Eosinophilic Esophagitis
OVERVIEW | CAUSES | RISK FACTORS | SYMPTOMS | COMPLICATION | DIAGNOSIS | TREATMENT | PREVENTION | REFERENCES
OVERVIEW
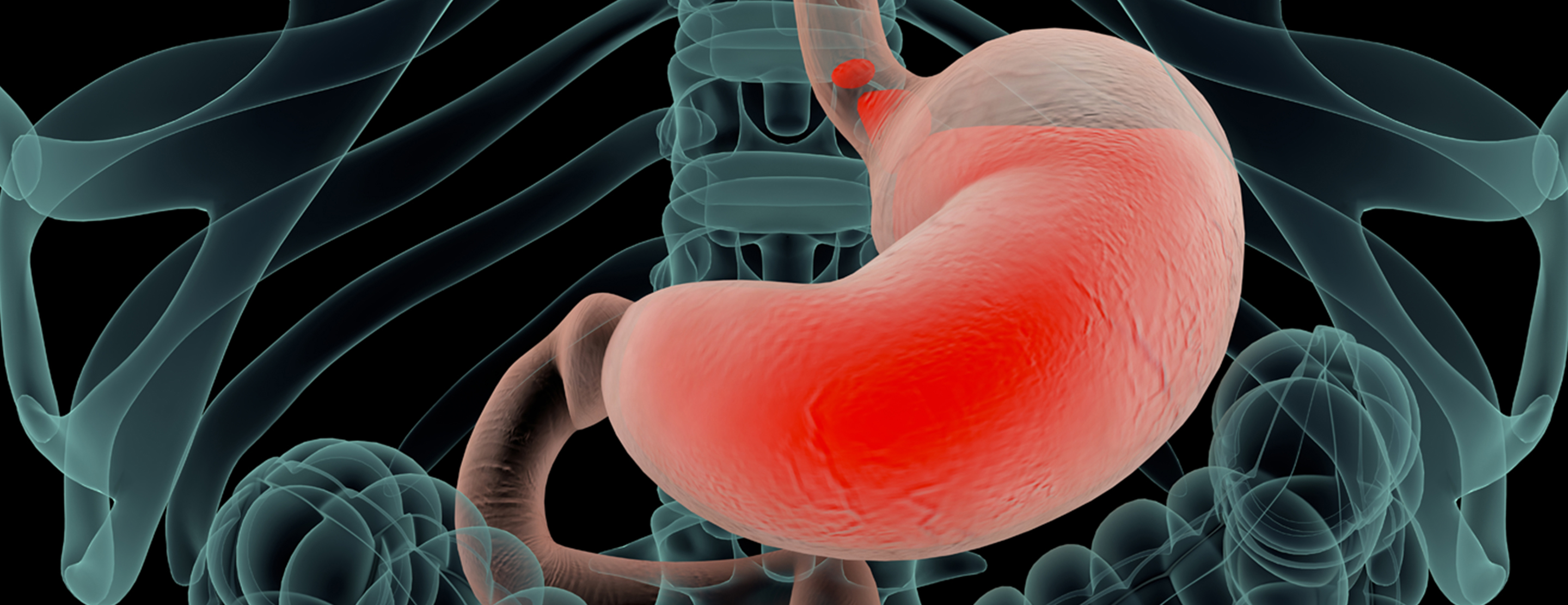
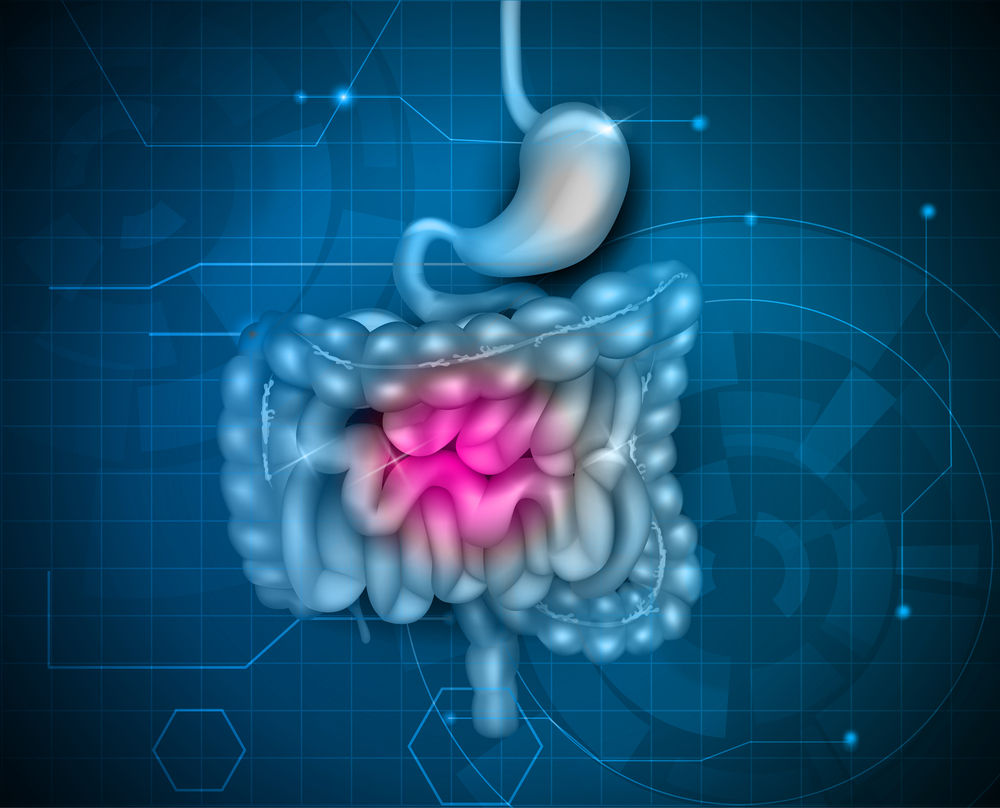
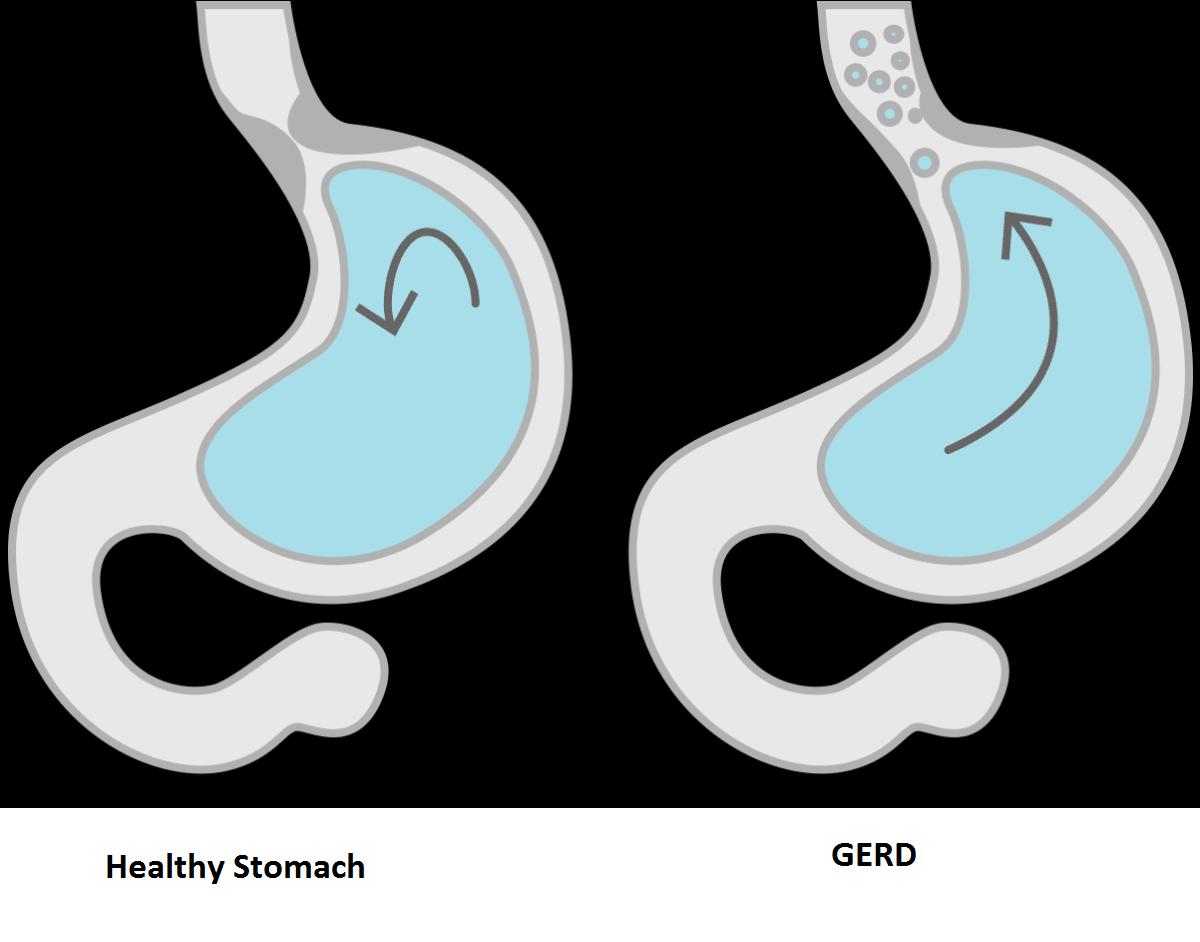
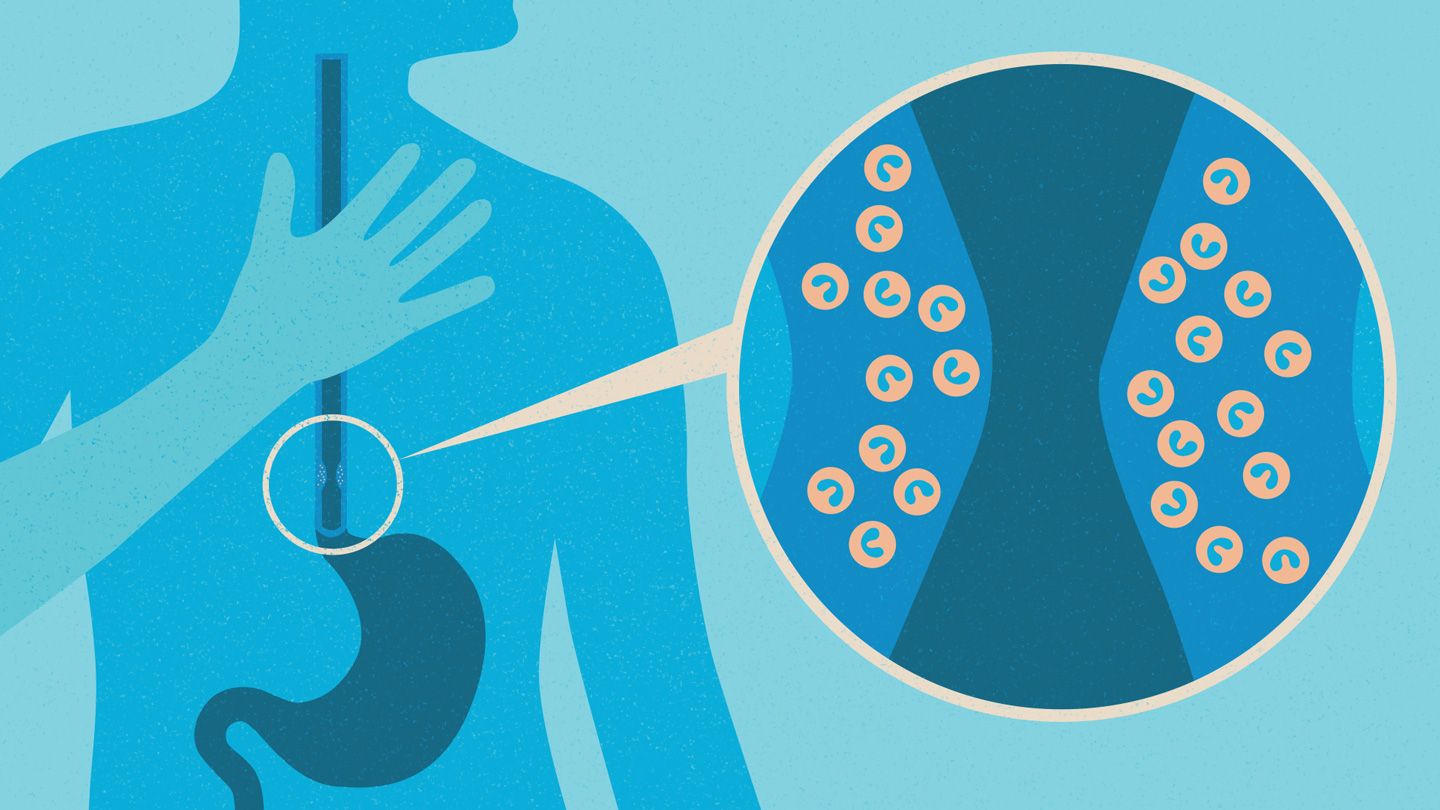
Eosinophilic esophagitis is a chronic immune system disease in which a type of white blood cell (eosinophil) builds up in the lining of the tube that connects your mouth to your stomach (esophagus). This buildup, which is a reaction to foods, allergens or acid reflux, can inflame or injure the esophageal tissue. Damaged esophageal tissue can lead to difficulty swallowing or cause food to get stuck when you swallow.
Eosinophilic esophagitis has been identified only since the early 90s, but is now considered a major cause of digestive system (gastrointestinal) illness. Research is ongoing and will likely lead to revisions in the diagnosis and treatment of eosinophilic esophagitis.
CAUSES
Eosinophils are a normal type of white blood cells present in your digestive tract. However, in eosinophilic esophagitis, you have an allergic reaction to an outside substance. The reaction may occur as follows:
- Reaction of the esophagus. The lining of your esophagus reacts to allergens, such as food or pollen.
- Multiplication of eosinophils. The eosinophils multiply in your esophagus and produce a protein that causes inflammation.
- Damage to the esophagus. Inflammation can lead to scarring, narrowing and formation of excessive fibrous tissue in the lining of your esophagus.
- Dysphagia and impaction. You may have difficulty swallowing (dysphagia) or have food become stuck when you swallow (impaction).
- Additional symptoms. You may have other symptoms, such as chest pain or stomach pain.
There has been a significant increase in numbers of people diagnosed with eosinophilic esophagitis in the past decade. At first, researchers thought this was due to an increase in awareness among doctors and greater availability of tests. However, studies now suggest that the disease is becoming increasingly common, parallel to the increase in asthma and allergies.
RISK FACTORS
The following risk factors are associated with eosinophilic esophagitis:
- Climate. People who live in a cold or dry climate are more likely than those in other climates to be diagnosed with eosinophilic esophagitis.
- Season. You're more likely to be diagnosed between the spring and fall, probably because levels of pollen and other allergens are higher and people are more likely to be outdoors.
- Sex. Eosinophilic esophagitis is more common in males than in females.
- Family history. Doctors think that eosinophilic esophagitis may run in the family (have a genetic component). If your family members have eosinophilic esophagitis, you have a greater chance of being diagnosed.
- Allergies and asthma. If you have food or environmental allergies, asthma, atopic dermatitis, or a chronic respiratory disease, you're more likely to be diagnosed with eosinophilic esophagitis.
- Age. Originally, eosinophilic esophagitis was thought to be a childhood disease, but now it is known to be common in adults as well. The symptoms differ somewhat between children and adults.
SYMPTOMS
Signs and symptoms include:
Adults
- Difficulty swallowing (dysphagia)
- Food getting stuck in the esophagus after swallowing (impaction)
- Chest pain that is often centrally located and does not respond to antacids
- Backflow of undigested food (regurgitation)
Children
- Difficulty feeding, in infants
- Difficulty eating, in children
- Vomiting
- Abdominal pain
- Difficulty swallowing (dysphagia)
- Food getting stuck in the esophagus after swallowing (impaction)
- No response to GERD medication
- Failure to thrive (poor growth, malnutrition and weight loss)
COMPLICATIONS
In some people, eosinophilic esophagitis can lead to the following:
- Scarring and narrowing of the esophagus. This makes it difficult to swallow and more likely that you will have food get stuck.
- Damage to the esophagus. Because of inflammation of the esophagus, endoscopy can cause perforation or tears in the tissue that lines the esophagus. Tearing can also occur in connection with retching that some people experience when they get food stuck in the esophagus.
DIAGNOSIS
Your doctor will consider both your symptoms and test results to diagnose eosinophilic esophagitis. This will include determining whether you have gastroesophageal reflux disease (GERD).
Tests to diagnose eosinophilic esophagitis include:
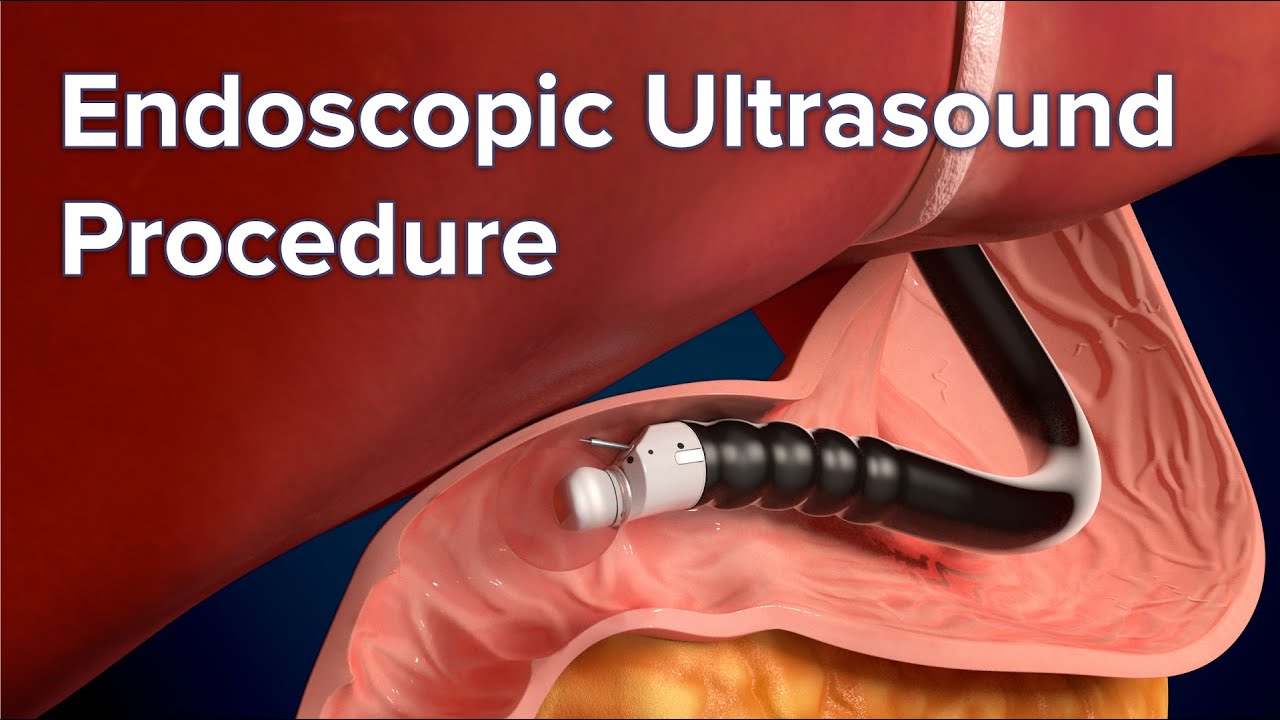
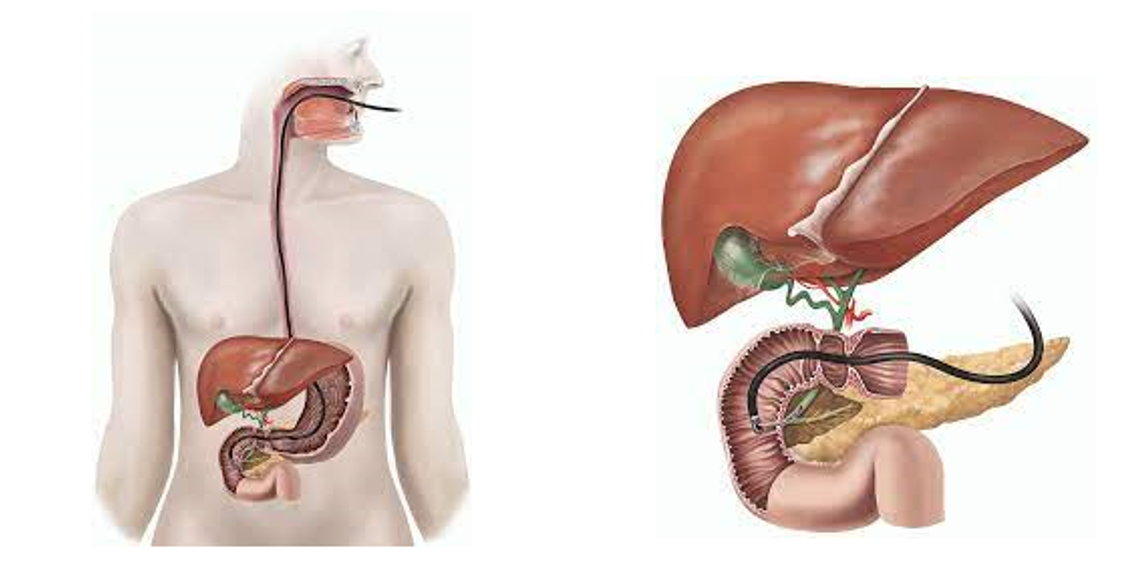
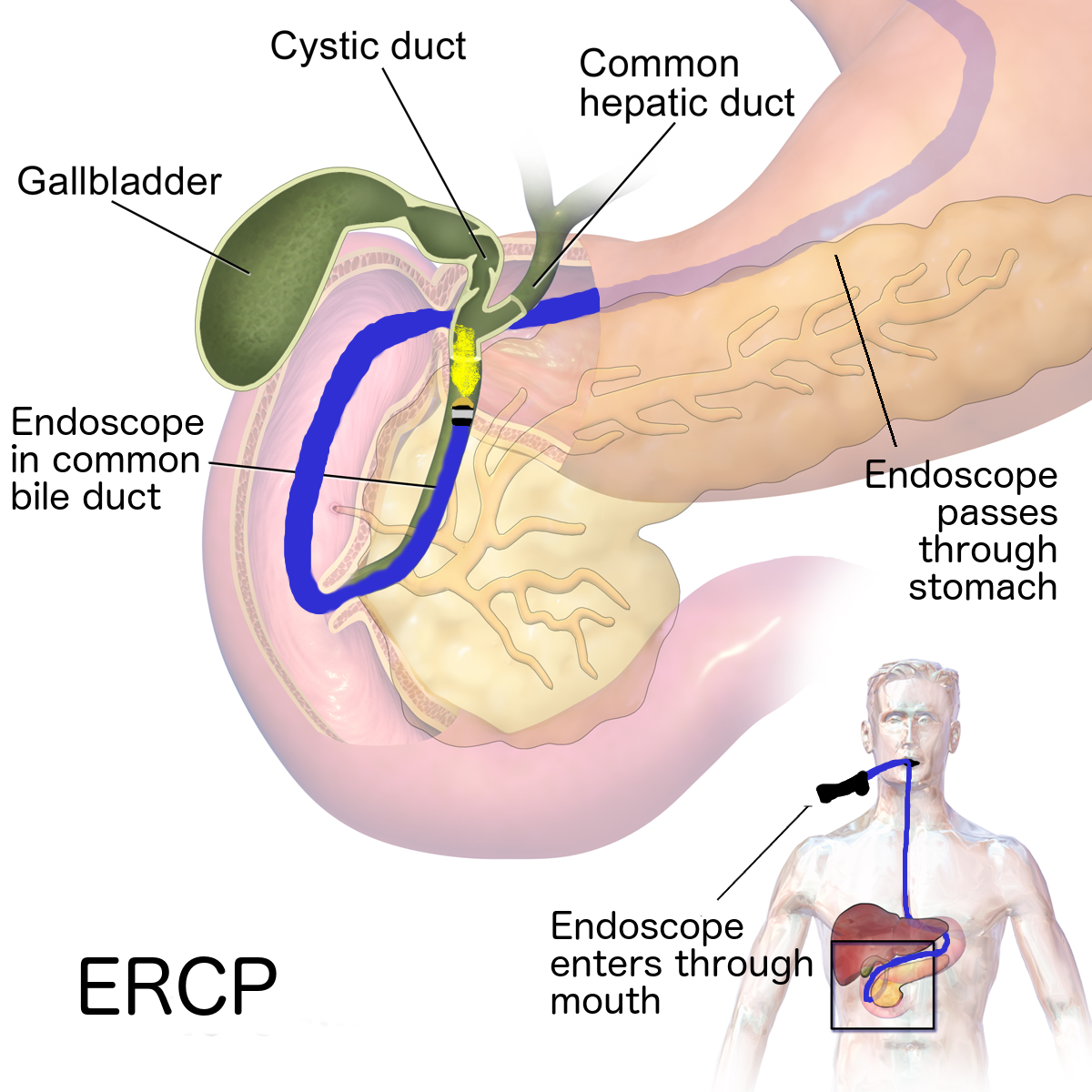
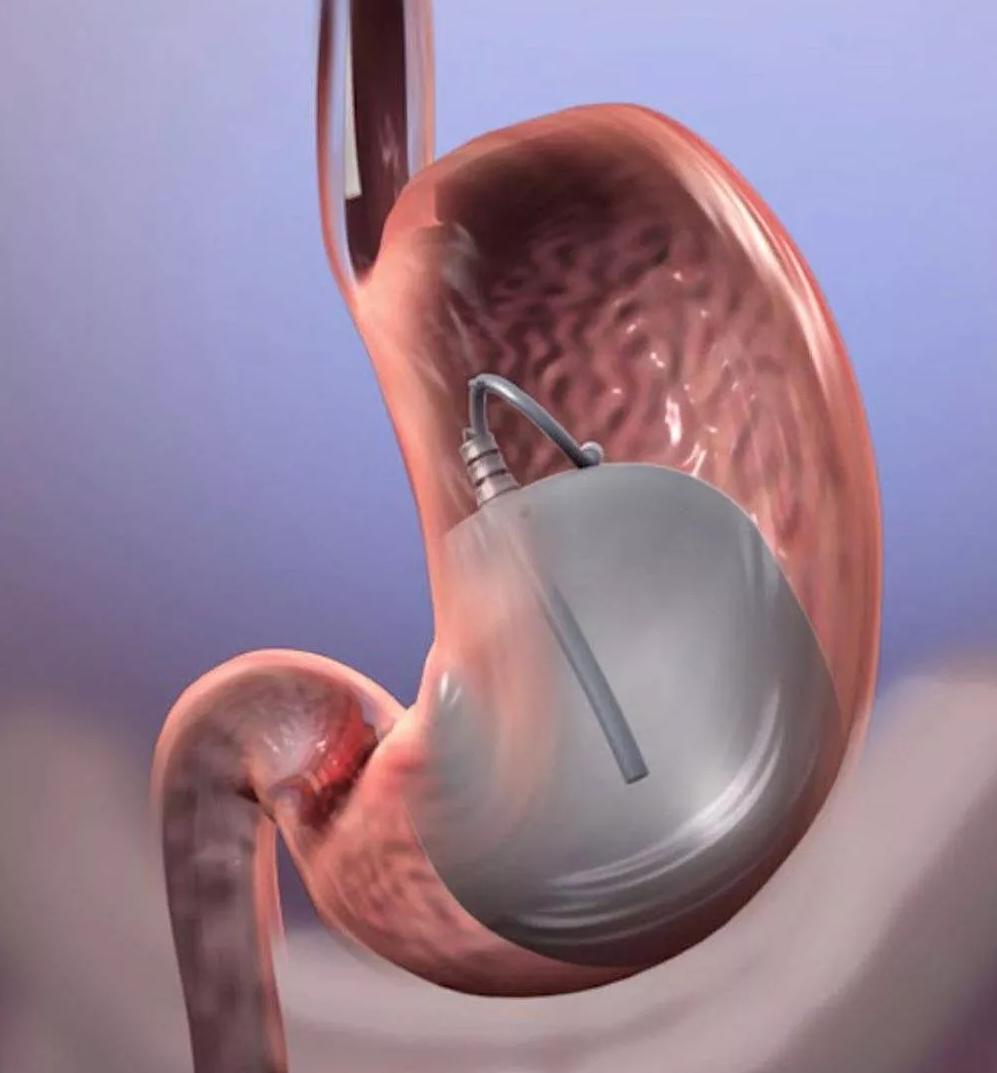
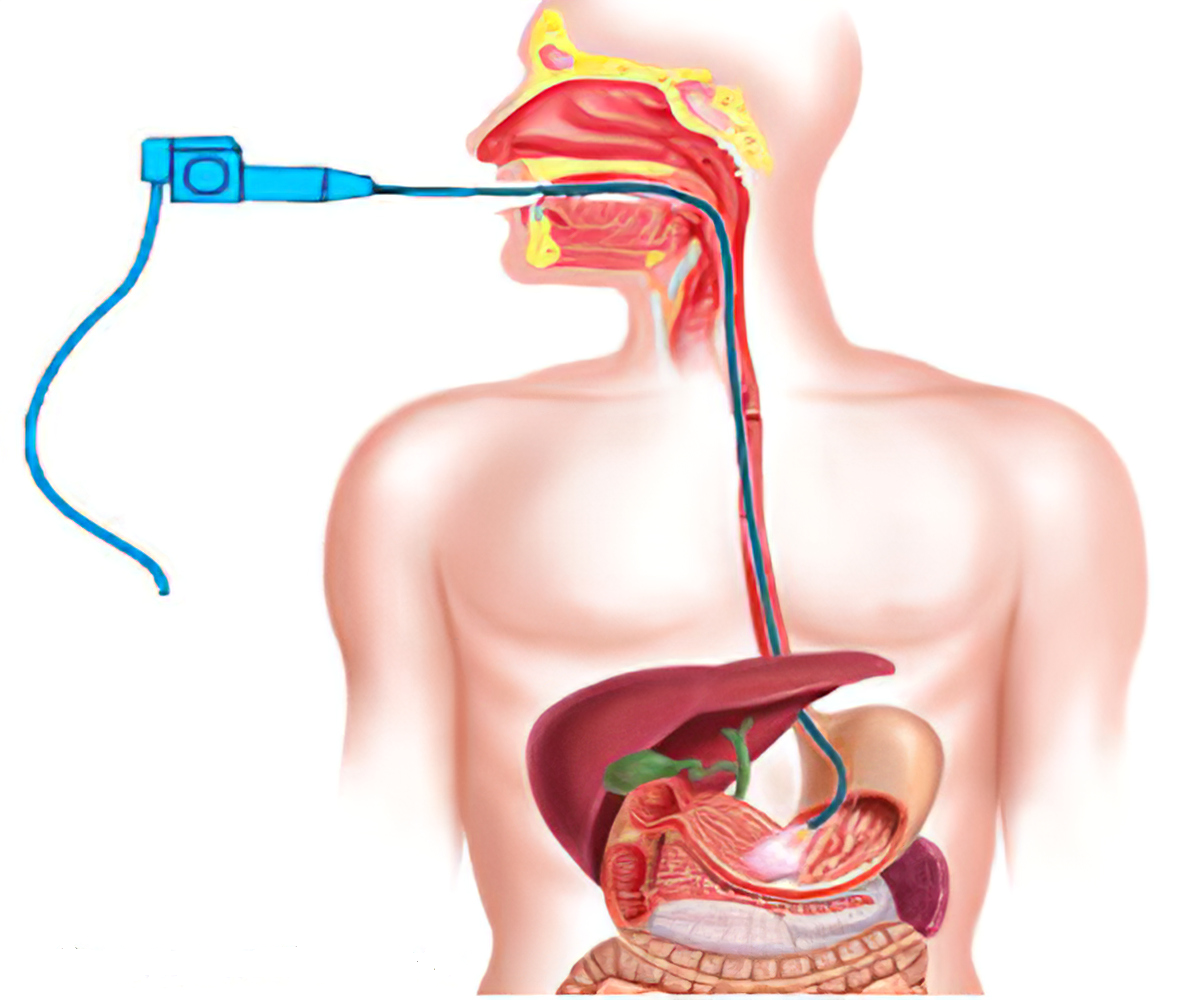
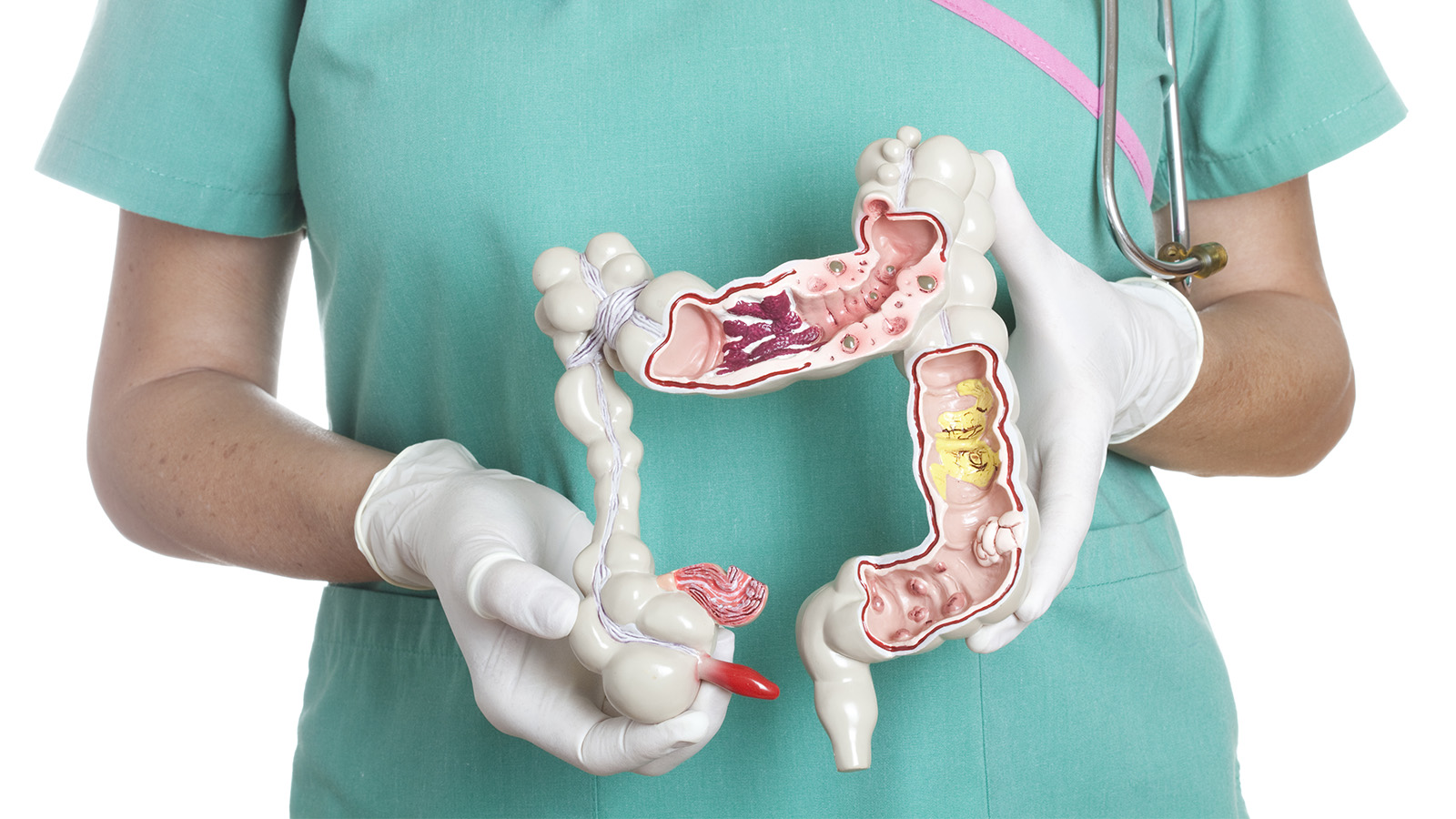
- Upper endoscopy. Your doctor will use a long narrow tube (endoscope) containing a light and tiny camera and insert it through your mouth down the esophagus. The doctor will inspect the lining of your esophagus for inflammation and swelling, horizontal rings, vertical furrows, narrowing (strictures), and white spots. Some people with eosinophilic esophagitis will have an esophagus that looks normal.
- Biopsy. During an endoscopy, your doctor will perform a biopsy of your esophagus. A biopsy involves taking a small bit of tissue. Your doctor will likely take multiple samples from your esophagus and then examine the tissue under a microscope for eosinophils.
- Blood tests. If doctors suspect eosinophilic esophagitis, you may undergo some additional tests to confirm the diagnosis and to begin to look for the sources of your allergic reaction (allergens). You may be given blood tests to look for higher than normal eosinophil counts or total immunoglobulin E levels, suggesting an allergy.
- Esophageal sponge. This test is performed in the doctor's office and involves swallowing a capsule attached to a string. The capsule will dissolve in your stomach and release a sponge that the doctor will pull out your mouth with the string. As the sponge is pulled out, it will sample the esophageal tissues and allow the doctor to determine the degree of inflammation in your esophagus without having to undergo endoscopy.
TREATMENT
Eosinophilic esophagitis is considered a chronic relapsing disease, meaning that most people will require ongoing treatment to control their symptoms. Treatment will involve one or more of the following:
Dietary therapy
Depending on your response to tests for food allergies, your doctor may recommend that you stop eating certain foods, such as dairy or wheat products, to relieve your symptoms and reduce inflammation. A more limited diet is sometimes required.
Medication
-
Proton pump inhibitor (PPI). Your doctor will likely first prescribe an acid blocker such as a PPI. This treatment is the easiest to use, but most people's symptoms don't improve.
-
Topical steroid. If you do not respond to the PPI, your doctor will then likely prescribe a topical steroid, such as fluticasone or budesonide, which is a liquid that is swallowed to treat eosinophilic esophagitis. This type of steroid is not absorbed into the bloodstream, so you are unlikely to have the typical side effects often associated with steroids.
Dilation
If you experience severe narrowing (strictures) of your esophagus, your doctor may recommend dilation (stretching) to help make swallowing easier. Dilation may be used if steroids are not helpful. Or dilation may be a choice to avoid ongoing use of medication.
PREVENTION
There is no particular method to prevent eosinophilic esophagitis. Treatments can help you manage your symptoms and prevent further damage.