Gastroparesis
OVERVIEW | CAUSES | RISK FACTORS | SYMPTOMS | COMPLICATION | DIAGNOSIS | TREATMENT | PREVENTION | REFERENCES
OVERVIEW
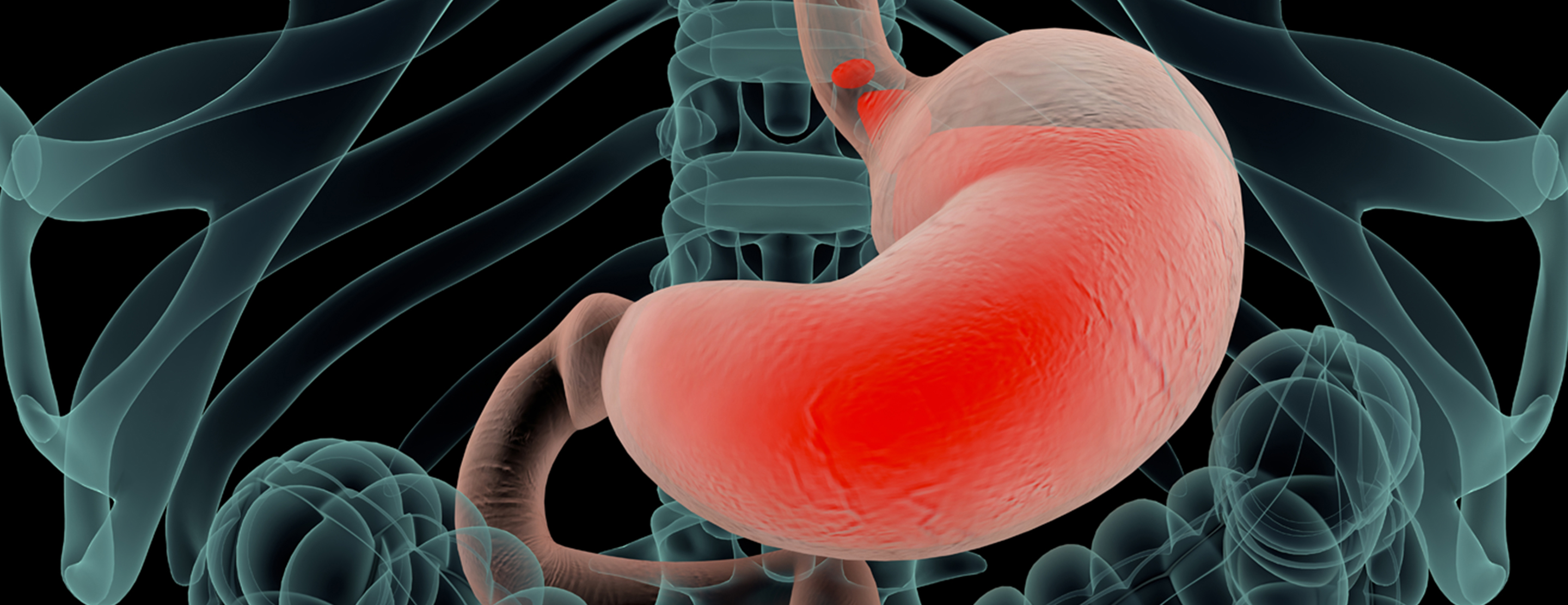
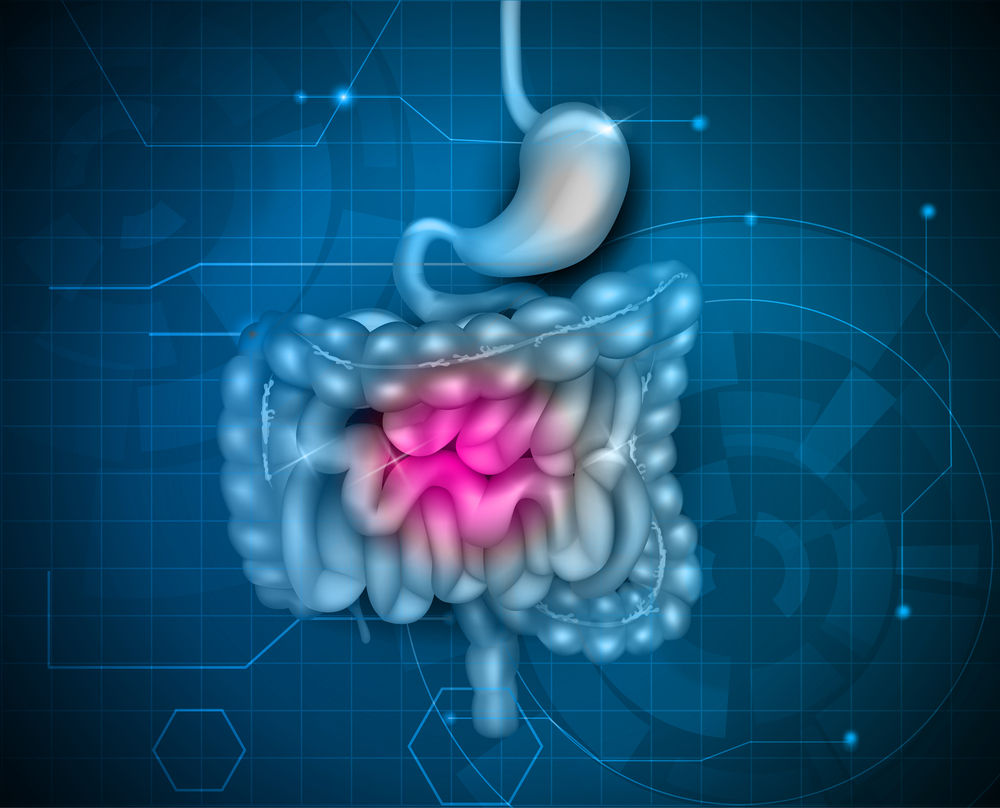
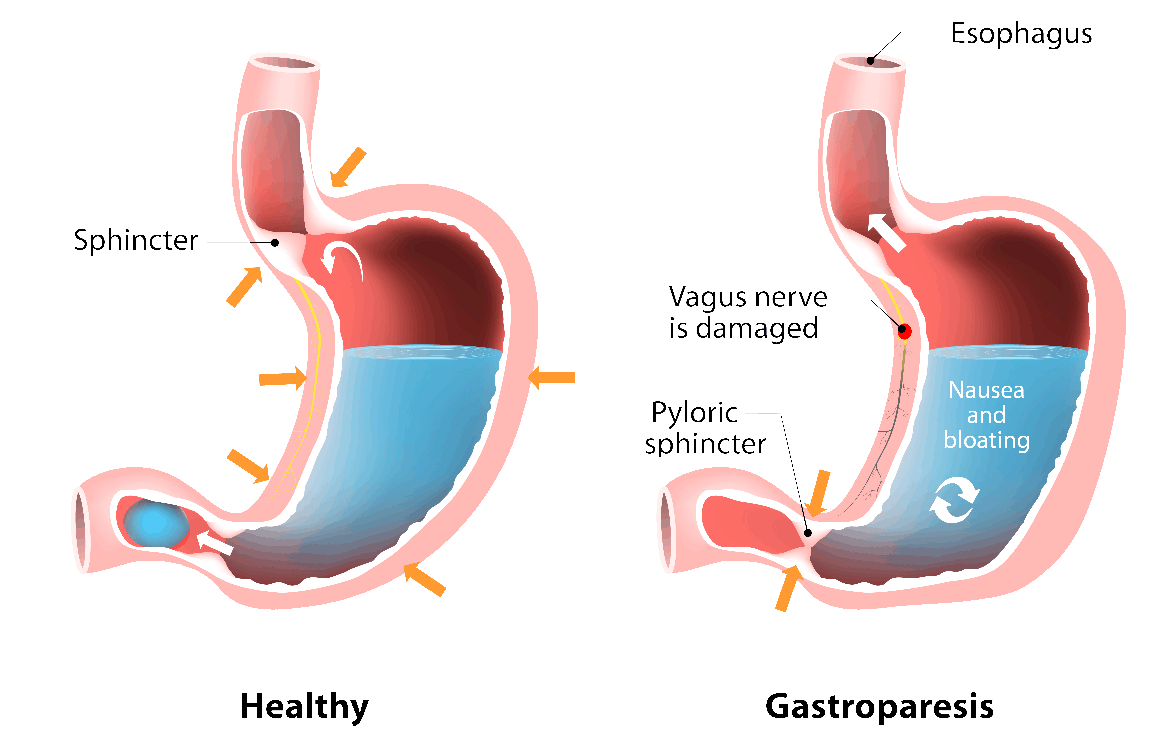
Gastroparesis, which means partial paralysis of the stomach, is a disease in which the stomach cannot empty itself of food in a normal way. If you have this condition, damaged nerves and muscles don’t function with their normal strength and coordination- slowing the movement of contents through your digestive system.
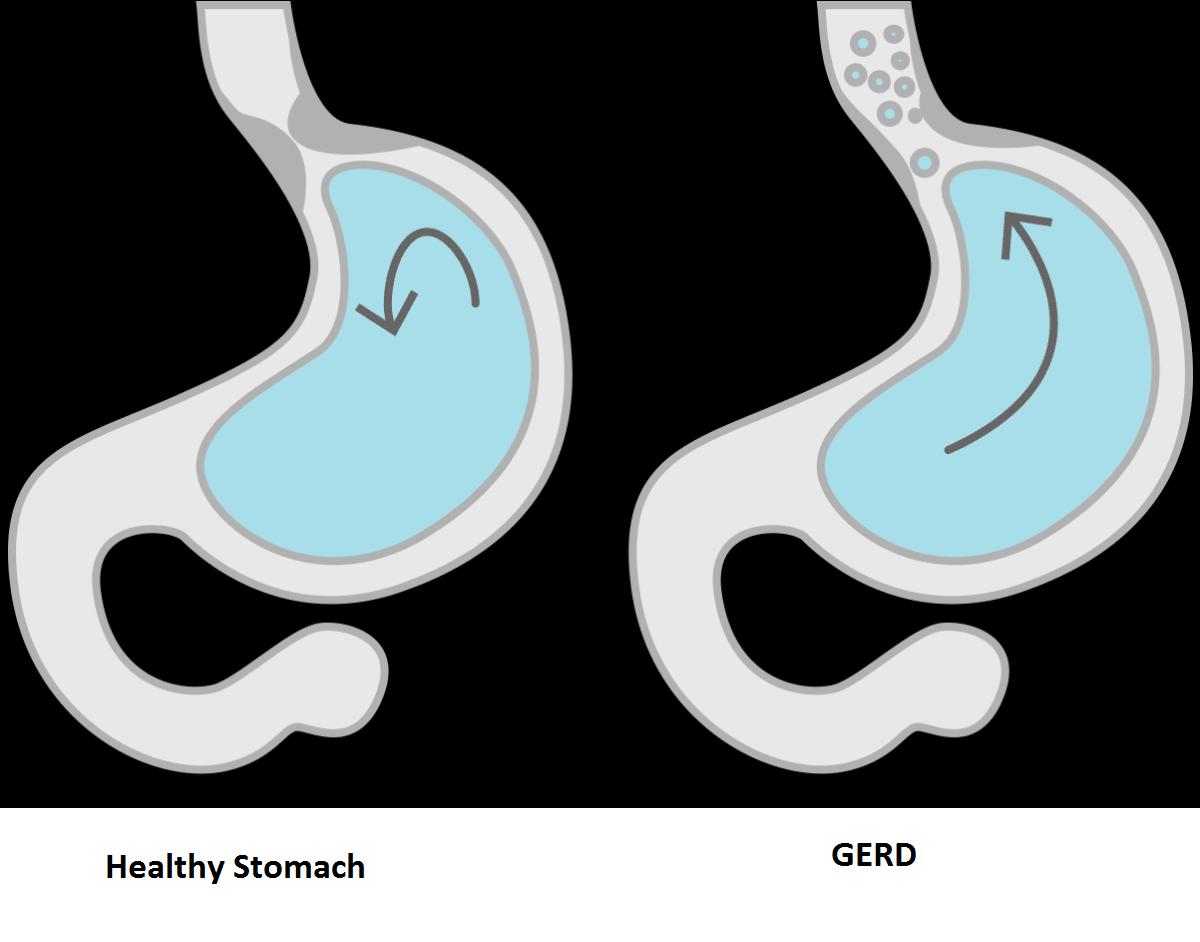
This is a common condition in people who have had diabetes for a long time, but it may also occur in other situations. Gastroparesis can be misdiagnosed and is sometimes mistaken for an ulcer, heartburn or an allergic reaction. In non-diabetic people, the condition may relate to acid reflux.
CAUSES
Gastroparesis is caused by nerve injury, including damage to the vagus nerve. In its normal state, the vagus nerve contracts (tightens) the stomach muscles to help move food through the digestive tract. In cases of gastroparesis, the vagus nerve is damaged by diabetes. This prevents the muscles of the stomach and intestine from working properly, which keeps food from moving from the stomach to the intestines.
Other causes of gastroparesis include:
- Viral infections.
- Gastric (abdominal) surgery with injury to the vagus nerve.
- Medications such as narcotics and some antidepressants.
- Amyloidosis (deposits of protein fibers in tissues and organs) and scleroderma (a connective tissue disorder that affects the skin, blood vessels, skeletal muscles and internal organs).
RISK FACTORS
Factors that can increase your risk of gastroparesis:
- Diabetes
- Abdominal or esophageal surgery
- Infection, usually from a virus
- Certain medications that slow the rate of stomach emptying, such as narcotic pain medications
- Scleroderma — a connective tissue disease
- Nervous system diseases, such as Parkinson's disease or multiple sclerosis
- Underactive thyroid (hypothyroidism)
- Women are more likely to develop gastroparesis than are men.
SYMPTOMS
The symptoms of gastroparesis include:
- Heartburn or gastroesophageal reflux (backup of stomach contents into the esophagus).
- Nausea.
- Vomiting undigested food.
- Early satiety (feeling full quickly when eating).
- Abdominal bloating (enlargement).
- Chronic abdominal pain.
- Poor appetite and weight loss.
- Poor blood sugar control.
COMPLICATIONS
Gastroparesis can cause several problems:
- Food that stays in the stomach too long can ferment, which can lead to the growth of bacteria.
- Food in the stomach can harden into a solid mass called a bezoar. Bezoars can cause blockages in the stomach that keep food from passing into the small intestine.
- People who have both diabetes and gastroparesis may have other problems as well, because blood glucose levels rise quickly when food finally leaves the stomach and enters the small intestine.
- Dehydration (extreme thirst).
- Malnutrition (poor nutrition).
DIAGNOSIS
Your doctor will go over your symptoms and medical history with you. He or she will also give you a physical examination and may order certain blood tests, including blood sugar levels.
Other tests that are used to diagnose gastroparesis include:
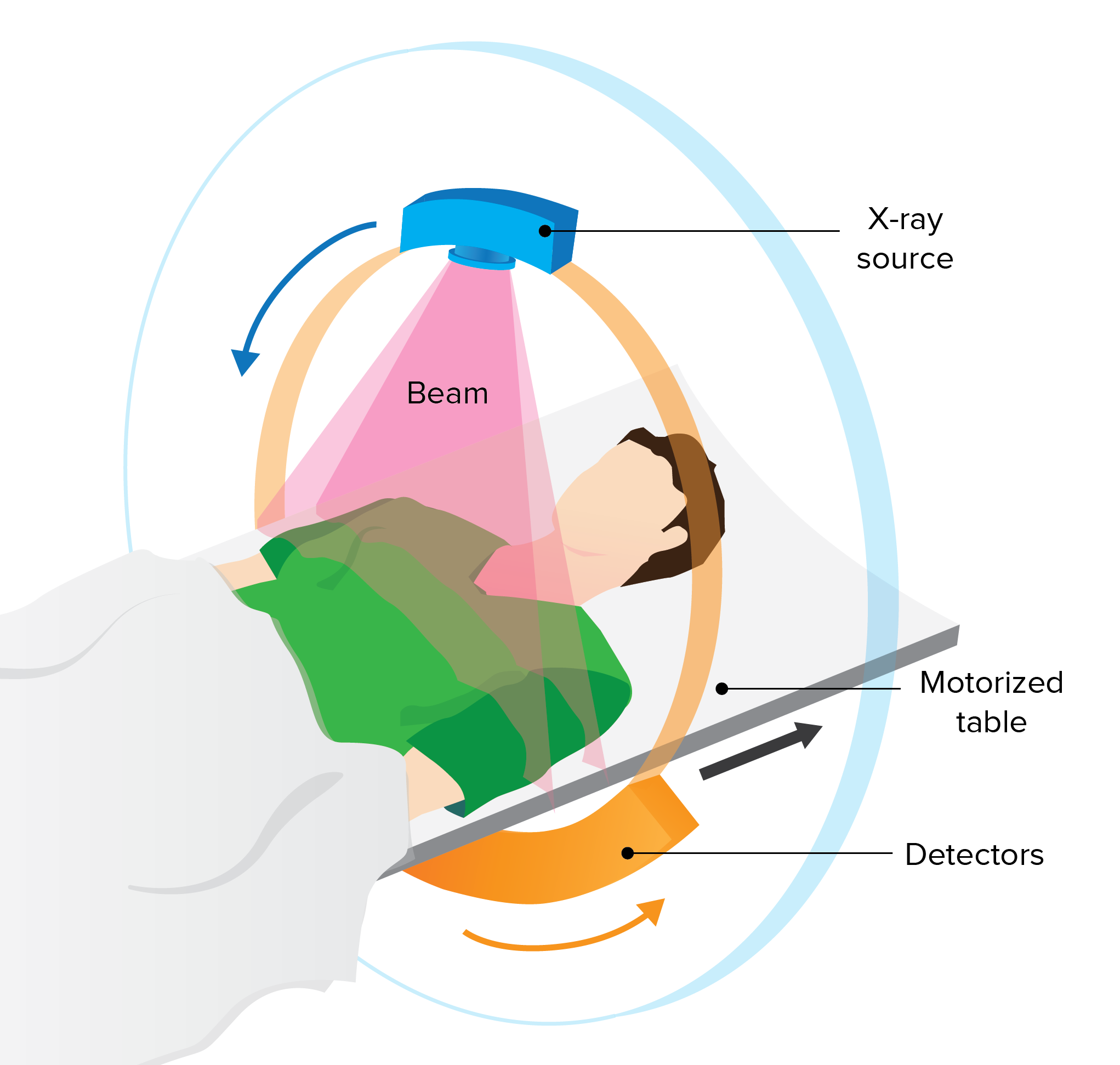
- Four-hour solid gastric emptying study: This is a test to determine the time is takes a meal to move through a your stomach. A technologist will take you to a room and give you a meal to eat that is tagged with a radioactive isotope. After you eat this meal, a one-minute image of your stomach will be taken. You will be allowed to leave the department, but you must return in one, two and four hours.
- SmartPill: This is a capsule that contains a small electronic device. You swallow the capsule, and as it moves through your digestive tract, it sends information to a receiver you are wearing on how quickly food is traveling through the digestive tract.
TREATMENT
Gastroparesis is a chronic (long-lasting) condition. This means that treatment usually doesn’t cure the disease, but you can manage it and keep it under control. People who have diabetes should try to control their blood glucose levels to reduce the problems of gastroparesis.
Some patients may benefit from medications, including:
- Reglan: You take this drug before you eat, and it causes your stomach muscles to contract to help move food out of your stomach. Reglan also helps cut down on vomiting and nausea. Side effects include diarrhea and, rarely, a serious neurological (nerve) disorder.
- Erythromycin: This is an antibiotic that also causes stomach contractions and helps move food out. Side effects include diarrhea and development of resistant bacteria from taking the antibiotic for a long time.
- Antiemetics: These are drugs that help control nausea.
Surgery for gastroparesis
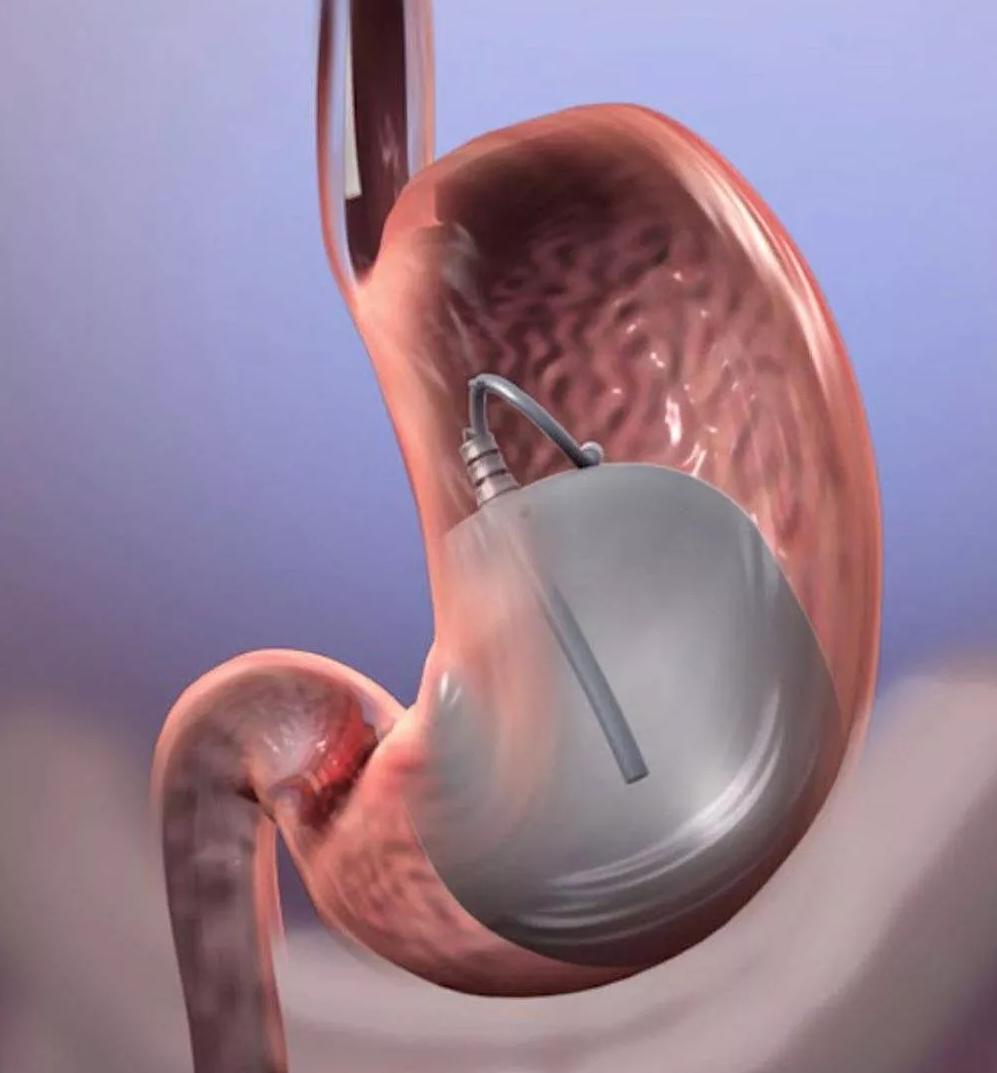
Gastroparesis patients who still have nausea and vomiting even after taking medications may benefit from surgery. One type of surgery for gastroparesis is gastric electrical stimulation, which is a treatment that sends mild electric shocks to the stomach muscles. In this procedure, the doctor inserts a small device called a gastric stimulator into the abdomen. The stimulator has two leads that are attached to the stomach and provide the mild electric shocks, which help control vomiting. The strength of the electric shocks can be adjusted by the doctor. The device runs on a battery that lasts up to 10 years.
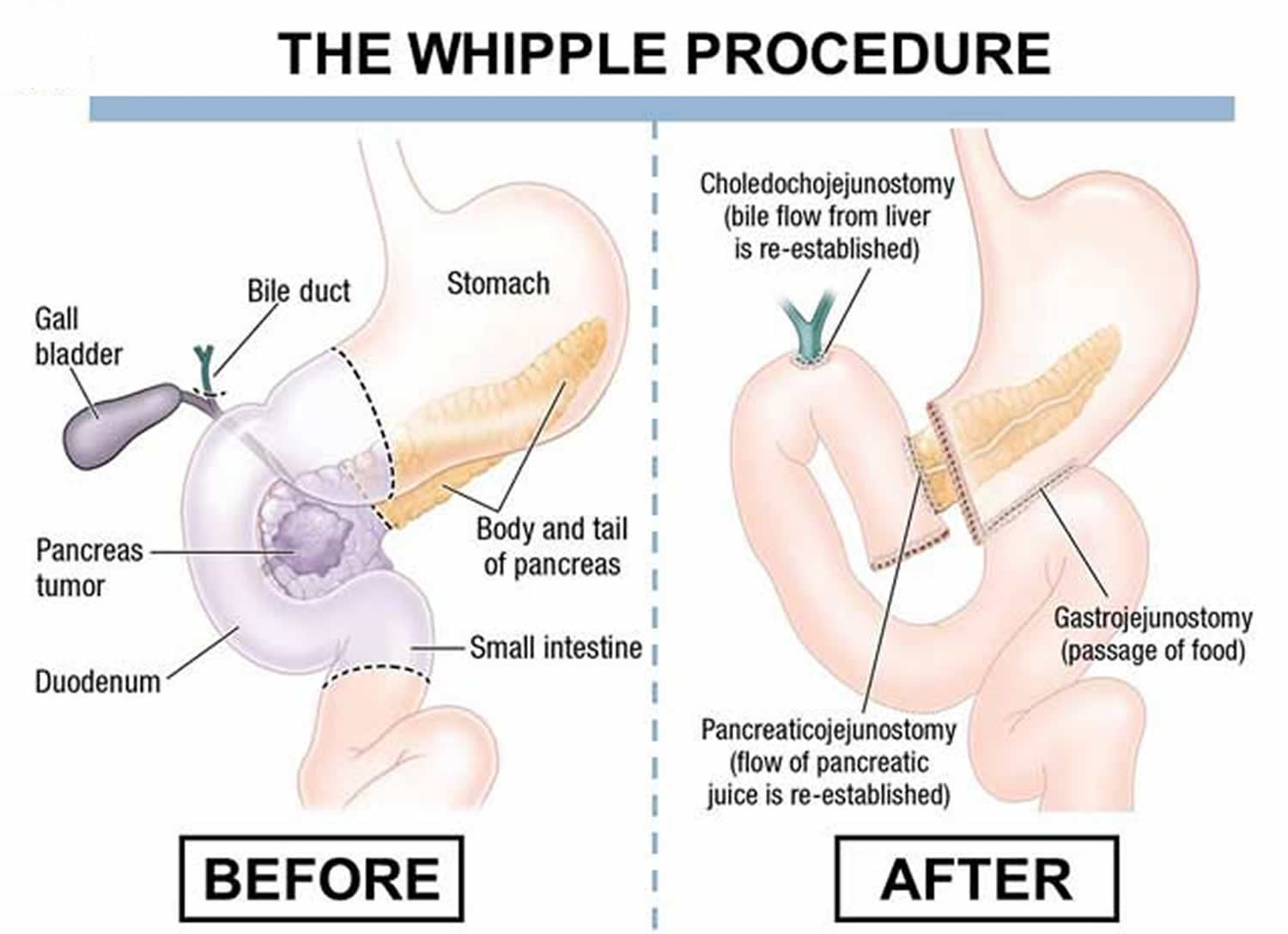
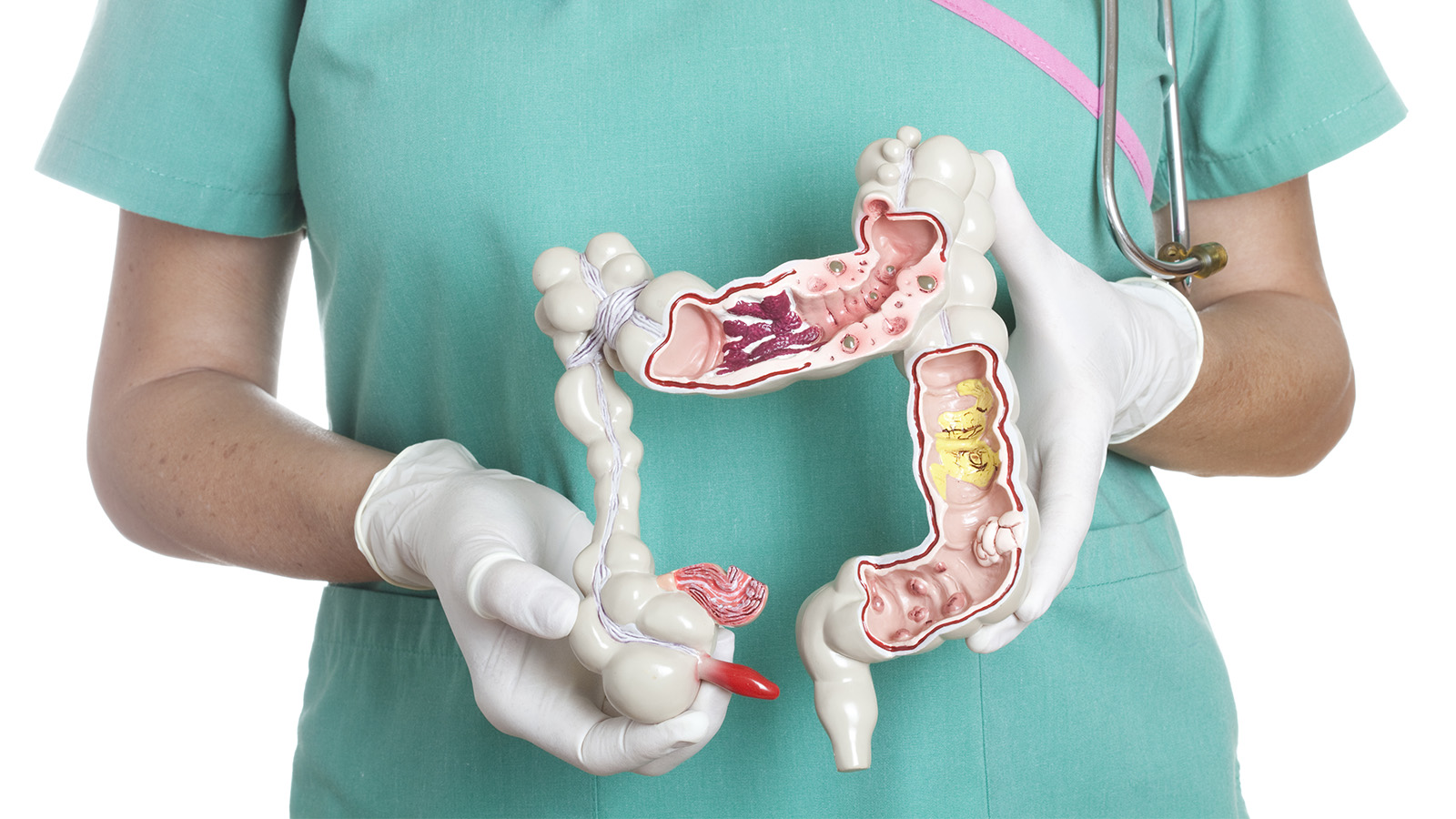
Another surgery to relieve gastroparesis symptoms is gastric bypass, in which a small pouch is created from the top part of the stomach. The small intestine is divided in half and the lower end is attached directly to the small stomach pouch. This limits the amount of food the patient can eat. This surgery is more effective for an obese diabetic patient than either medication or a gastric stimulator.
Are there any other treatments for gastroparesis?
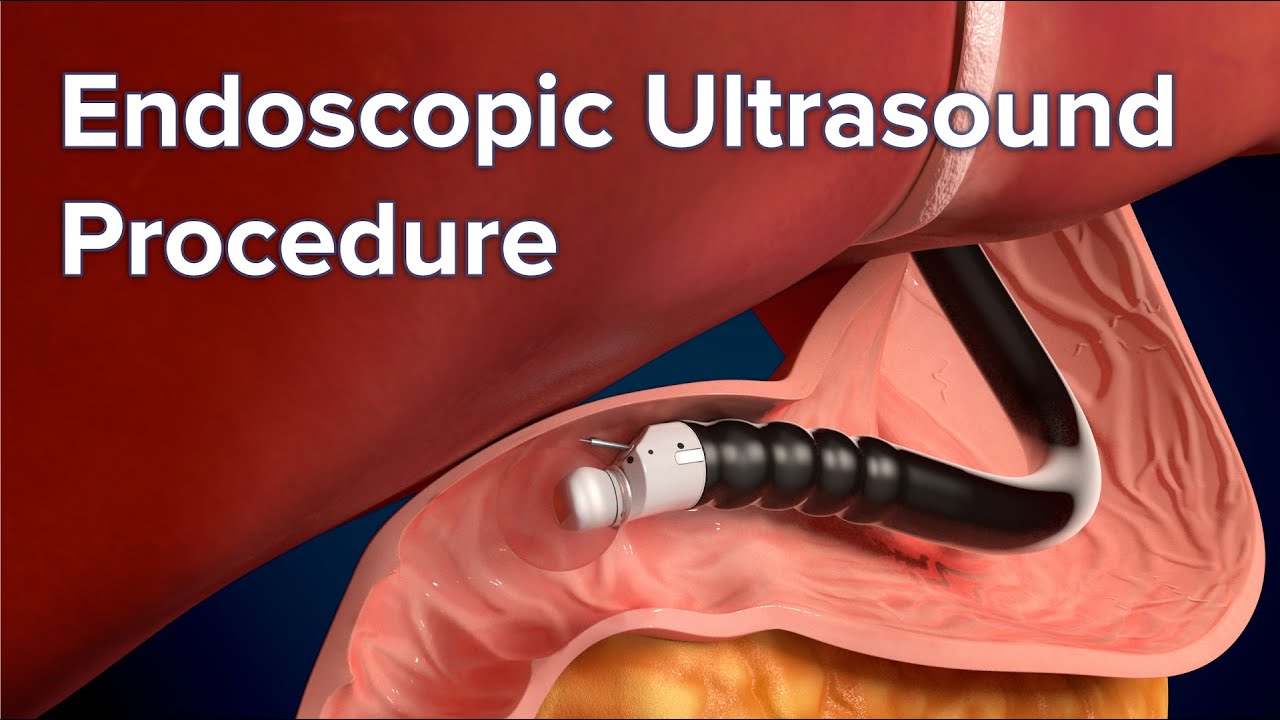
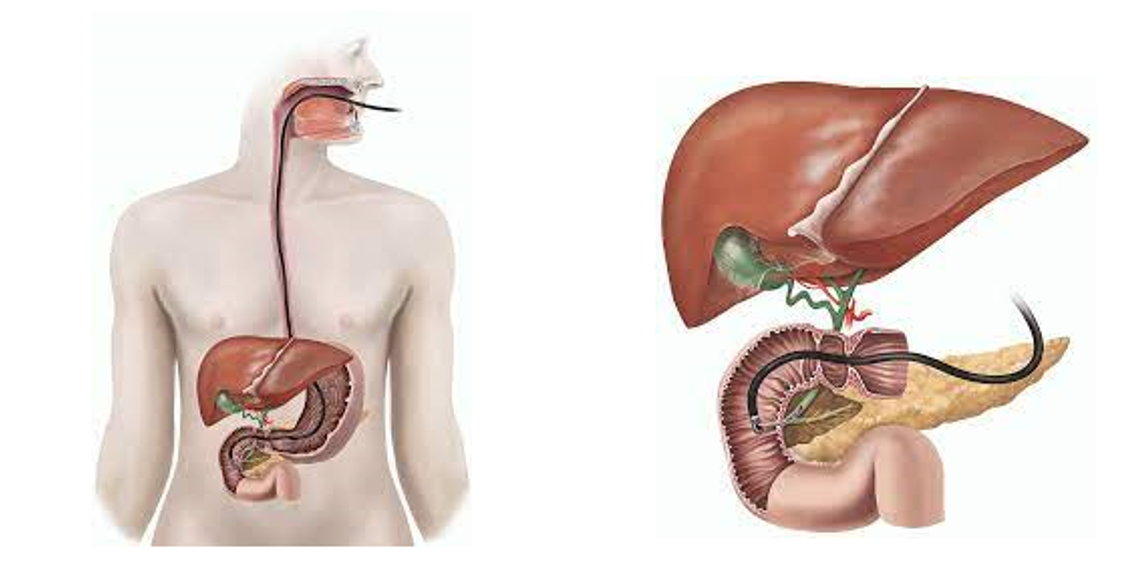
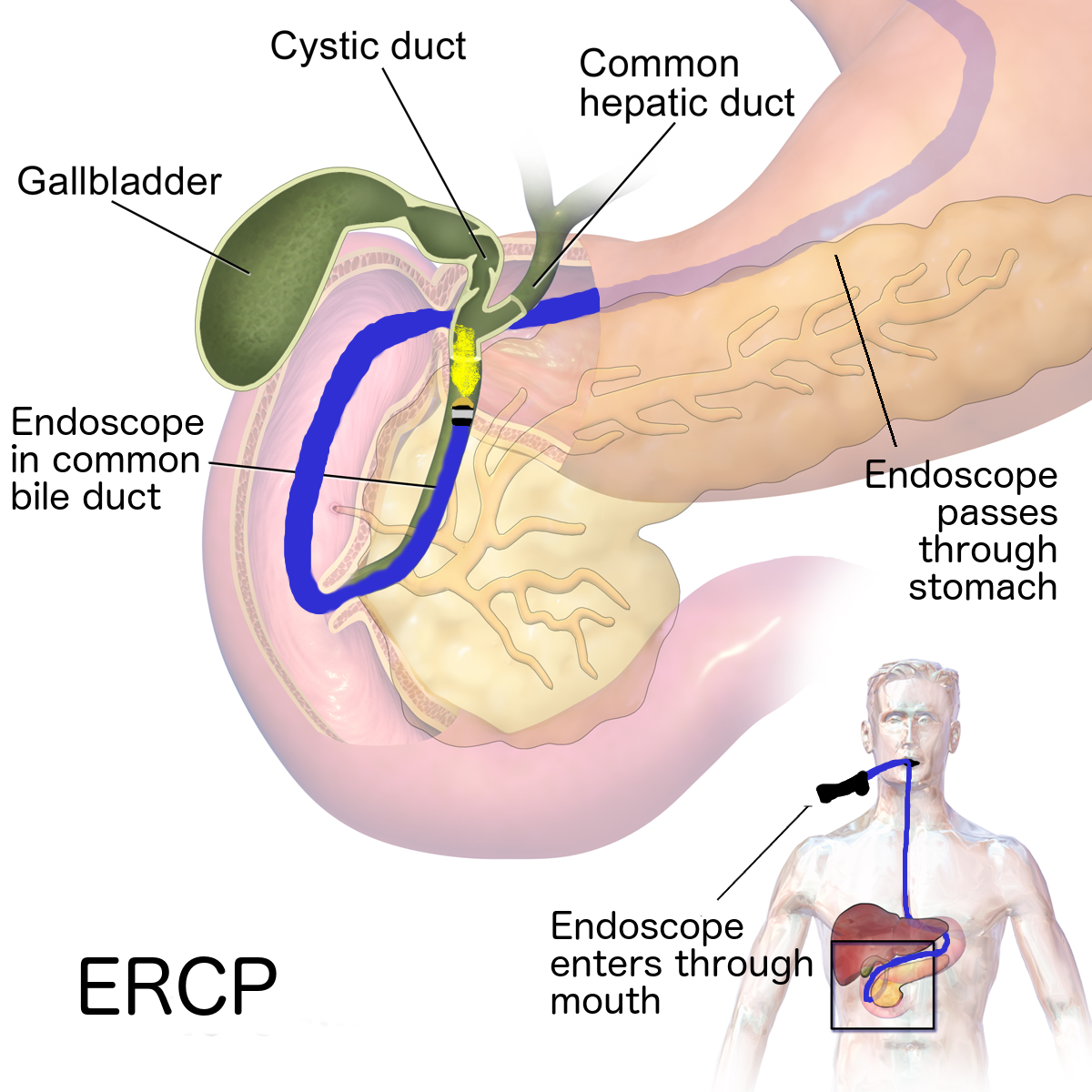
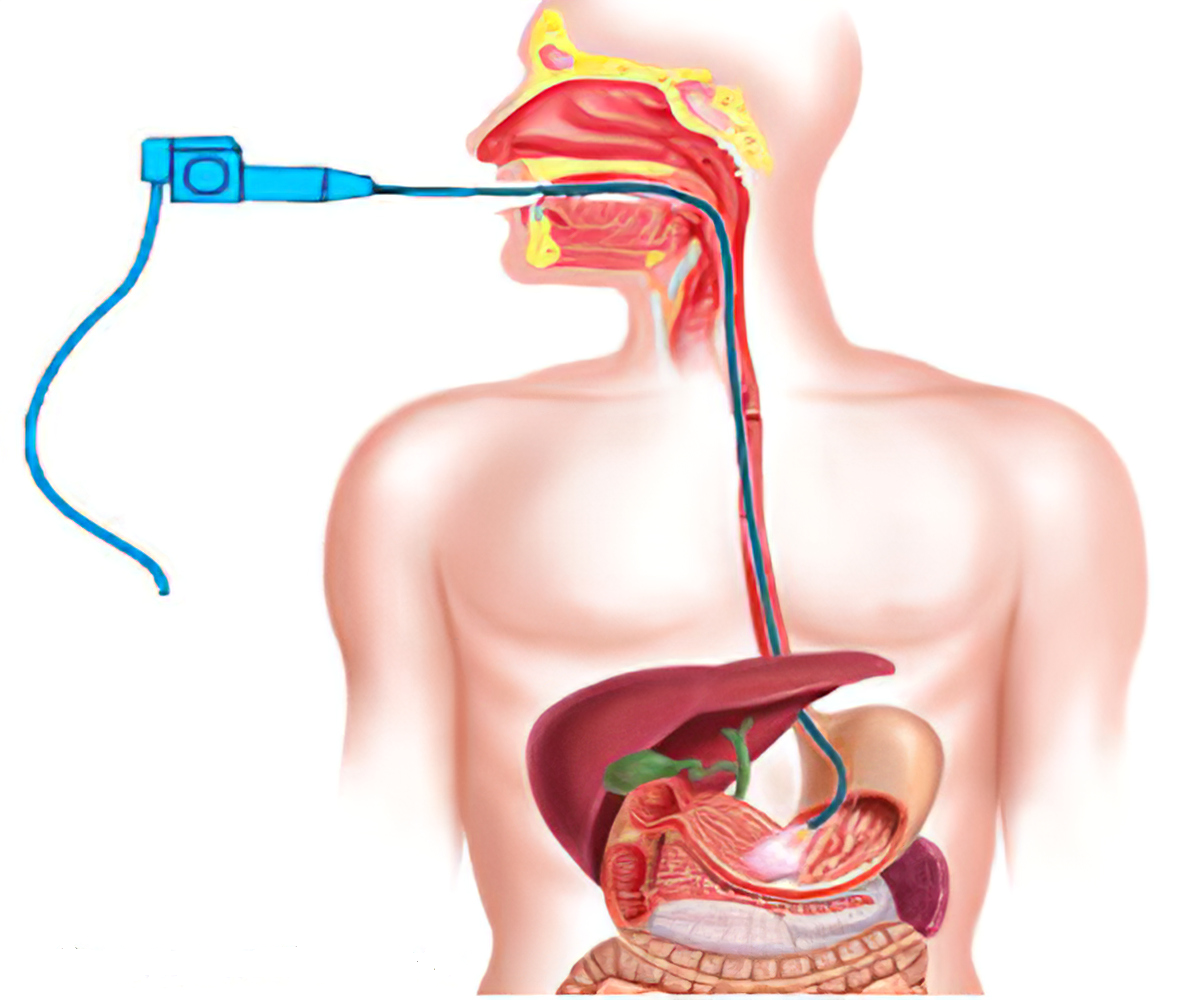
A newer treatment for gastroparesis is called per oral pyloromyotomy (POP). This is a nonsurgical procedure in which the doctor inserts an endoscope (a long, thin, flexible instrument) into the patient’s mouth and advances it to the stomach. The doctor then cuts the pylorus, the valve that empties the stomach, which allows food to move from the stomach to the small intestine more easily.
In a severe case of gastroparesis, your doctor may decide you would benefit from a feeding tube, or jejunostomy tube. The tube is inserted in a surgical procedure through your abdomen into your small intestine. To feed yourself, you put nutrients into the tube, which go directly into your small intestine; this way, they go around the stomach and get into your bloodstream more quickly. The jejunostomy tube is usually a temporary measure.
Another treatment option is intravenous, or parenteral, nutrition. This is a feeding method in which nutrients go directly into your bloodstream through a catheter placed into a vein in your chest. Like a jejunostomy tube, parenteral nutrition is meant to be a temporary measure for a severe case of gastroparesis.
Should I change my diet if I have gastroparesis?
One of the best ways to help control the symptoms of gastroparesis is to change your daily eating habits. For instance, instead of three meals a day, you can eat six small meals. In this way, there is less food in your stomach — you won’t feel as full, and it will be easier for the food to leave your stomach.
Another important factor is the texture of food; liquids and low residue are encouraged (for example, you should eat applesauce instead of whole apples with intact skins).
You should also avoid foods that are high in fat (which can slow down digestion) and fiber (which is difficult to digest).
- Work with a registered dietician (RD) or nutrition support specialist (nurse or doctor) to design a dietary plan to meet your individual needs; understand how to use and maintain dietary and nutritional therapies.
- Eat frequent, small meals that are low in fat and fiber. Fat, fiber, and large meals can delay stomach emptying and worsen symptoms.
- Keep hydrated and as nutritionally fit as possible.
- If you have diabetes, maintain good glucose control. Irregular stomach emptying can negatively affect blood sugar levels. Keeping your blood sugar under control may help stomach emptying.
- Before having surgery, ask your doctor, surgeon, or health care team about risks involved and weigh these against the benefits. Ask about alternatives.
- Let your doctor and pharmacist know about all medications you are taking – prescription and over-the-counter, as well as any supplements.
- Be aware of possible drug interactions and discuss alternatives with your doctor.
- Understand the possible side effects of your treatments, and know what to do if side effects occur.
- Avoid or reduce alcohol and smoking tobacco. These can slow gastric emptying.
- Engage in regular physical activity as you are able.
Seek appropriate care and take an active role in your health. Working along with your doctor or health care team will help control, reduce, or prevent symptoms and complications.