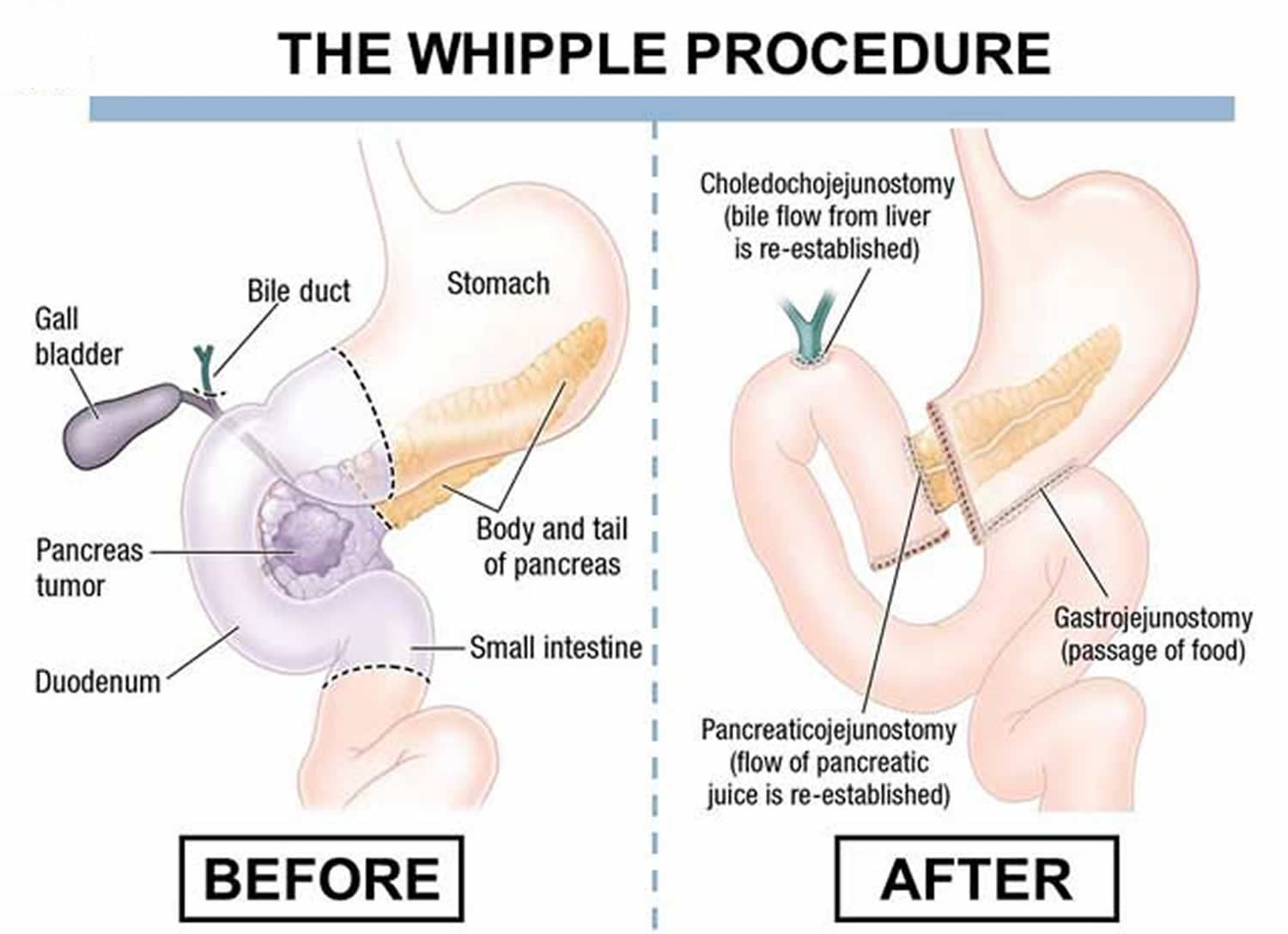
Pancreatitis
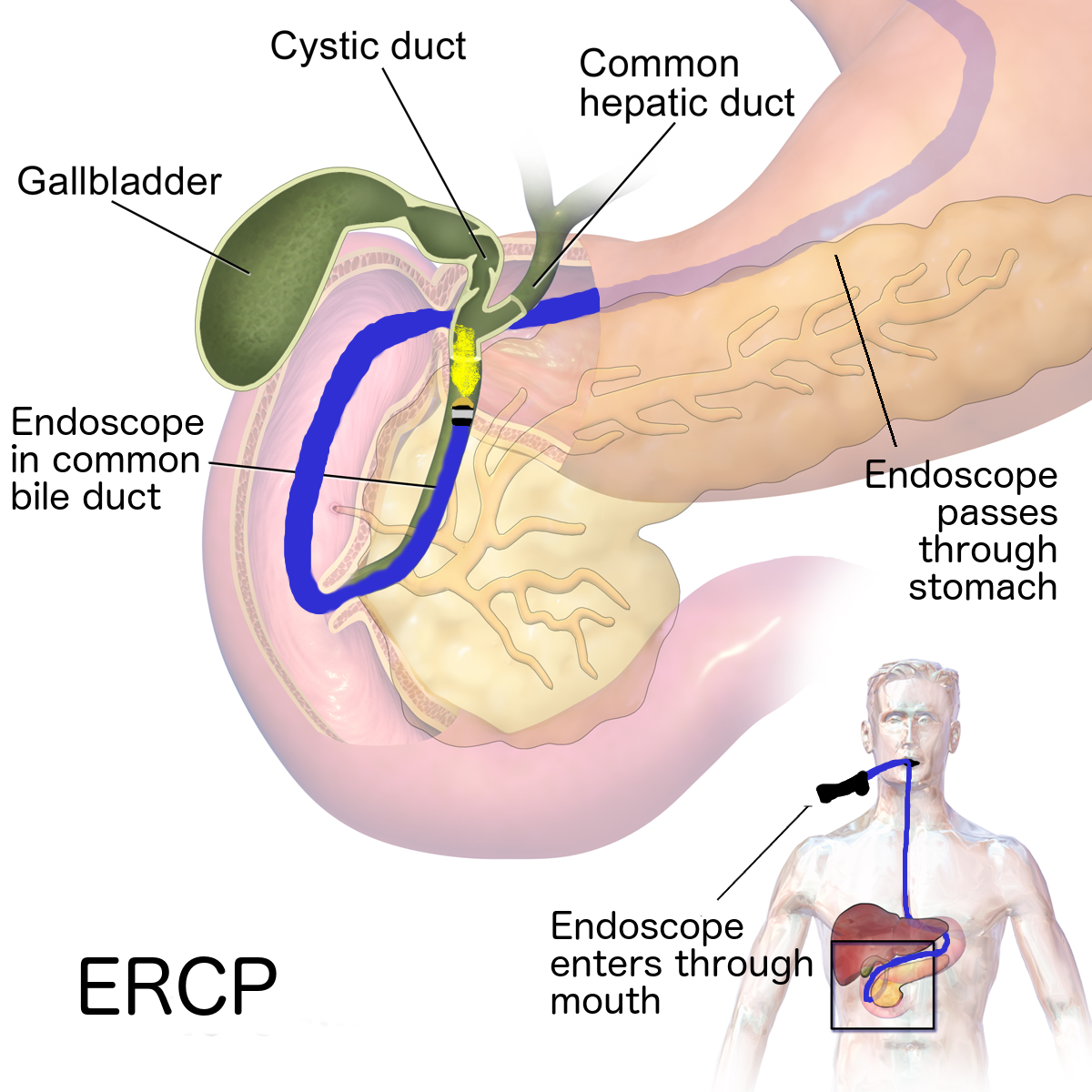
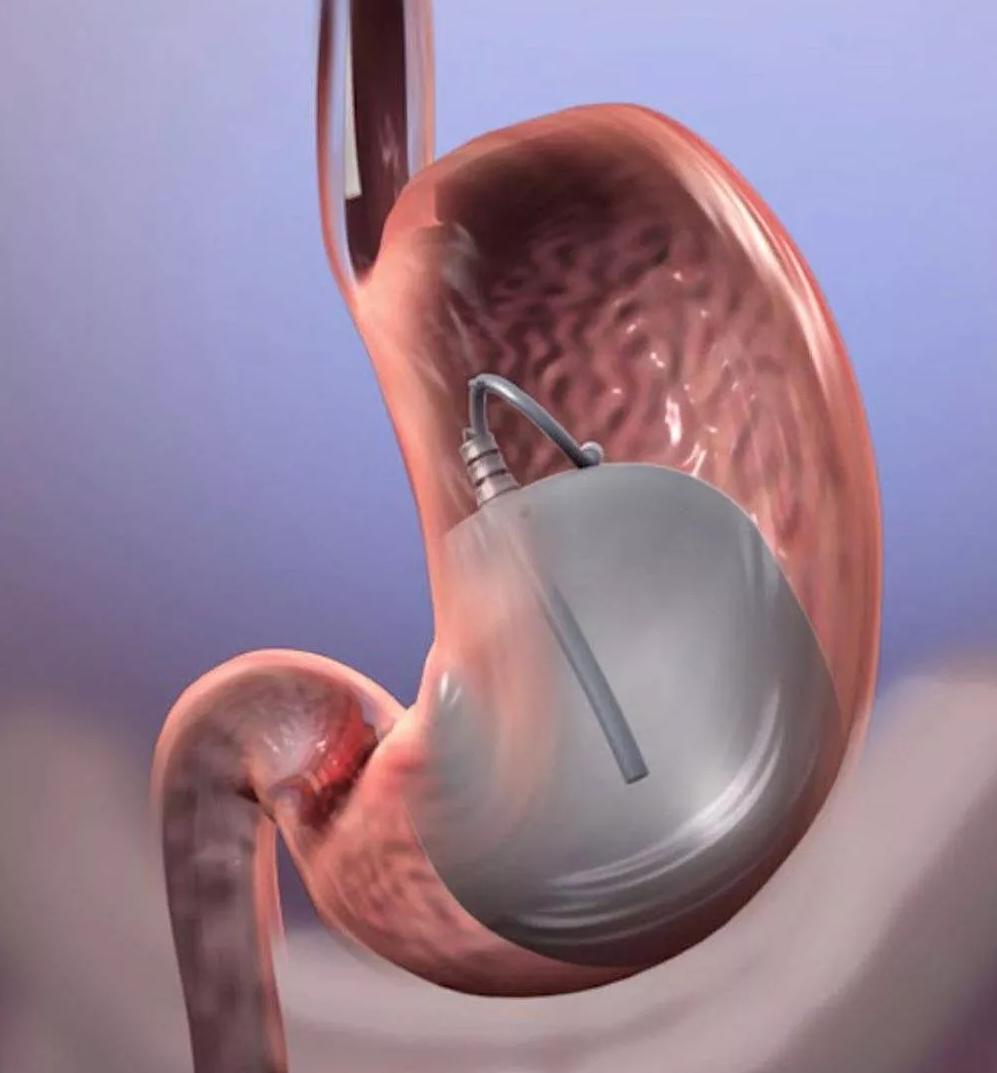
Pancreatitis occurs when your pancreas, the small organ located behind your stomach in your abdomen, becomes inflamed. This could lead to type 3c diabetes.
Your pancreas produces the hormone insulin, which regulates your body’s blood glucose (sugar) level. It also produces digestive enzymes, which help you to digest your food.
There are two types of pancreatitis, acute pancreatitis and chronic pancreatitis.
Acute pancreatitis
Acute pancreatitis is where your pancreas suddenly becomes inflamed over a short period of time. Common signs and symptoms of acute pancreatitis include:
- Severe pain in your tummy (abdomen)
- Feeling or being sick
- Difficulty digesting food
- Diarrhea
You may need treatment in hospital, but you should be able to recover fully in a few days if your condition is not severe.
Chronic pancreatitis
If your pancreas stays inflamed over time, the cells may become permanently damaged and stop working properly. This is called chronic pancreatitis. In addition to the symptoms of acute pancreatitis, the common signs and symptoms of chronic pancreatitis also include:
- Oily stools
- Losing weight without trying to
It’s important that you are aware of these symptoms so you can get the treatment you need as soon as possible.
Almost 1 in 3 people with chronic pancreatitis go on to develop type 3c diabetes. This is because the damaged cells prevent the pancreas from producing enough insulin.
If you have experienced acute pancreatitis more than once, or if you notice any of the symptoms of diabetes, consult a doctor for more information and advice.
Reference
- https://www.nhs.uk/conditions/chronic-pancreatitis/
- https://www.diabetes.org.uk/diabetes-the-basics/related-conditions
- https://www.nia.nih.gov/health/diabetes-older-people
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4673801/
- https://www.cdc.gov/diabetes/basics/diabetes.html
- https://www.mayoclinic.org/diseases-conditions/diabetes/symptoms-causes/syc-20371444
- https://www.nhs.uk/conditions/type-2-diabetes/health-problems/