Disease
Inflammatory Bowel Disease (IBD)
OVERVIEW | CAUSES | RISK FACTORS | SYMPTOMS | COMPLICATION | Diagnosis | TREATMENT | PREVENTION | REFERENCES
Overview
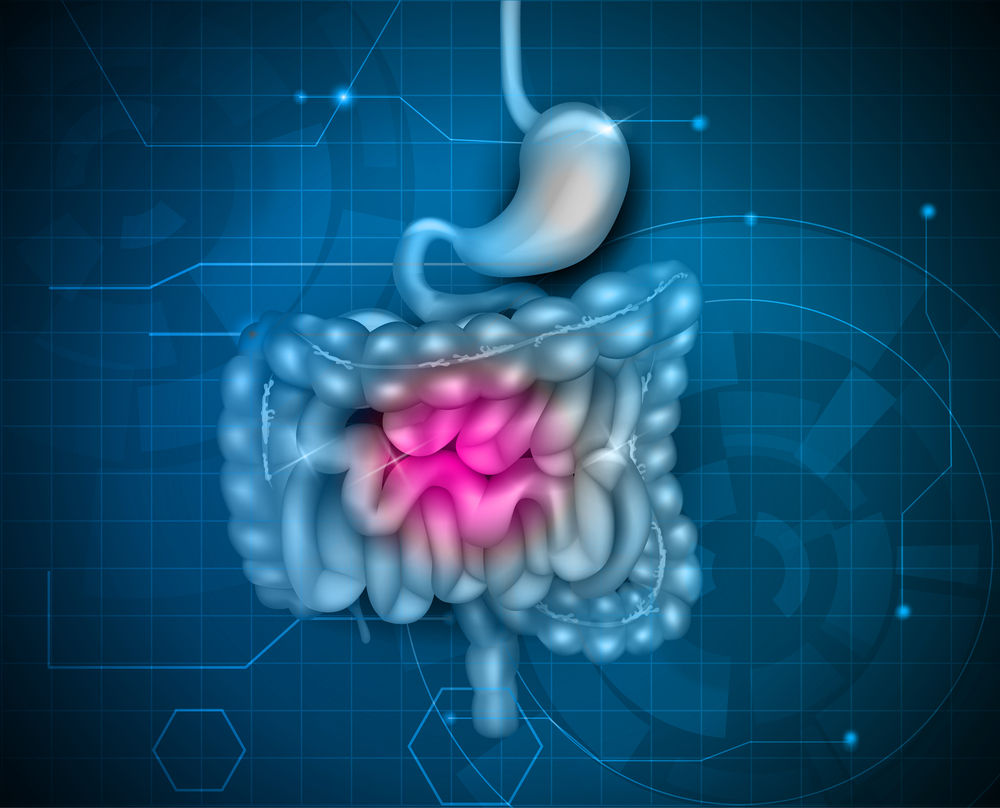
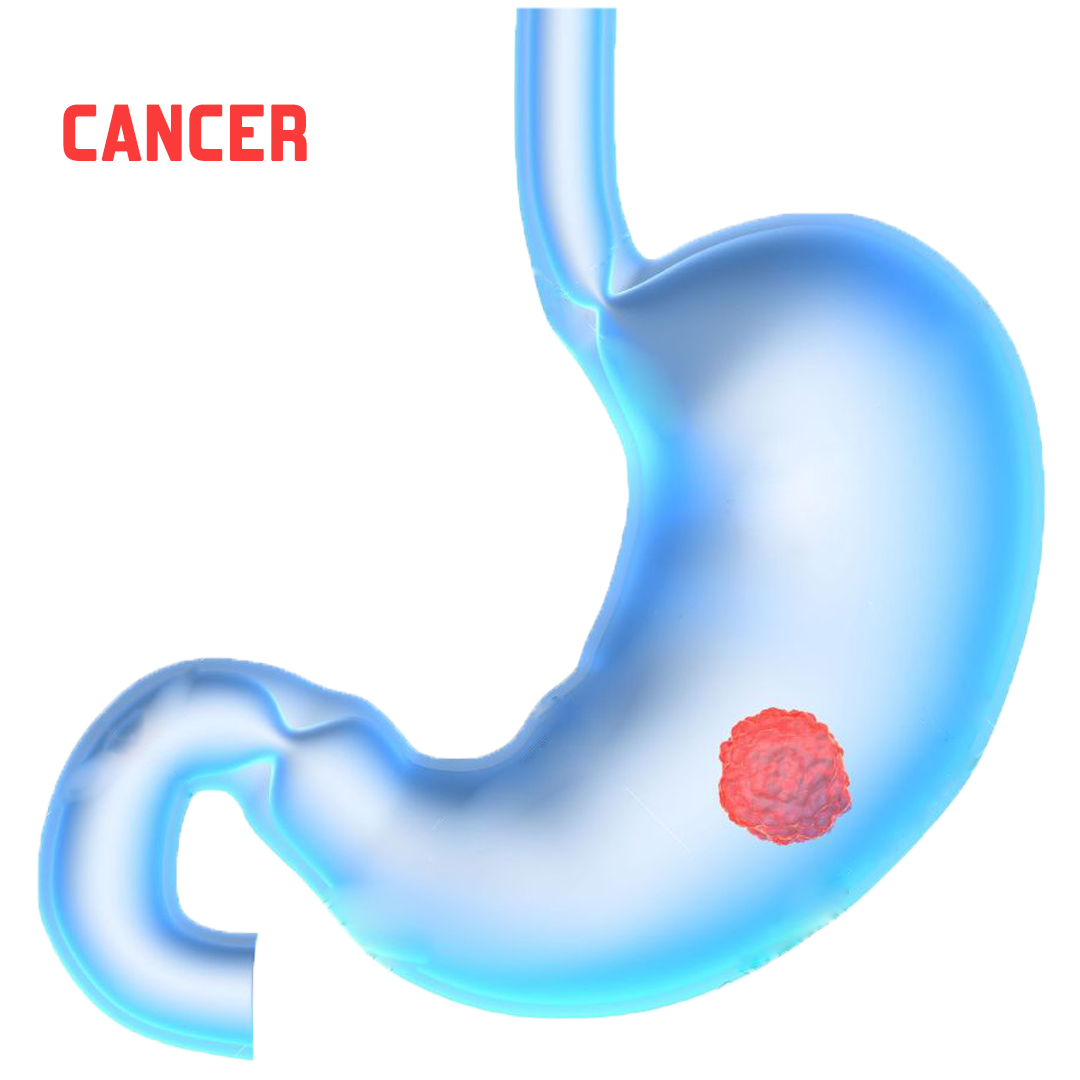
Inflammatory bowel disease (IBD) represents a group of intestinal disorders that cause prolonged inflammation of the digestive tract.
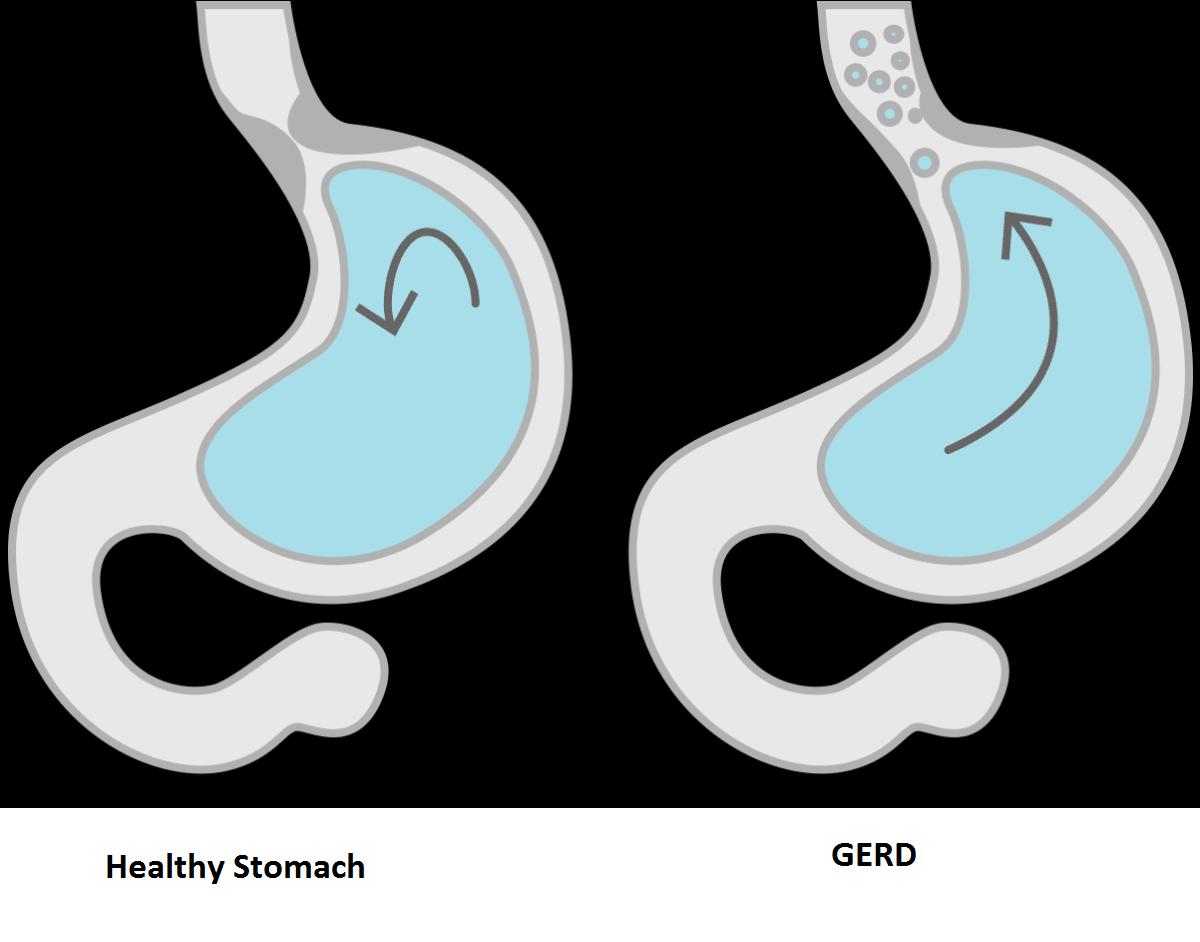
The digestive tract comprises the mouth, esophagus, stomach, small intestine, and large intestine. It’s responsible for breaking down food, extracting the nutrients, and removing any unusable material and waste products.
Inflammation anywhere along the digestive tract disrupts this normal process. IBD can be very painful and disruptive, and in some cases, it may even be life-threatening.
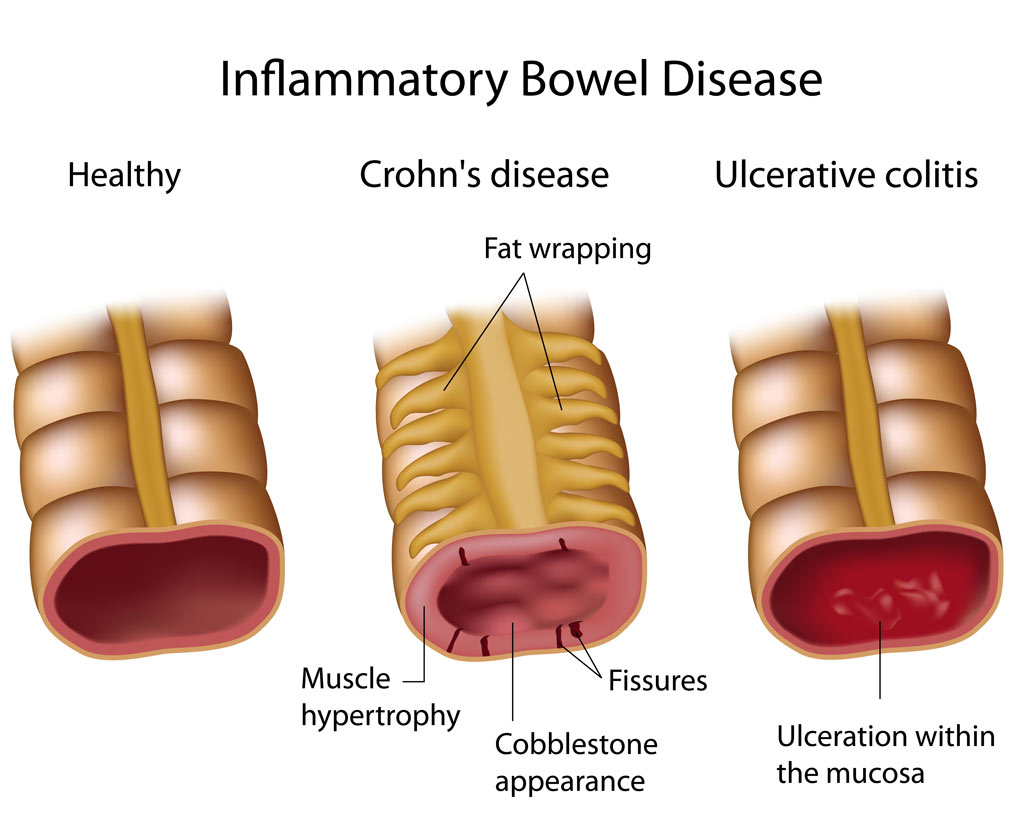
Many diseases are included in this IBD umbrella term. The two most common diseases are ulcerative colitis and Crohn’s disease.
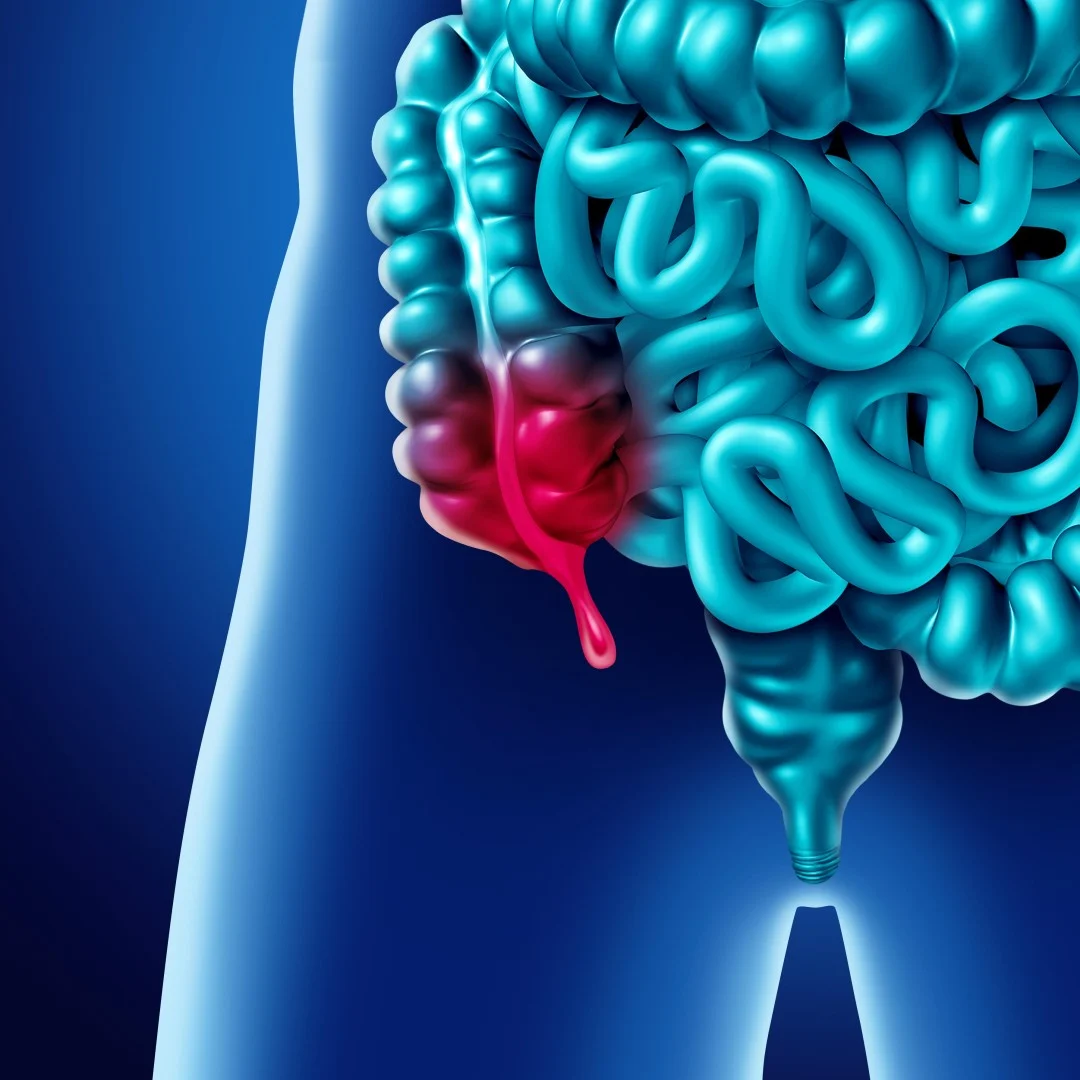
Crohn’s disease can cause inflammation in any part of the digestive tract. However, it mostly affects the tail end of the small intestine.
Ulcerative colitis involves inflammation of the large intestine.
Causes
The exact cause of IBD is unknown. However, genetics and problems with the immune system have been associated with IBD.
1. Genetics
You might be more likely to develop IBD if you have a sibling or parent with the disease. This is why scientists believe IBD may have a genetic component.
2. The immune system
The immune system may also play a role in IBD.
Normally, the immune system defends the body from pathogens (organisms that cause diseases and infections). A bacterial or viral infection of the digestive tract can trigger an immune response.
As the body tries to fight off the invaders, the digestive tract becomes inflamed. When the infection is gone, the inflammation goes away. That’s a healthy response.
In people with IBD, however, digestive tract inflammation can happen even when there’s no infection. The immune system attacks the body’s own cells instead. This is known as an autoimmune response.
IBD can also occur when the inflammation doesn’t go away after the infection is cured. The inflammation may continue for months or even years.
Risk factors
The biggest risk factors for developing Crohn’s disease and ulcerative colitis include:
1. Smoking
Smoking is one of the main risk factors for developing Crohn’s disease.
Smoking also aggravates the pain and other symptoms of Crohn’s disease and increases the risk of complications. However, ulcerative colitis primarily affects nonsmokers and ex-smokers.
2. Ethnicity
IBD is present in all populations. However, certain ethnic groups such as Caucasians and Ashkenazi Jews have a higher risk.
3. Age
IBD can happen at any age, but in most cases, it starts before the age of 35.
4. Family history
People who have a parent, sibling, or child with IBD are at a much higher risk for developing it themselves.
5. Geographical region
People who live in urban areas and industrialized countries have a higher risk of getting IBD.
Those with white collar jobs are also more likely to develop the disease. This can be partially explained by lifestyle choices and diet.
People who live in industrialized countries tend to eat more fat and processed food. IBD is also more common among people living in northern climates, where it’s often cold.
6. Gender
In general, IBD affects both genders equally. Ulcerative colitis is more common among men, while Crohn’s disease is more common among women.
Symptoms
Symptoms of IBD vary depending on the location and severity of inflammation, but they may include:
- diarrhea, which occurs when affected parts of the bowel can’t reabsorb water
- bleeding ulcers, which may cause blood to show up in the stool (hematochezia)
- stomach pain, cramping, and bloating due to bowel obstruction
- weight loss and anemia, which can cause delayed growth or development in children
People with Crohn’s disease may also get canker sores in their mouths. Sometimes ulcers and fissures also appear around the genital area or anus.
IBD can also be associated with problems outside of the digestive system, such as:
- eye inflammation
- skin disorders
- arthritis
Complications
Possible complications of IBD include:
- malnutrition with resulting weight loss
- colon cancer
- fistulas, or ulcers that go through the bowel wall, creating a hole between different parts of the digestive tract
- intestinal rupture, or perforation
- bowel obstruction
In rare cases, a severe bout of IBD can make you go into shock. This can be life-threatening. Shock is usually caused by blood loss during a long, sudden episode of bloody diarrhea.
Diagnosis
To diagnose IBD, your doctor will first ask you questions about your family’s medical history and your bowel movements.
A physical exam may then be followed by one or more diagnostic tests.
1. Stool sample and blood test
These tests can be used to look for infections and other diseases.
Blood tests can also sometimes be used to distinguish between Crohn’s disease and ulcerative colitis. However, blood tests alone can’t be used to diagnose IBD.
2. Barium enema
A barium enema is an X-ray exam of the colon and small intestine. In the past, this type of test was often used, but now other tests have largely replaced it.
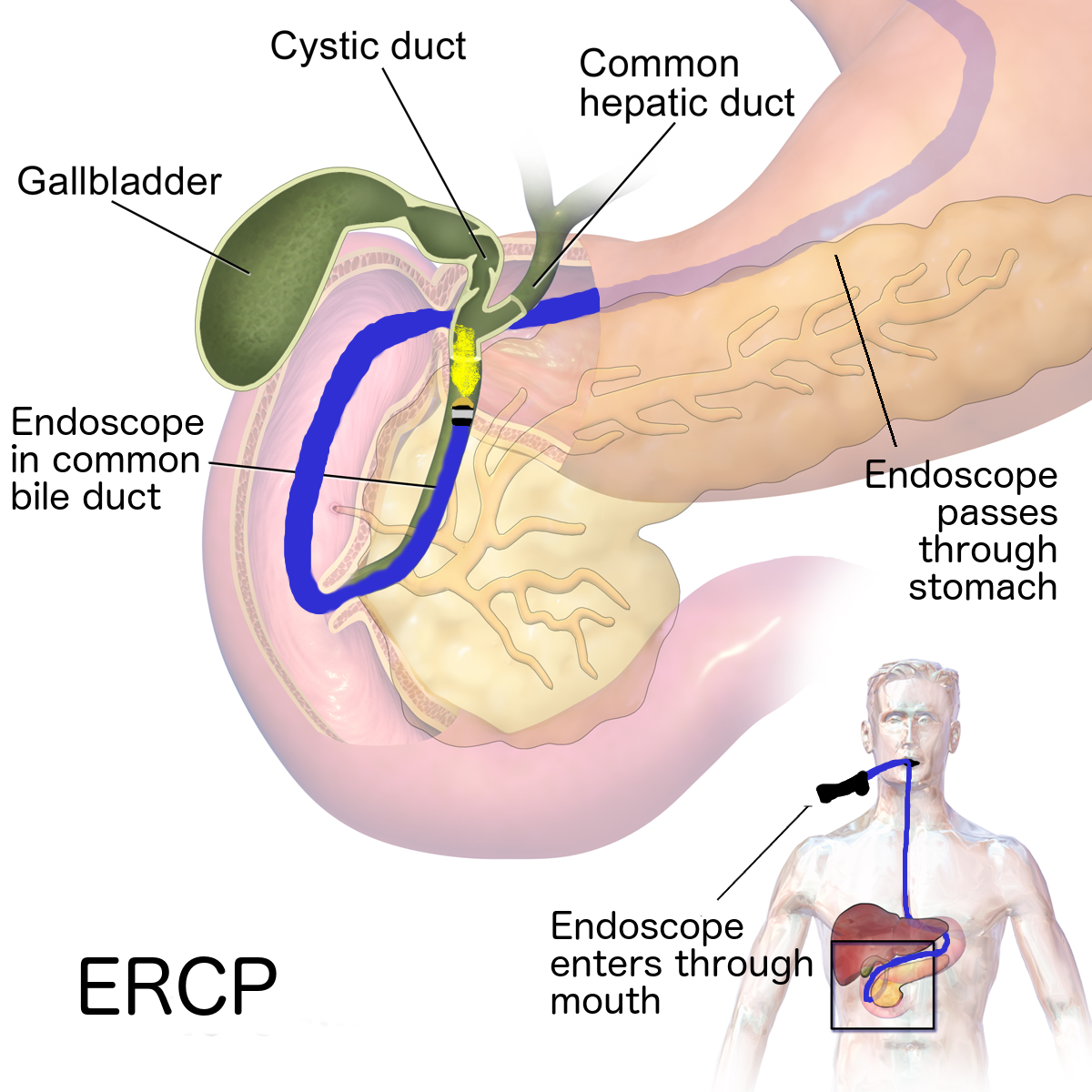
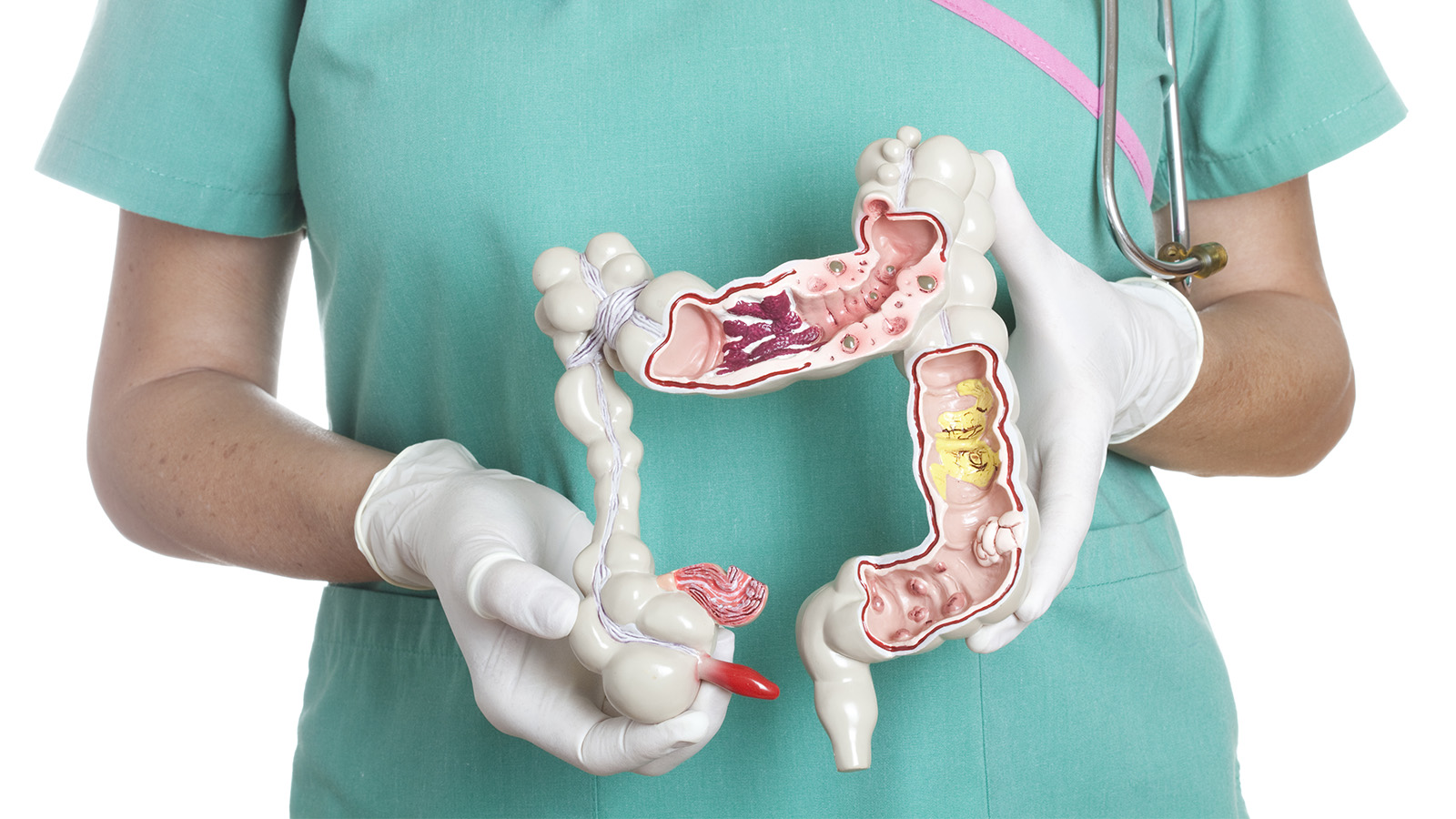
3. Flexible sigmoidoscopy and colonoscopy
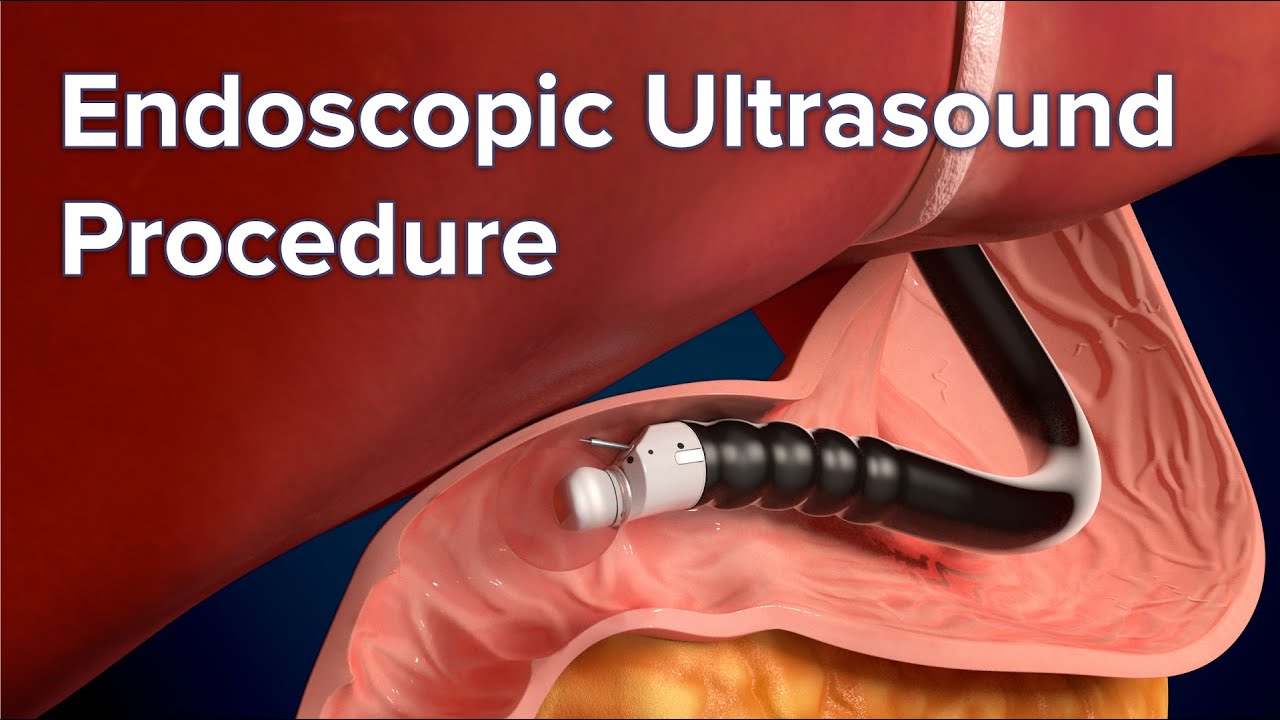
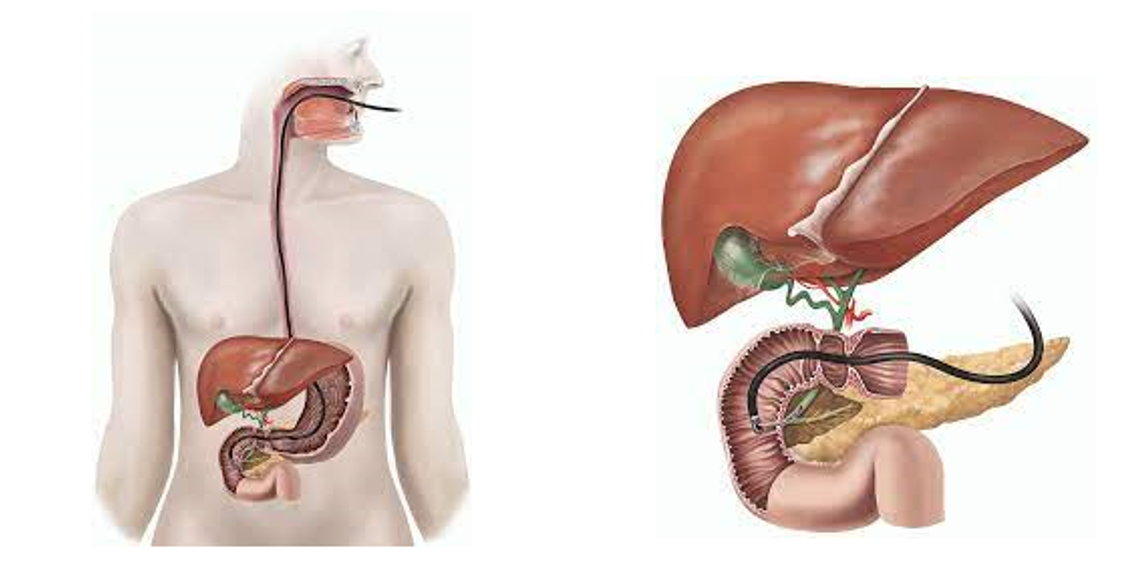
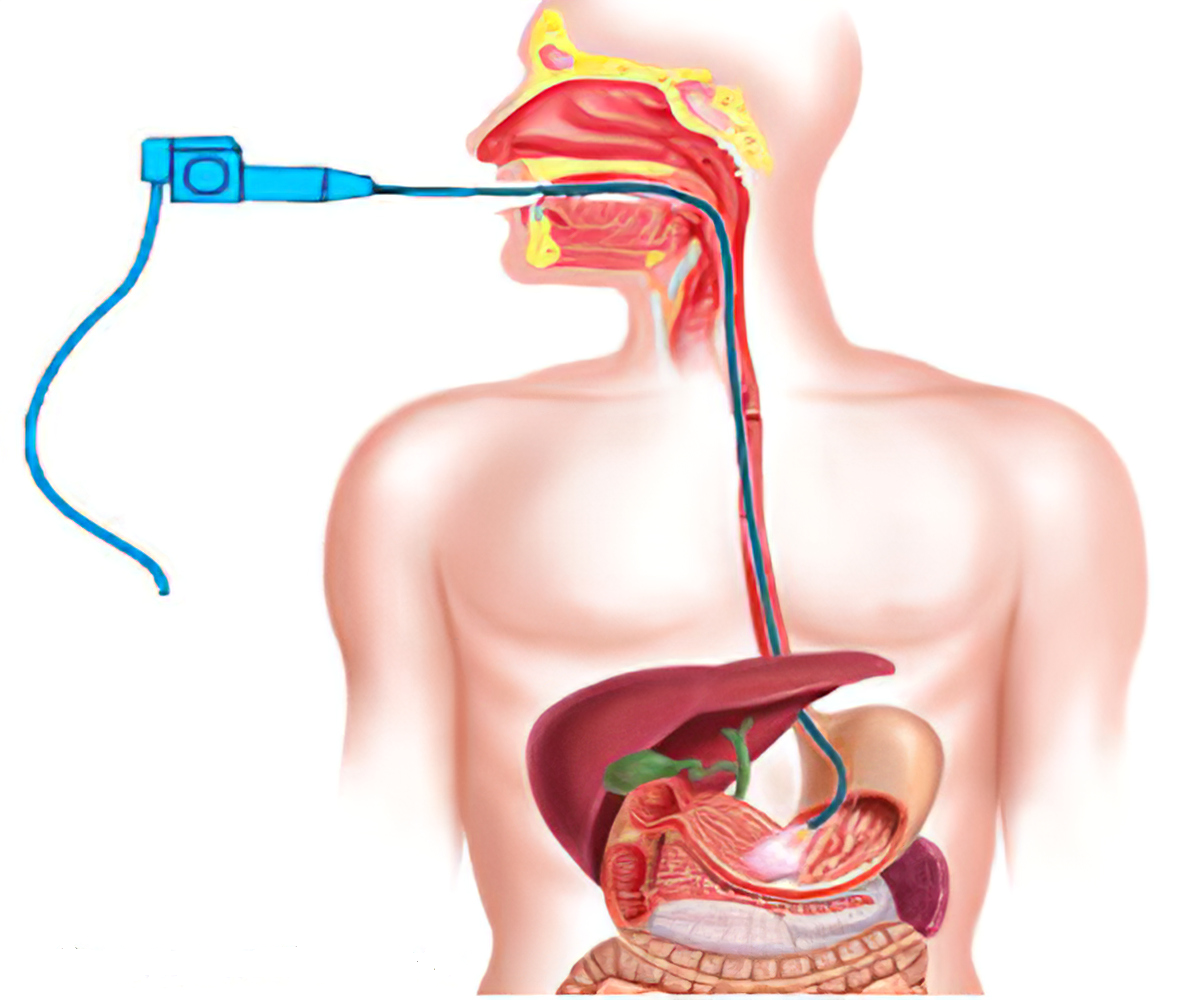
These procedures use a camera on the end of a thin, flexible probe to look at the colon.
The camera is inserted through the anus. It allows your doctor to look for ulcers, fistulas, and other damage in the rectum and colon.
A colonoscopy can examine the entire length of the large intestine. A sigmoidoscopy examines only the last 20 inches of the large intestine — the sigmoid colon.
During these procedures, a small sample of the bowel wall will sometimes be taken. This is called a biopsy. Examining this biopsy under the microscope can be used to diagnose IBD.
4. Capsule endoscopy
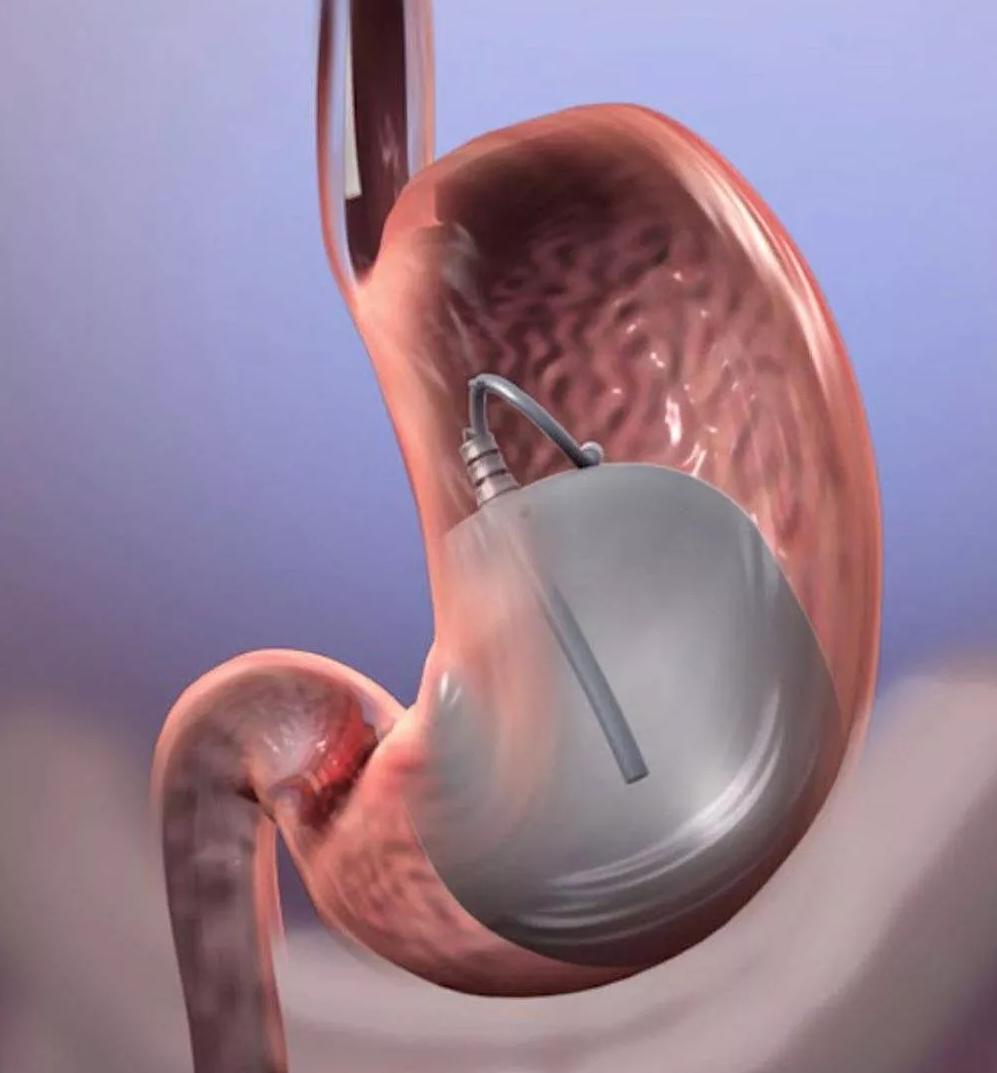
This test inspects the small intestine, which is much harder to examine than the large intestine. For the test, you swallow a small capsule containing a camera.
As it moves through your small intestine, it takes pictures. Once you’ve passed the camera in your stool, the pictures can be seen on a computer.
This test is only used when other tests have failed to find the cause of Crohn’s disease symptoms.
5. Plain film or X-ray
A plain abdominal X-ray is used in emergency situations where intestine rupture is suspected.
6. Computer tomography (CT) and magnetic resonance imaging (MRI)
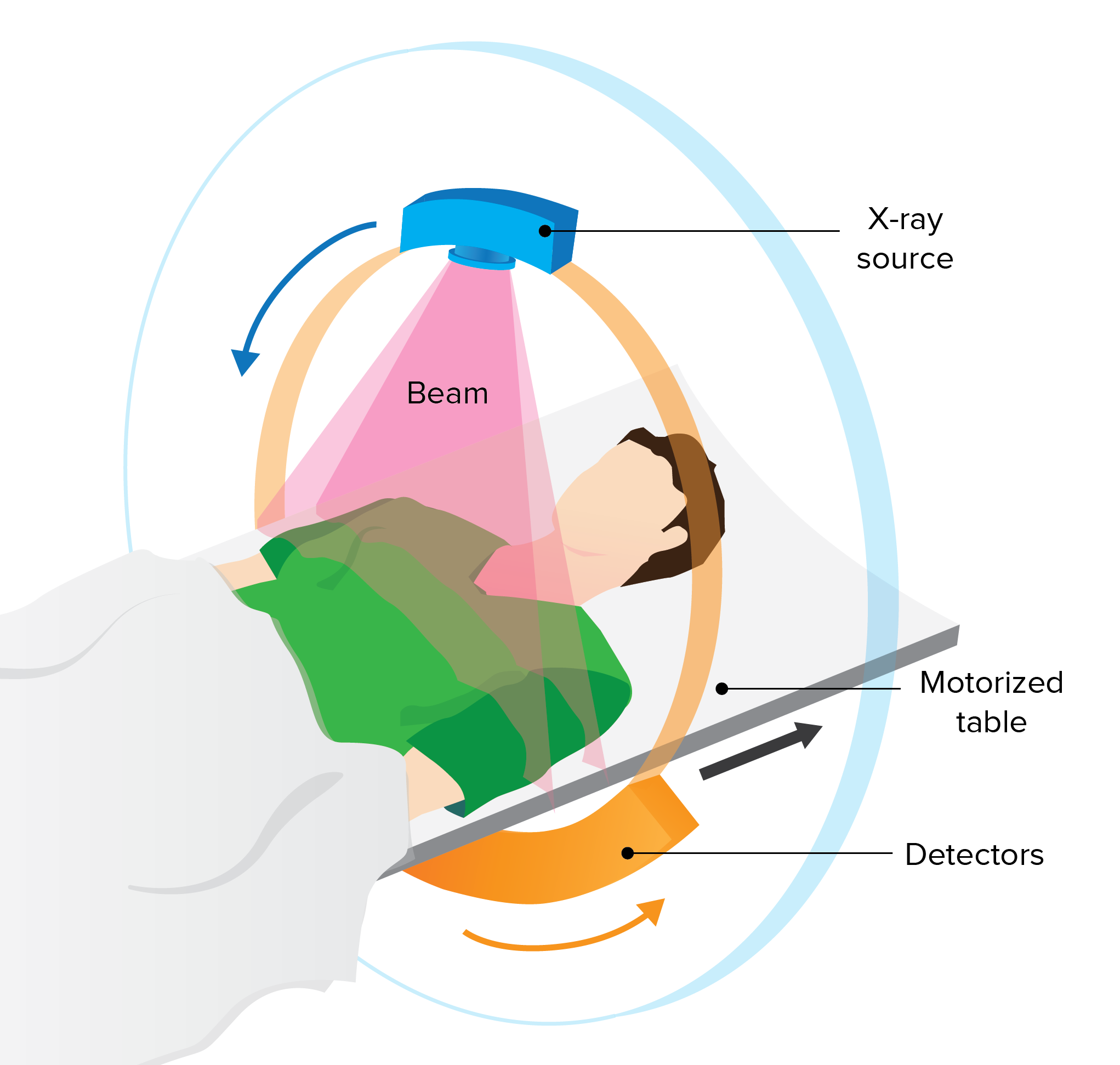
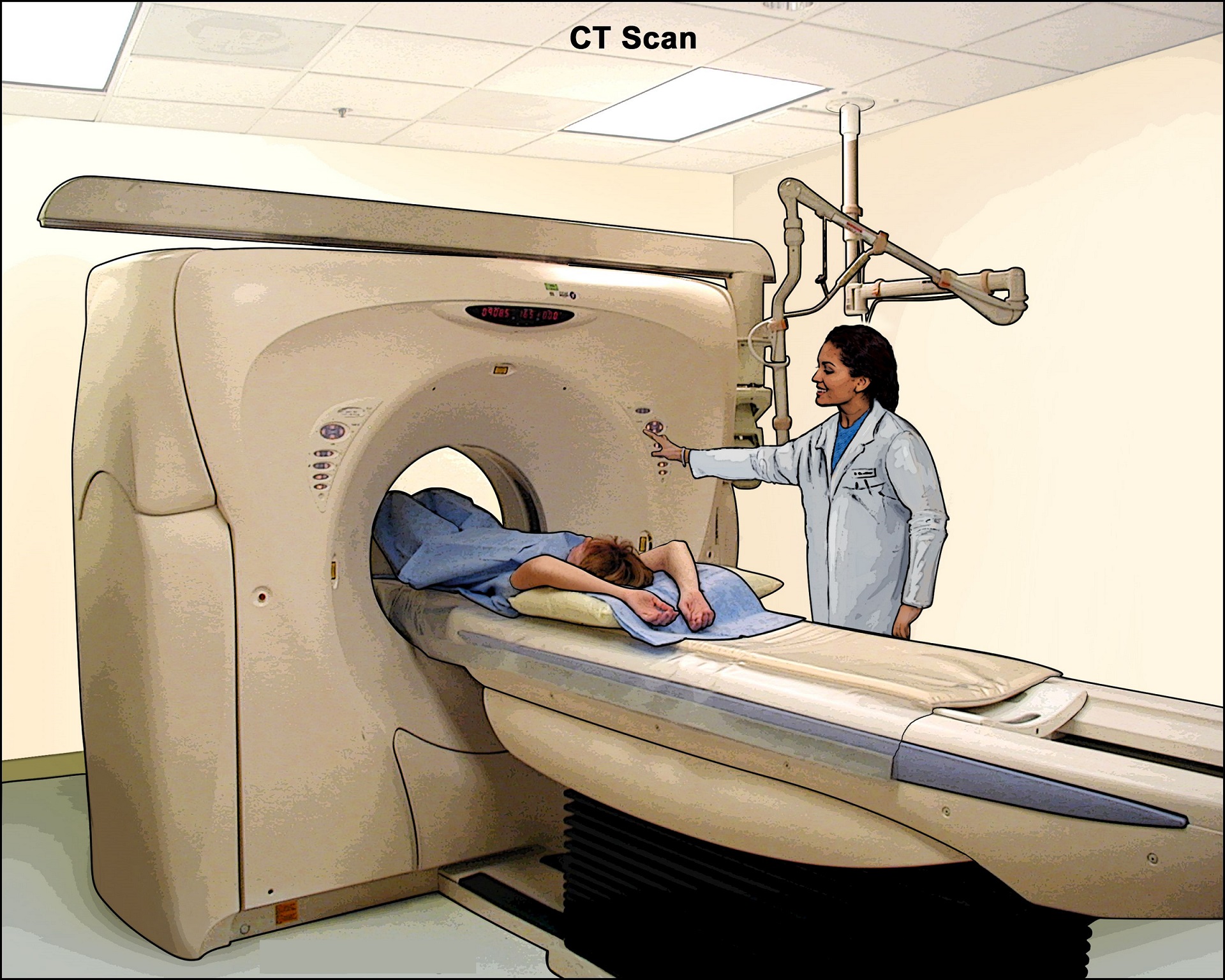
CT scans are basically computerized X-rays. They create a more detailed image than a standard X-ray. This makes them useful for examining the small intestine. They can also detect complications of IBD.
MRIs use magnetic fields to form images of the body. They’re safer than X-rays. MRIs are especially helpful in examining soft tissues and detecting fistulas.
Both MRIs and CT scans can be used to determine how much of the intestine is affected by IBD.
Treatment
There are a number of different treatments for IBD.
1. Medications
Anti-inflammatory drugs are the first step in IBD treatment. These drugs decrease inflammation of the digestive tract. However, they have many side effects.
Anti-inflammatory drugs used for IBD include standard-dose mesalamine, sulfasalazine and its byproducts, and corticosteroids.
Immune suppressants (or immunomodulators) prevent the immune system from attacking the bowel and causing inflammation.
This group includes drugs that block TNF. TNF is a chemical produced by the immune system that causes inflammation. Excess TNF in the blood is normally blocked, but in people with IBD, higher levels of TNF can lead to more inflammation.
Another medication, tofacitinib (Xeljanz), is a newer option that works in a unique way to reduce inflammation.
Immune suppressants can have many side effects, including rashes and infections.
Antibiotics are used to kill bacteria that may trigger or aggravate IBD symptoms.
Antidiarrheal drugs and laxatives can also be used to treat IBD symptoms.
2. Lifestyle choices
Lifestyle choices are important when you have IBD.
Drinking plenty of fluids helps to compensate for those lost in your stool. Avoiding dairy products and stressful situations also improves symptoms.
Exercising and quitting smoking can further improve your health.
3. Supplements
Vitamin and mineral supplements can help with nutritional deficiencies. For example, iron supplements can treat anemia.
Talk to your doctor before adding any new supplements to your diet. Get iron supplements online.
4. Surgery
Surgery can sometimes be necessary for people with IBD. Some IBD surgeries include:
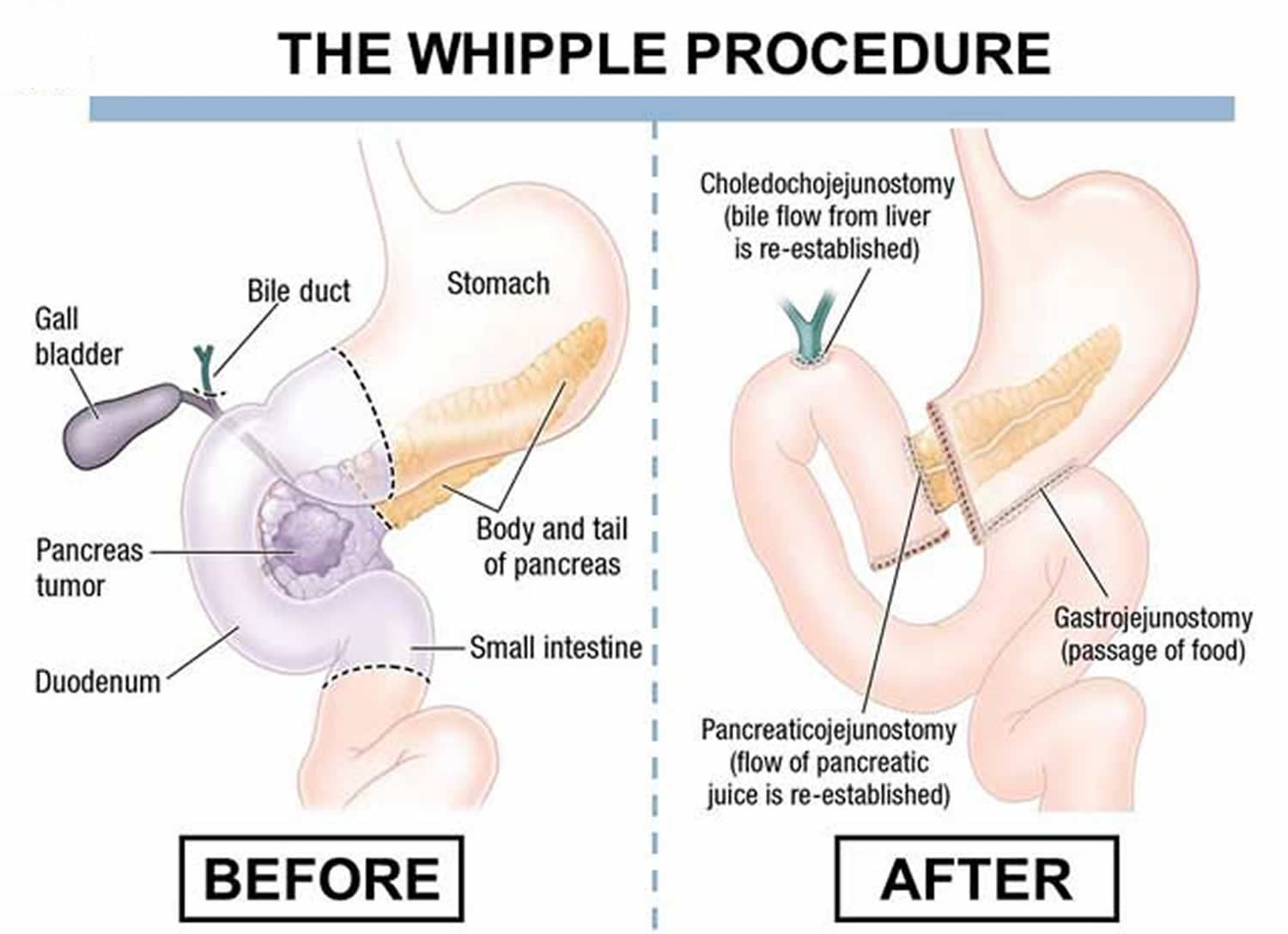
- strictureplasty to widen a narrowed bowel
- closure or removal of fistulas
- removal of affected portions of the intestines, for people with Crohn’s disease
- removal of the entire colon and rectum, for severe cases of ulcerative colitis
Routine colonoscopy is used to monitor for colon cancer, since those with IBD are at a higher risk for developing it.
Prevention
The hereditary causes of IBD can’t be prevented. However, you may be able reduce your risk of developing IBD or prevent a relapse by:
- eating healthy foods
- exercising regularly
- quitting smoking
IBD can cause some discomfort, but there are ways you can manage the disease and still live a healthy, active lifestyle.
Reference
- https://gi.org/topics/inflammatory-bowel-disease/#tabs2
- https://www.mayoclinic.org/diseases-conditions/inflammatory-bowel-disease/symptoms-causes/syc-20353315