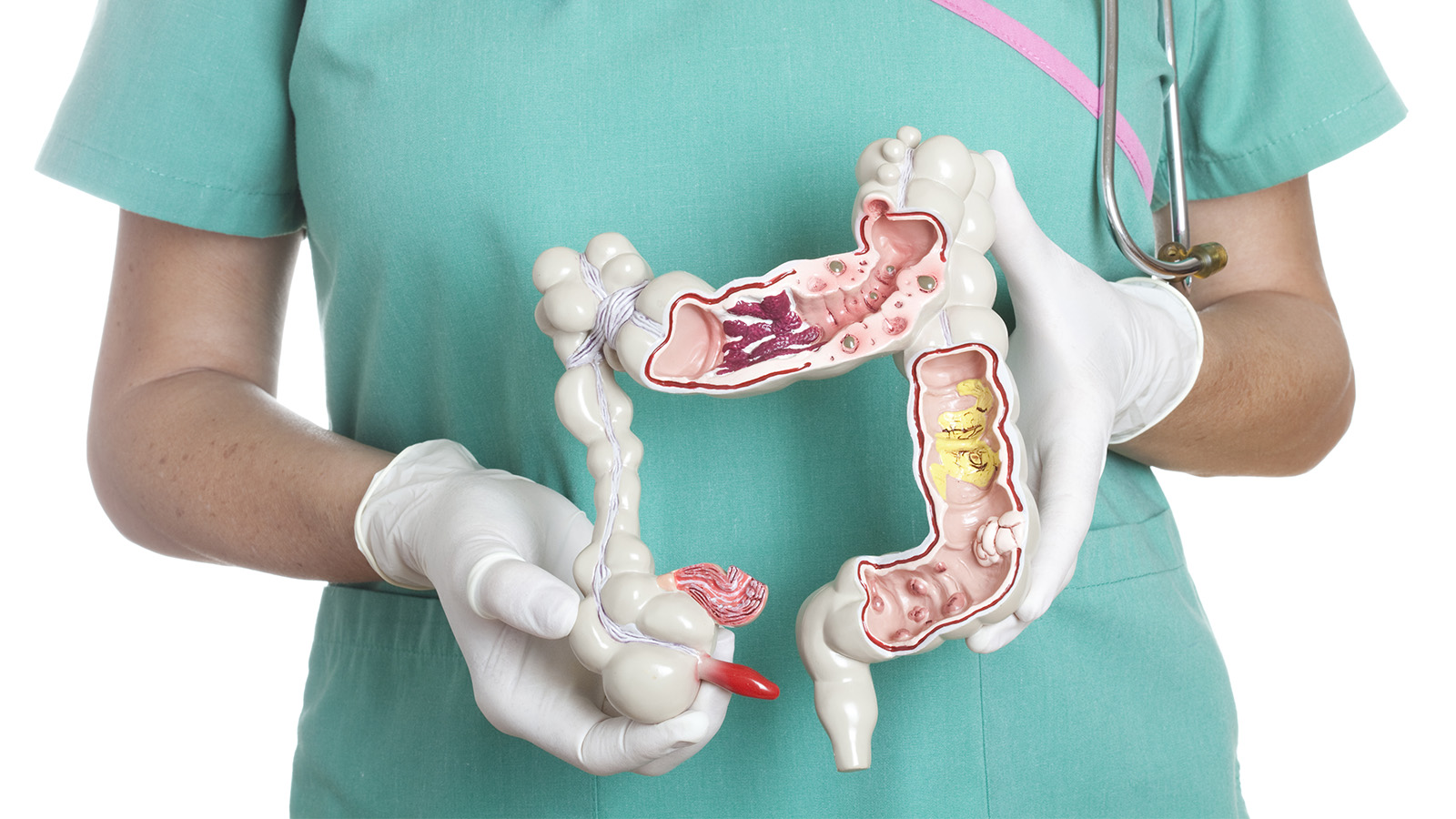
Enterocolitis
OVERVIEW | CAUSES | RISK FACTORS | SYMPTOMS | COMPLICATION | DIAGNOSIS | TREATMENT | PREVENTION | REFERENCES
OVERVIEW
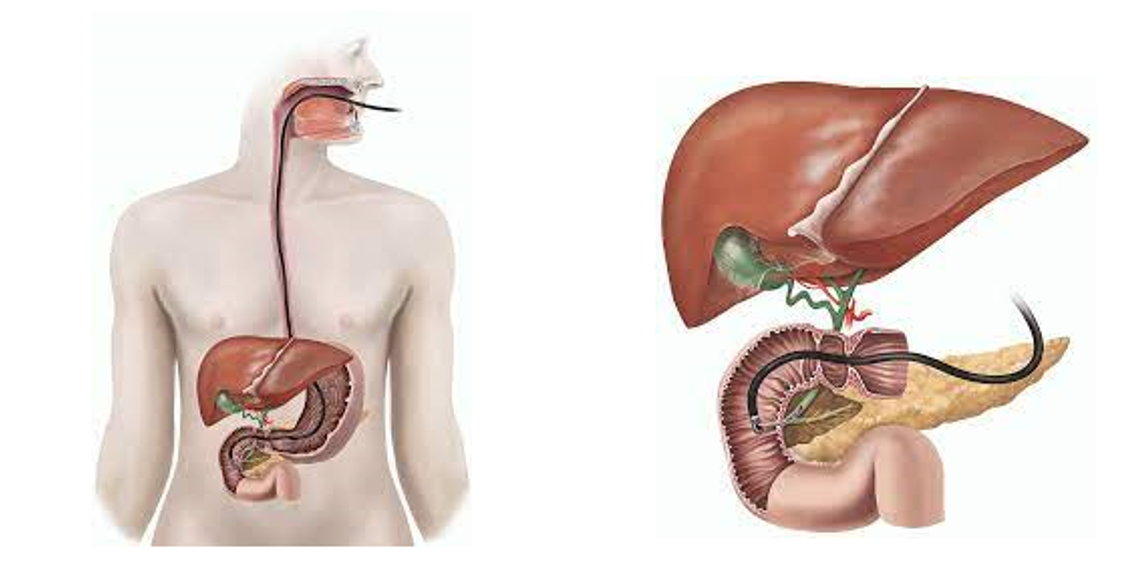
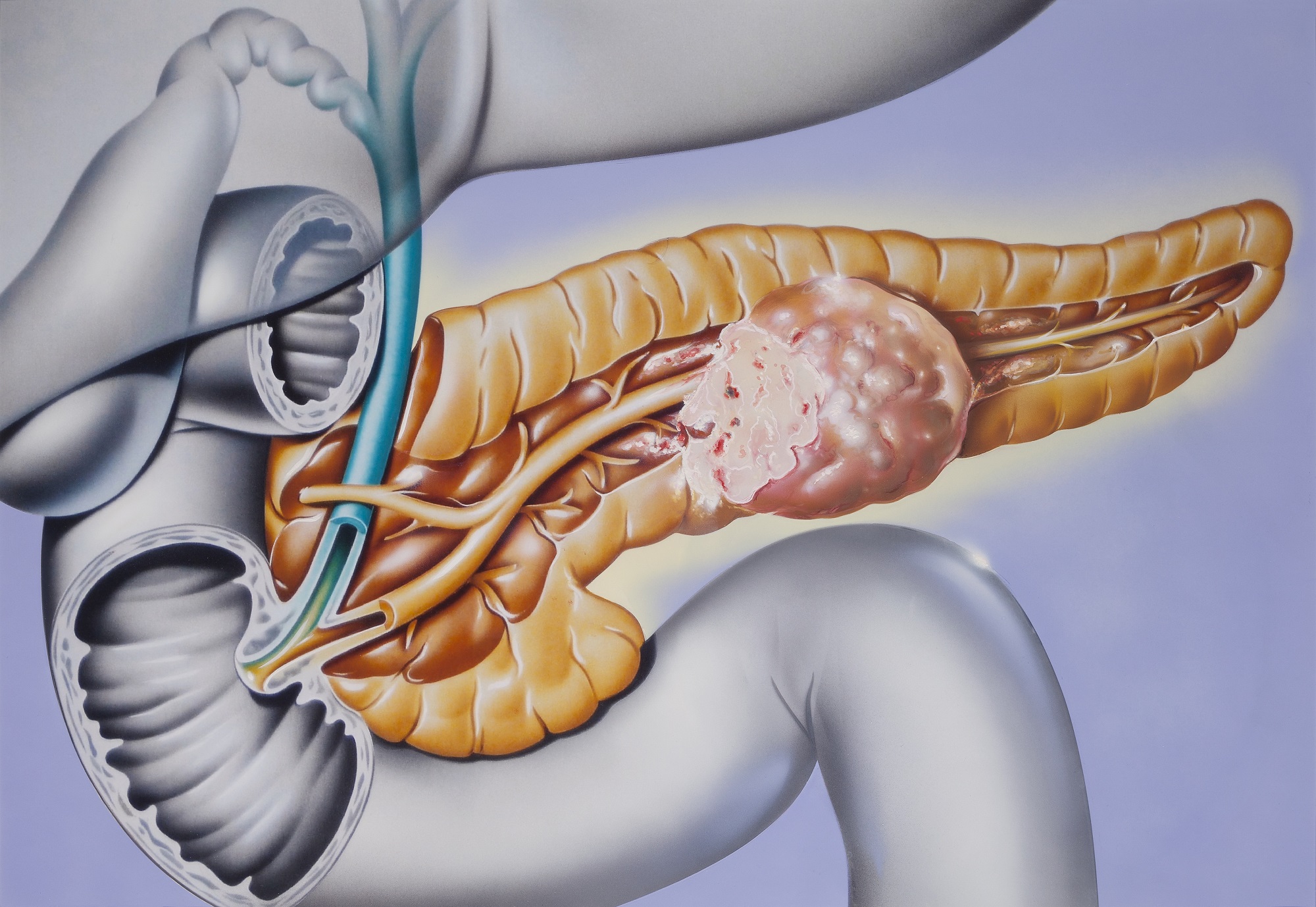
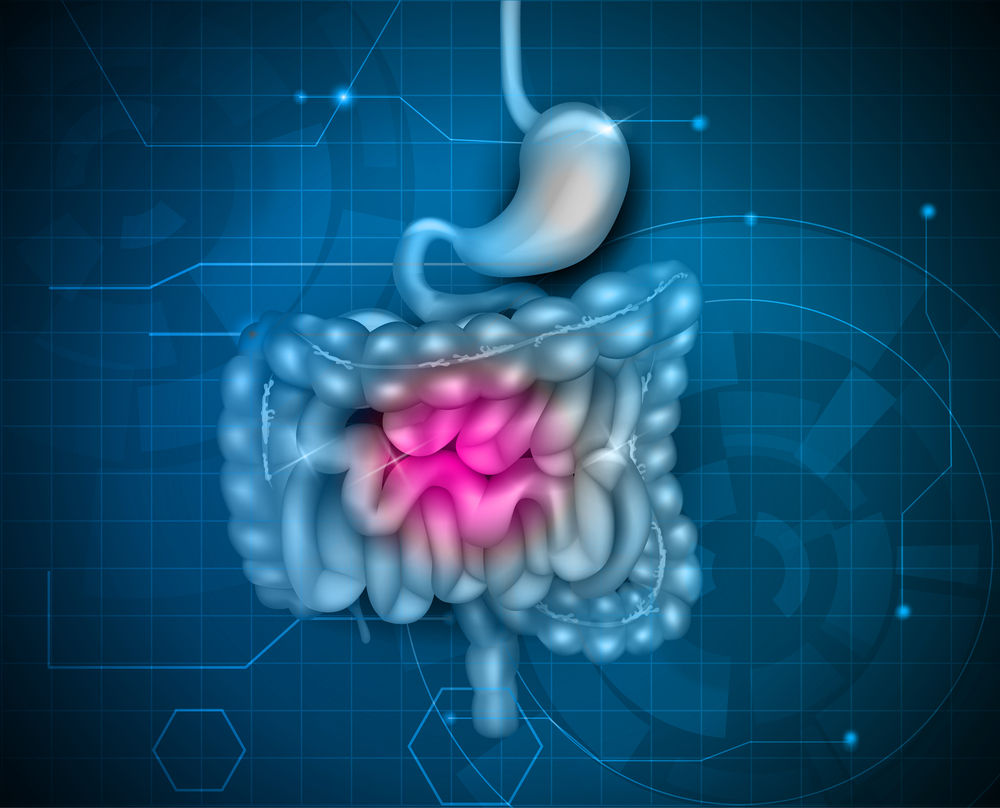
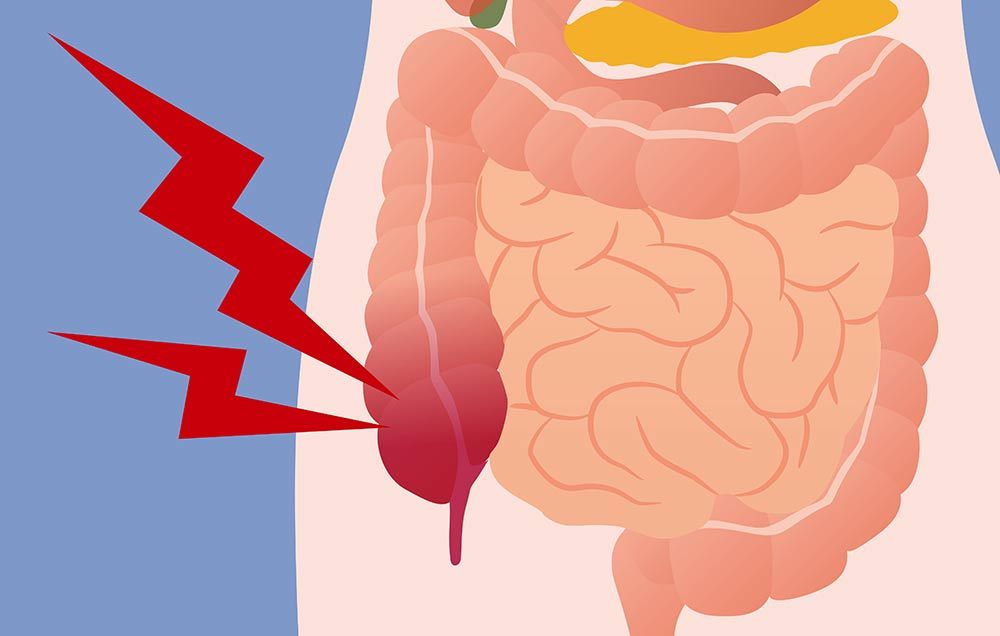
Enterocolitis means inflammation in the digestive tract including both the small intestine and the large intestine or colon. The word “Enteritis'' specifically refers to an inflammation of the small intestine and the word “colitis” specifically refers to inflammation of the large intestine. It occurs in both adults and children but infants and pre-term babies are more commonly affected.
There are different types of enterocolitis, distinctive in their symptoms and the mode of causes. They are as follows:
1. Necrotizing enterocolitis (NEC)
It is one of the most frequently occurring diseases in neonates or pre-term births. It occurs in 5–10% of very low birth weight infants (less than 1500 gms). Statistics show mortality rates ranging from 15% to 30% in infants. It is commonly described as inflammation accompanied by the death of tissues in the lining of the intestine. The etiology generally includes formula feeding, genetic variations, intestinal immaturity, altered microvascular tone, abnormal microbial growth and highly immune-reactive intestinal mucosa. Study show that histologic Chorioamnionitis (Inflammation of fetal membranes) is associated with a 2.5 times higher risk of necrotizing enterocolitis. Early signs include dilated loops of bowel, a paucity of gas, and gas-filled loops of bowel that may progress rapidly as abdominal discoloration and intestinal perforation.
2. Antibiotic-associated enterocolitis (also known as Pseudo-membranous colitis)
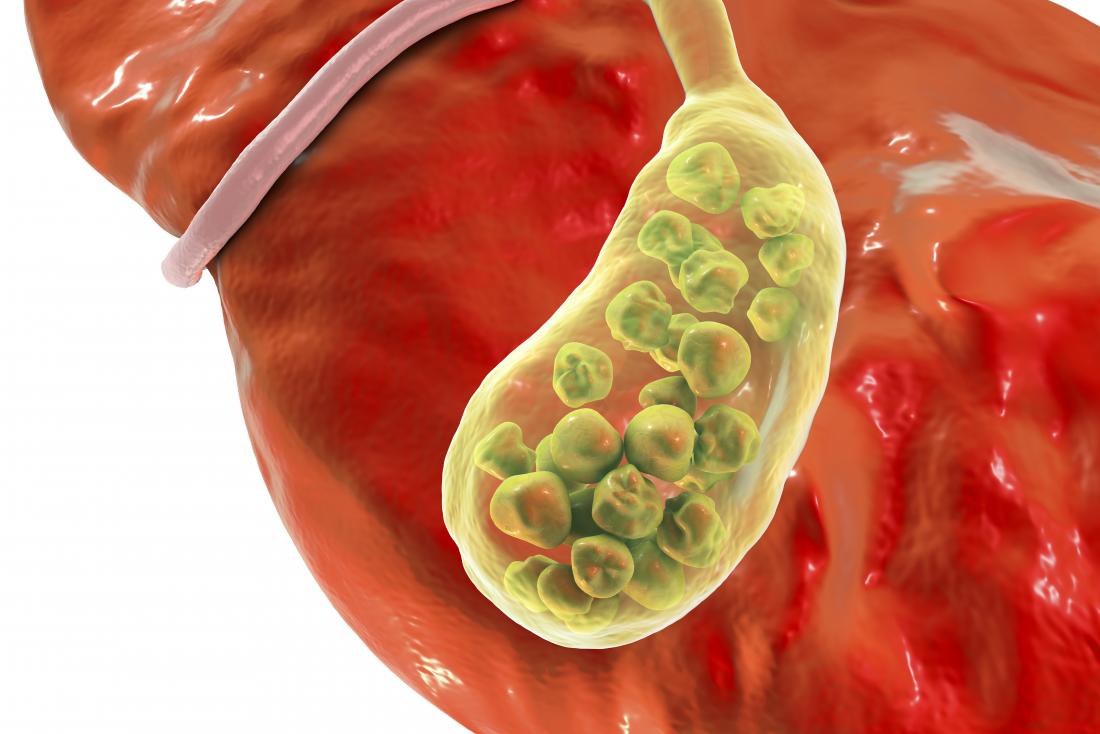
Antibiotic therapy is widely used today for the prevention of a number of diseases, but it is associated with a major risk factor for the development of diarrhea and colitis. The use of antibiotics may result in severe depletion of the endogenous gastrointestinal microbiota. These microbiotas are helpful in breaking down and digesting food, and their deficiency creates an environment for bacteria such as Clostridia difficile and Klebsiella oxytoca to infect. The bacterium releases a toxin that causes inflammation and bleeding in the lining of colon and also alters the homeostasis of the gastrointestinal tract. Antibiotics like Methotrexate, Dexamethasone and Prednisolone have been reported to cause antibiotic-associated enterocolitis.
3. Hemorrhagic enterocolitis
This type of enterocolitis is so named due to its usual manifestation as bloody diarrhea. E.coli mainly cause a severe infection in both young children and geriatric patients who have an increased attack rate for E. coli infection. The bacterium adheres to the intestinal mucosa and produces cytotoxins (also referred as Shiga-like toxins). It can spread by touching an infected animal, eating or drinking contaminated water or unpasteurized milk.
4. Hirschsprung-associated enterocolitis (HAEC)
It is a life-threatening complication of Hirschsprung disease which usually manifests as abdominal distension, foul diarrhea, along with emesis, fever, lethargy, and even shock. Failure to recognize HD in the early perinatal period may increase the risk of HAEC in children.
CAUSES
Enterocolitis may be caused by a variety of infectious agents including bacteria, viruses, fungi and parasites. It is often caused by eating or drinking contaminated foods.
- Bacterial agents include: Salmonella, E.coli, and Shigella.
- Viral agents include: Rotaviruses, enteroviruses, and adenoviruses.
- Parasitic agents may cause giardiasis, and amebic dysentery.
Enterocolitis may also be caused by:
- An autoimmune condition, such as Crohn’s disease.
- Medications or drugs including ibuprofen, naproxen sodium, and cocaine.
- Damage from radiation therapy.
- Celiac disease.
- Immunno-suppressed patients.
RISK FACTORS
While there appears to be no single cause of enterocolitis, in case of infants, risk factors include premature birth and early feedings in premature babies with an immature gut. Babies who have had difficult deliveries with lowered oxygen levels can also develop enterocolitis.
SYMPTOMS
The common signs and symptoms of Enterocolitis include:
- Diarrhea
- Nausea and vomiting
- Loss of appetite
- Abdominal cramps and pain
- Pain, bleeding, or mucus-like discharge from the rectum
- Fever
- Tiredness
- Swollen Abdomen
COMPLICATIONS
If symptoms are severe then the patient is at an increased risk of dehydration. Especially infants and young children are more vulnerable to dehydration. So, one should contact a medical professional immediately in case of following symptoms:
- Dehydration
- Diarrhea that does not go away in 3-4 days
- Fever over 101 degrees F
- Blood in the stools
DIAGNOSIS
To confirm a diagnosis of enterocolitis, the following examinations or tests may be used:
Physical examination
During the exam, the doctor examines the baby’s abdomen to check for swelling, pain, and tenderness.
Stool culture or stool tests
A stool culture is done to determine the type of infection. Other stool tests used are:
- Gram stain of stool
- Fecal smear
- Stool ova and parasites exam
- Serological tests
These tests help to check for antibodies in the blood that can cause various disease conditions. They can involve a number of laboratory techniques. Different types of serologic markers including C-reactive protein, platelet-activating factor and intestinal fatty acid binding protein are used in the diagnosis. Complete blood count is also used to check the presence of neutropenia. Blood culture also helps to find out any fungal infection that may cause sepsis.
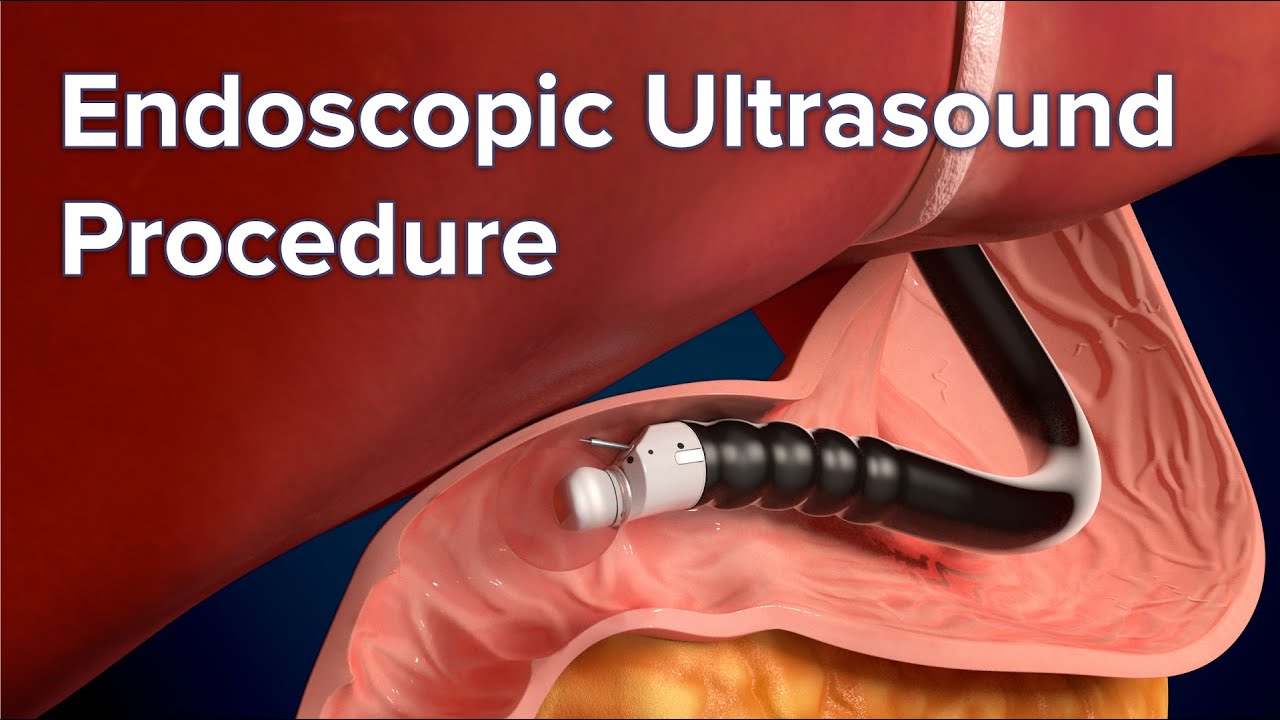
Abdominal ultrasound
Abdominal ultrasonography is a useful tool in an early detection of complications. It gives clear insight of bowel wall i.e. its thickening or thinning, reduced peristalsis or disturbed bowel wall perfusion. It also helps to determine the exact status of intra-abdominal fluid. Bowel wall thickening of more than 5mm has been reported to cause a higher mortality rate.
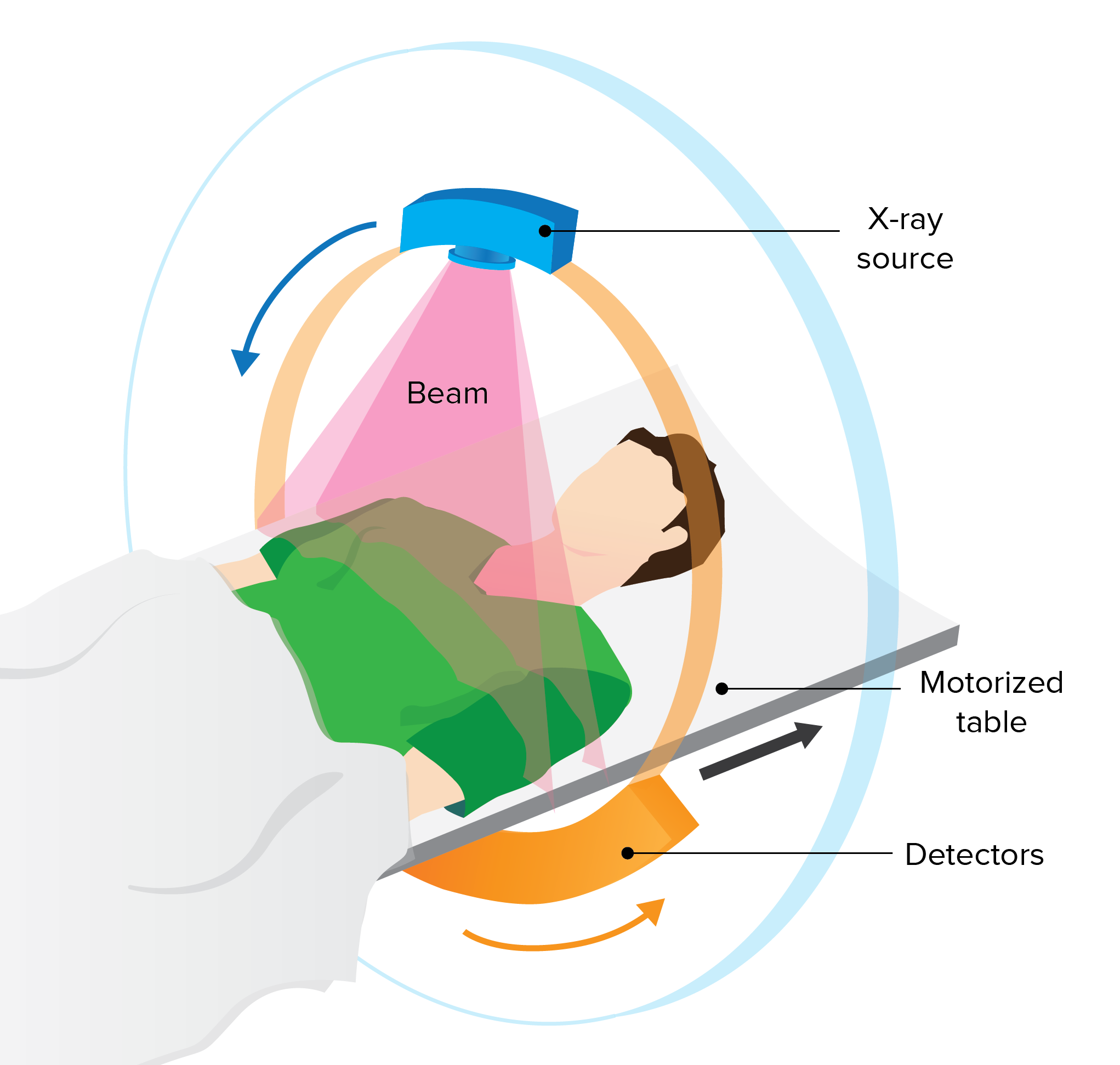
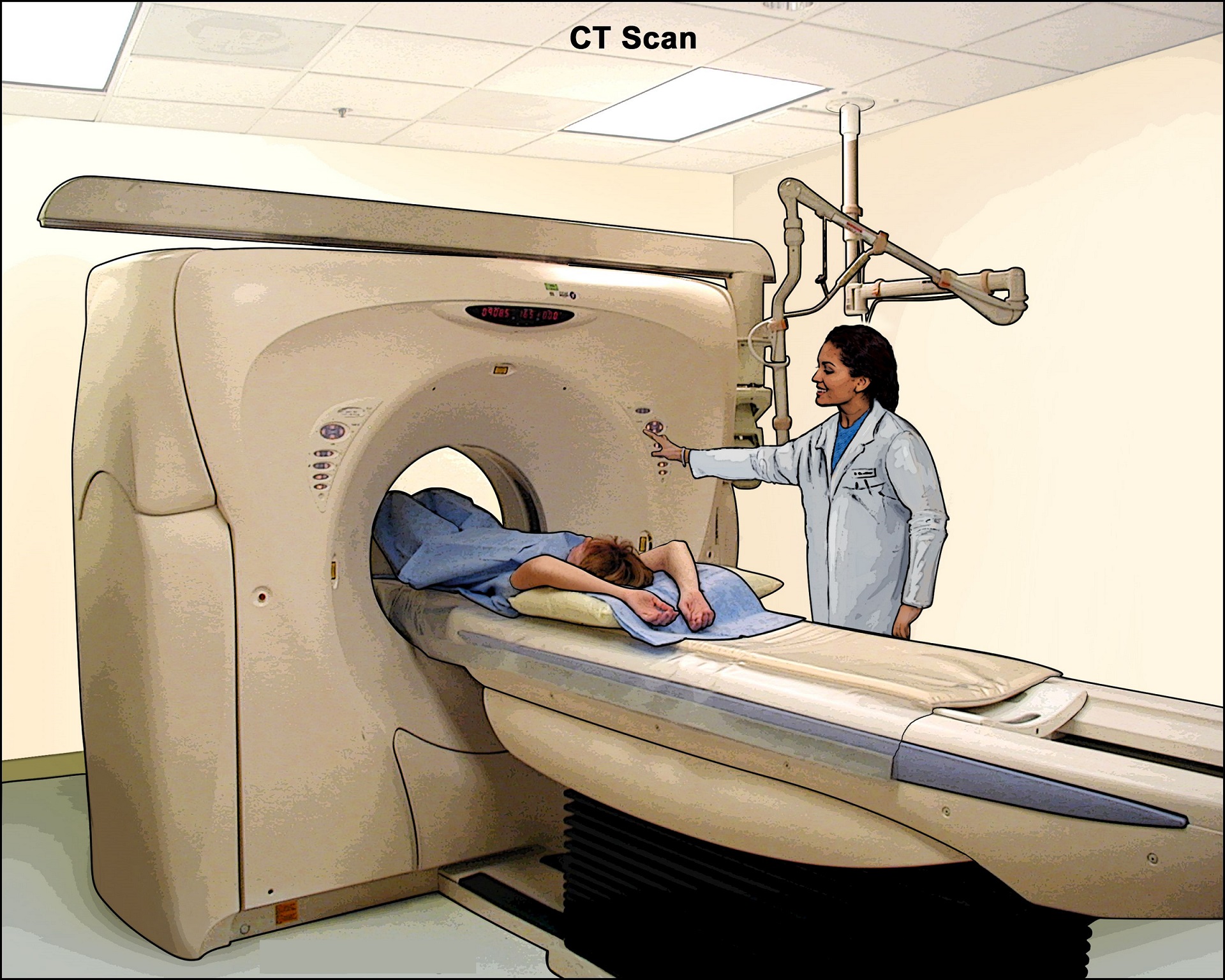
Imaging techniques
The doctor may also opt for an imaging technique. CT scan allows checking for thickening in the cecum, pericecal inflammation, and an air-filled perforation. Abdominal radiographs have been widely used for diagnosing neutropenic enterocolitis.
TREATMENT
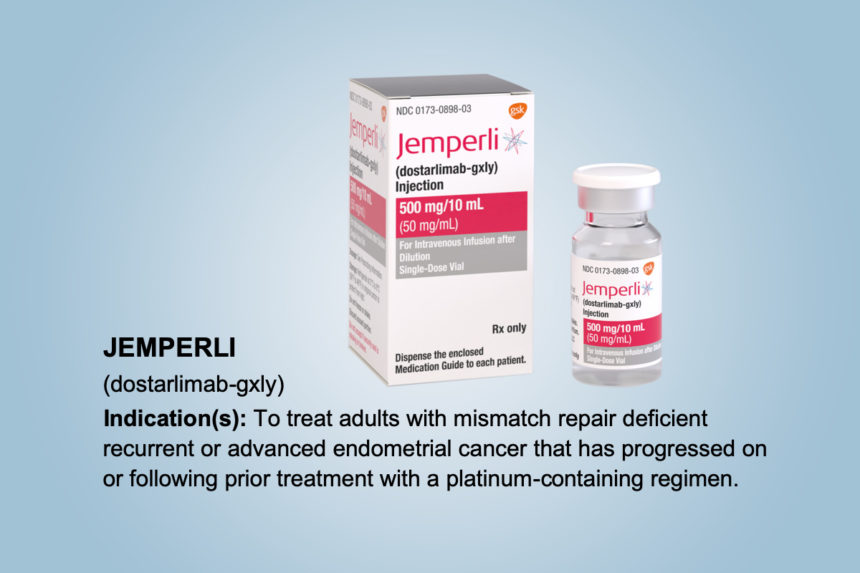
In general, patients with enterocolitis require a therapy of broad-spectrum antibiotics and IV fluid resuscitation. Immediate medical management and introduction of antibiotic treatment is a crucial measure to decrease morbidity and mortality in patients infected with enterocolitis.
In the treatment of necrotizing enterocolitis, cessation of formula feedings, nasogastric decompression, and intravenous fluid resuscitation are commonly used.
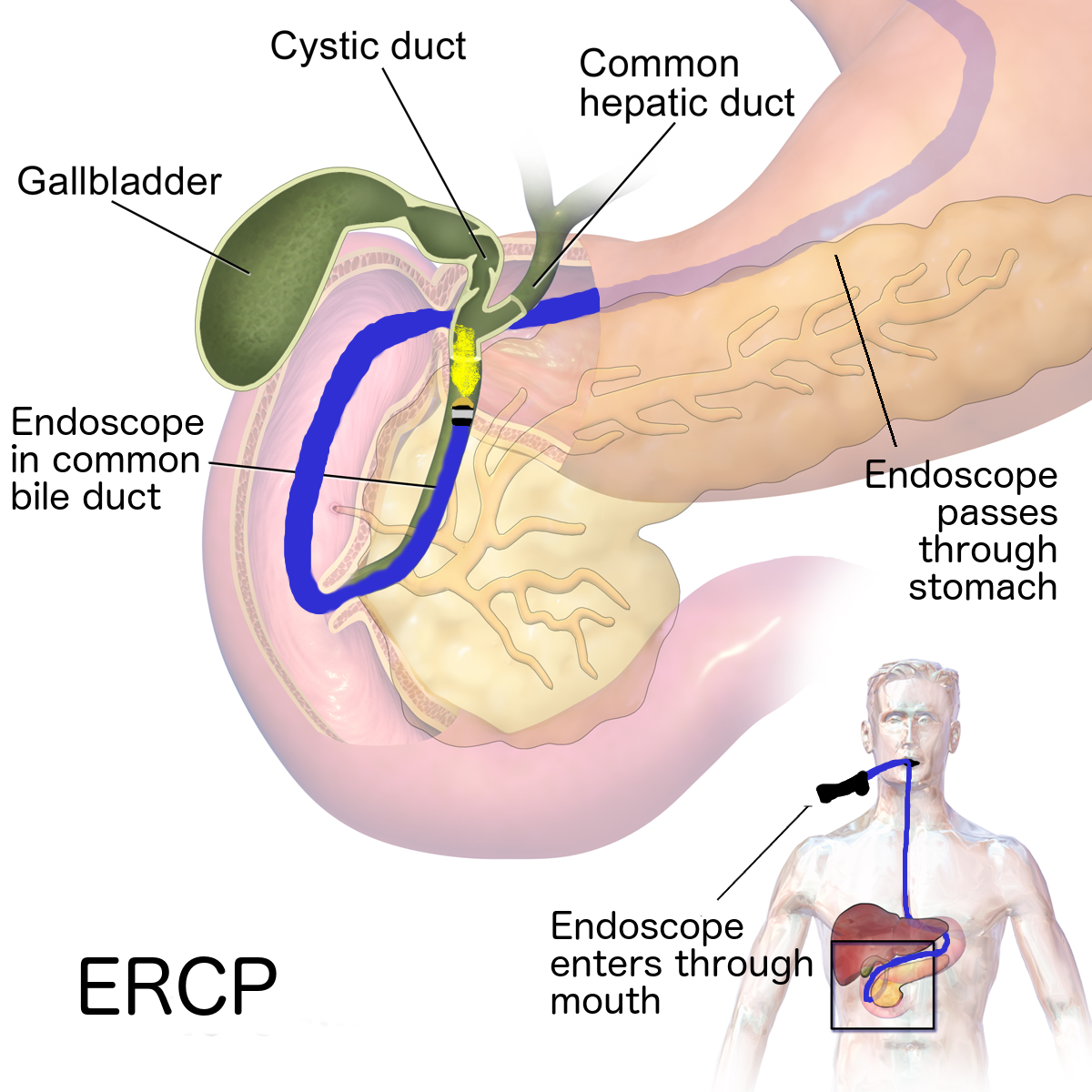
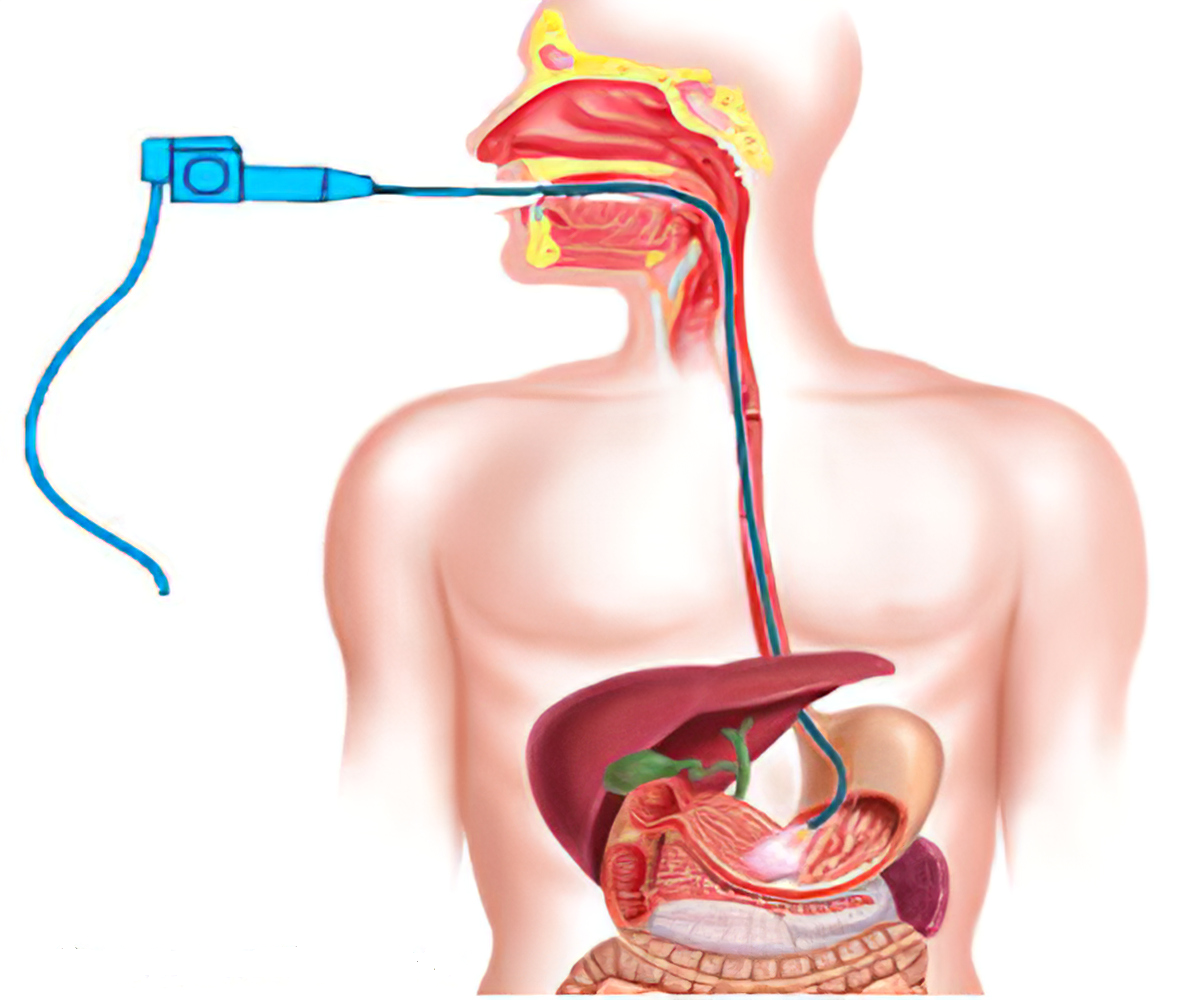
Nasogastric decompression- In this technique, a nasogastric tube is used to decompress the stomach and remove gas and fluid from it. Gastric lavage basically irrigates the stomach and helps to remove ingested toxins.
Intravenous fluid resuscitation- It is an effective therapy in case of dehydration as a result of enterocolitis. It compensates the loss of fluid and maintains electrolyte balance in the body.
- In the treatment and prevention of antibiotic-associated enterocolitis use of non-pathogenic living organisms has been reported which are capable of re-establishing the equilibrium of the intestinal ecosystem. For example, S. boulardii has shown its effectiveness and safety by decreasing significantly the occurrence of C. difficile colitis and preventing the pathogenic effects of toxins.
- Antibiotics and antimicrobials are important therapies in case of Hirschsprung-associated enterocolitis. Drugs like Ampicillin, Gentamicin and Metronidazole are widely used. In case of recurrent Hirschsprung-associated enterocolitis, Sodium cromoglycate (a mast cell stabilizer) has been reported to give positive results.
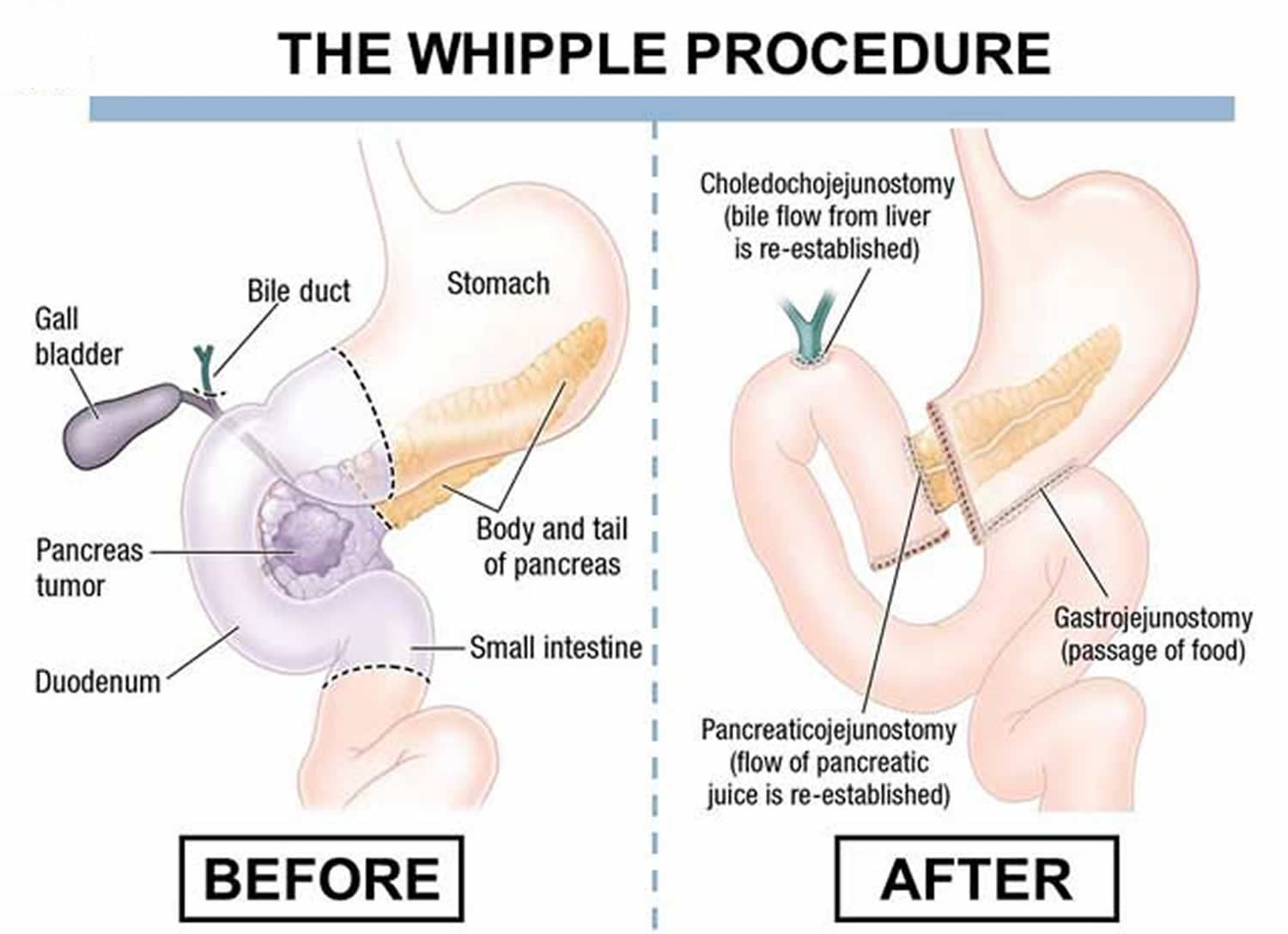
Surgical treatments- Despite medical management and supportive care, operative management is needed when the symptoms are severe, which includes either laparotomy or placement of a percutaneous peritoneal drain. In peritoneal drainage technique a permanent peritoneal catheter is used to remove abdominal fluids and reduce symptoms. In laparotomy, a surgical incision is done in the abdominal cavity. Through laparoscopy the abdominal cavity can be examined closely and proper treatment can be done.
The following measures are helpful in the prevention of enterocolitis:
- Always maintain proper personal hygiene.
- Always wash your hands after using the toilet and before consuming or preparing food or drinks.
- Use of Probiotics -For prophylactic prevention, probiotics (containing potentially beneficial bacteria or yeast) mainly Lactobacillus, Bifidobacterium, Saccharomyces, and Streptococcus sp. have been reported to be beneficial in children with necrotizing enterocolitis.
- Keep the children clean and change their diapers from time to time and dispose them off properly.
- Drink ample quantity of fluids.
- Always drink filtered or purified water and avoid drinking water from streams and outdoor wells.
- Use clean utensils for eating or handling foods.
- Use good quality poultry products.
REFERENCE
- https://www.chp.edu/our-services/transplant/liver/education/liver-disease-states/necrotizing-enterocolitis
- https://my.clevelandclinic.org/health/diseases/23049-enteritis-inflammation-small-intestine
- https://my.clevelandclinic.org/health/diseases/10026-necrotizing-enterocolitis
- https://medlineplus.gov/ency/article/001148.htm