Liver Injury From Medication
OVERVIEW | CAUSES | RISK FACTORS | SYMPTOMS | COMPLICATION | DIAGNOSIS | TREATMENT | PREVENTION | REFERENCES

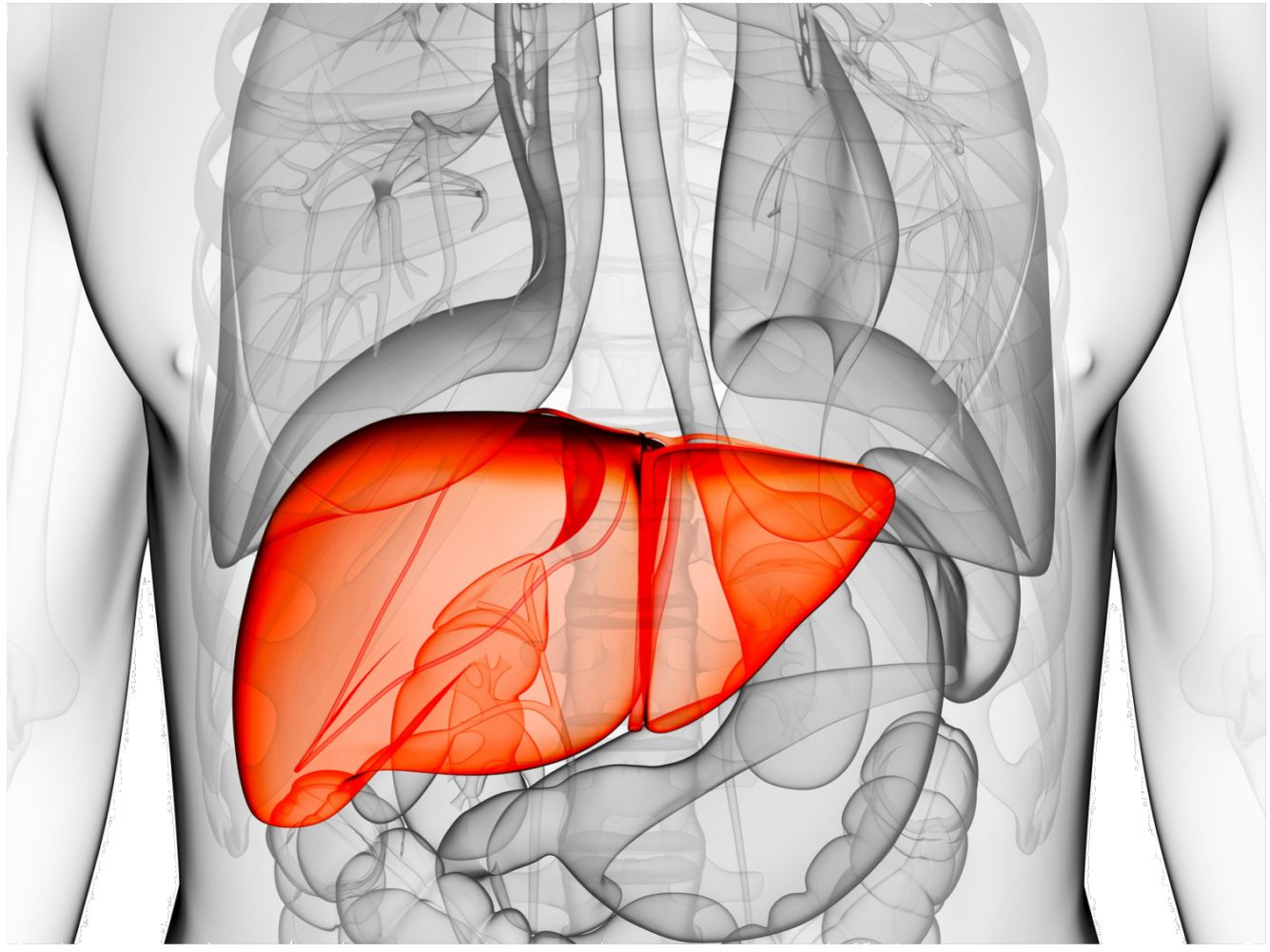
OVERVIEW
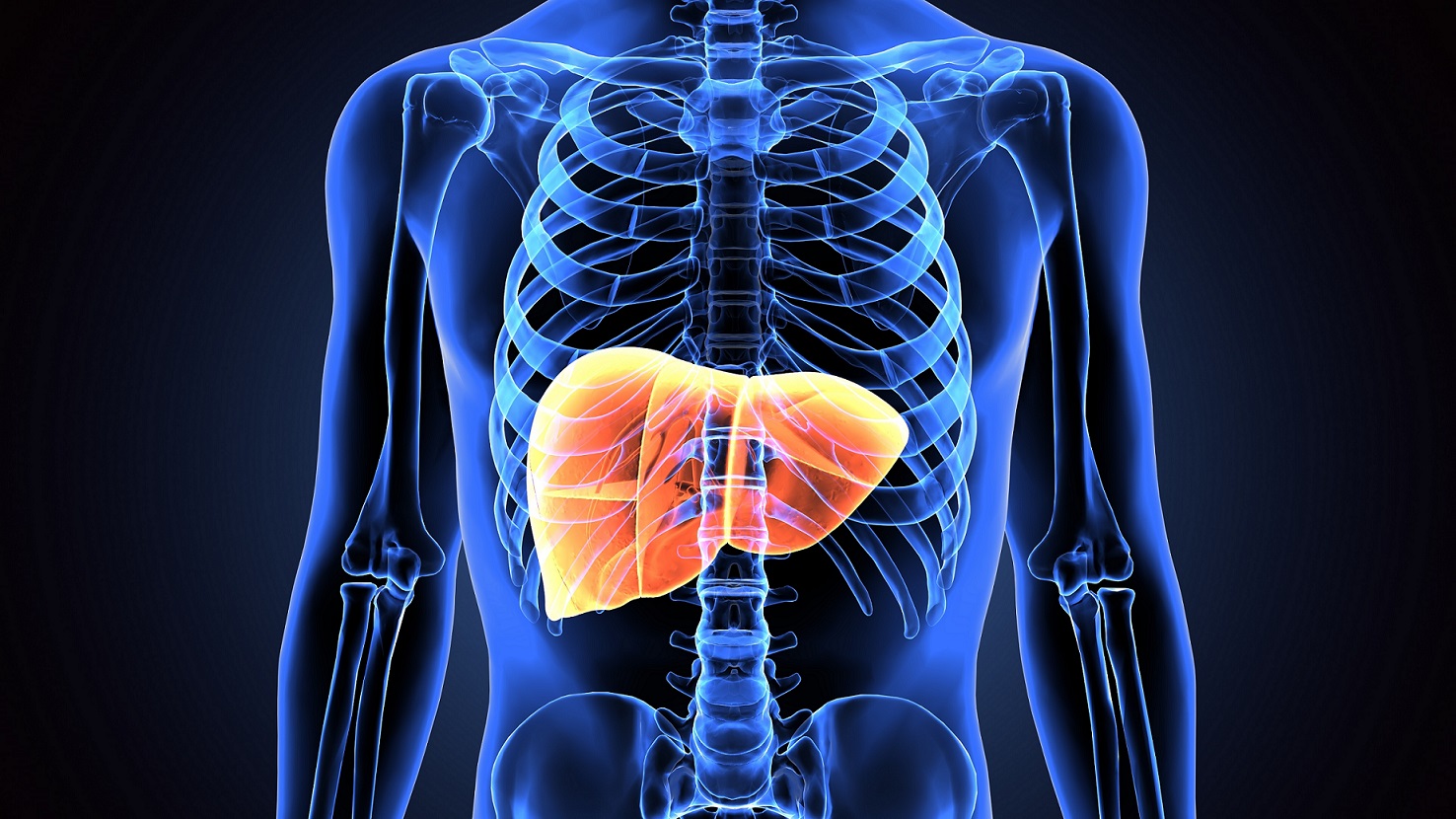
One of the main functions of the liver is to break down substances that we take by mouth, including medications, herbs and supplements. This process usually takes place efficiently and without causing any harm. When new medications are developed, they are extensively tested in many people prior to being approved for general use. During this period careful tests are done to ensure that the liver is not damaged. For this reason, the vast majority of the medications currently available are safe even for people with known liver disease.
Despite these safeguards sometimes medications can harm the liver. In some instances, a person can have a rare tendency that makes their liver susceptible to injury after taking a certain medication – we call this an idiosyncratic reaction. It happens in very rare instances and often cannot be predicted. Occasionally, medications that proved safe during testing are found to be potentially harmful when they are released for general use and millions of people take it. In other instances, people with liver disease may be at increased risk of developing liver damage when certain medications are used. Medications that are known to be toxic to people with liver disease usually carry a warning regarding its use in people with liver problems.
CAUSES
Drugs can cause liver disease in several ways. Some drugs are directly injurious to the liver; others are transformed by the liver into chemicals that can cause injury to the liver directly or indirectly. (This may seem strange in light of the liver's important role in transforming toxic chemicals into nontoxic chemicals, but it happens.) There are three types of liver toxicity; dose-dependent toxicity, idiosyncratic toxicity, and drug allergy.
Drugs that cause dose-dependent toxicity can cause liver disease in most people if enough of the drug is taken. The most important example of dose-dependent toxicity is acetaminophen (Tylenol) overdose.
Drugs that cause idiosyncratic toxicity cause disease in only those few patients who have inherited specific genes that control the chemical transformation of that specific drug, causing accumulation of the drug or products of their transformation (metabolites) that are injurious to the liver. These inherited idiosyncratic toxicities usually are rare, however, with some drugs the prevalence of toxicity is much higher. Even though the risk of developing drug-induced idiosyncratic liver disease is low, idiosyncratic liver disease is the most common form of drug-induced liver disease because tens of millions of patients are using drugs, and many of them are using several drugs.
Drug allergy also may cause liver disease, though it is uncommon. In drug allergy, the liver is injured by the inflammation that occurs when the body's immune system attacks the drugs with antibodies and immune cells.
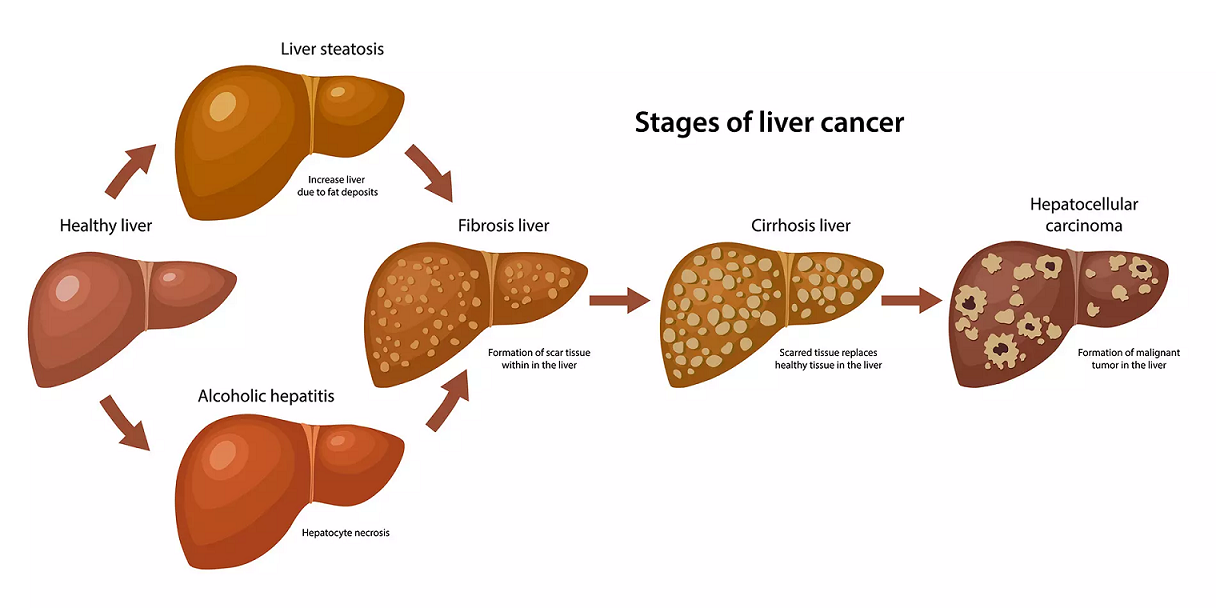
Drugs and chemicals can cause a wide spectrum of liver injury. These include:
- Mild elevations in blood levels of liver enzymes without symptoms or signs of liver disease
- Hepatitis (inflammation of liver cells)
- Necrosis (death of liver cells) that often is caused by more severe hepatitis
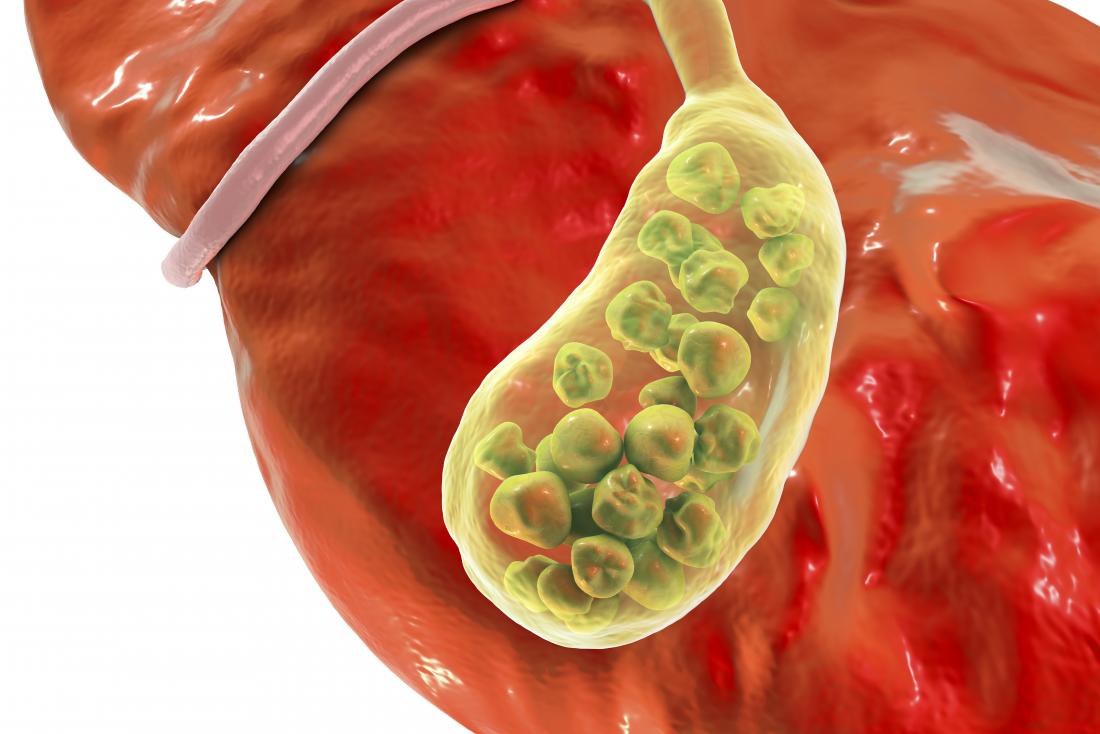
- Cholestasis (decreased secretion and/or flow of bile)
- Steatosis (accumulation of fat in the liver)
- Cirrhosis (advanced scarring of the liver) as a result of chronic hepatitis, cholestasis, or fatty liver
- Mixed disease, for example both hepatitis and necrosis of liver cells, hepatitis and fat accumulation, or cholestasis and hepatitis.
- Fulminant hepatitis with severe, life threatening liver failure
- Blood clots in the veins of the liver.
RISK FACTORS
The risk for drug-induced hepatitis varies with each medicine.
You may be at higher risk for drug-induced liver injuries if you:
- Have liver disease, such as from long-term alcohol use, HIV, or viral hepatitis
- Drink alcohol and take medicines at the same time
- Are older
- Are a woman
- Use long-acting or extended release medicines
- Take multiple medicines that contain acetaminophen. There are many medicines both over-the-counter and prescription with acetaminophen.
- Use herbal supplements
SYMPTOMS
In most cases substantial liver damage can occur before symptoms appear. Typical symptoms of liver disease may include nausea, lack of appetite, discomfort on the right upper corner of the abdomen, generalized itching, dark urine and jaundice (yellow discoloration of the eyes and skin), but many people have no symptoms at all. Blood tests can usually detect evidence of liver damage before symptoms develop. When a medication known to possibly cause liver damage is used, your physician may recommend that blood tests be checked periodically after starting the medication so that any evidence of liver damage can be detected before symptoms appear.
COMPLICATIONS
Rarely, drug-induced liver injury can lead to liver failure.
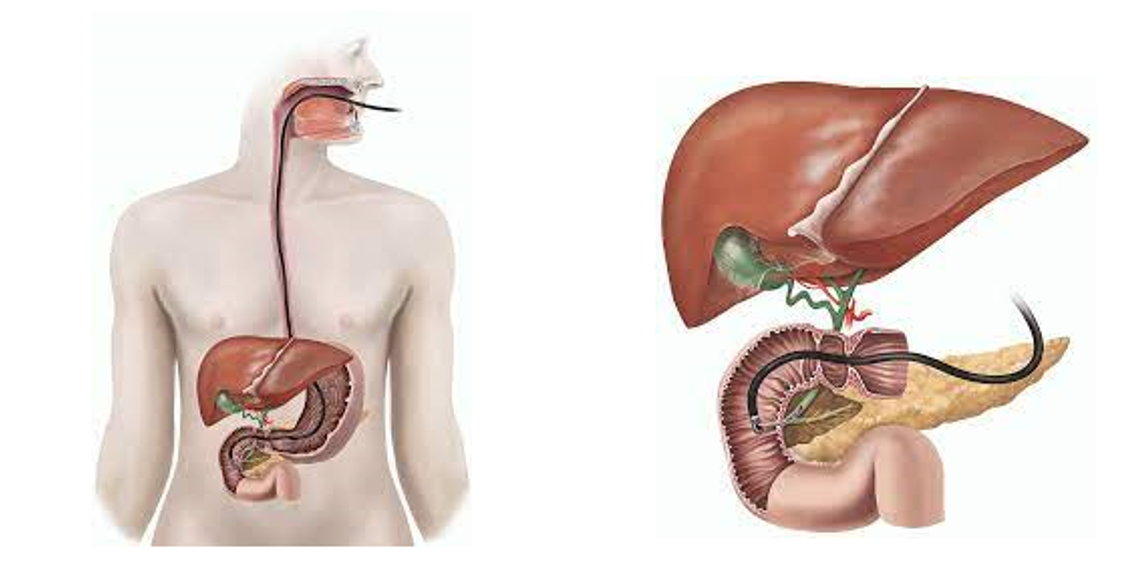
DIAGNOSIS
Liver damage of any type is usually detected by doing blood tests. Usually there is no need to monitor the liver tests when a medication is started. If your physician is planning on using a medication that in the past has been shown to rarely cause liver damage, the most common test used to monitor the liver is a liver panel, which consists of several blood tests that detect liver damage. These tests are: AST (aspartate aminotransferase), ALT (alanine aminotransferase), AP (alkaline phosphatase) and bilirubin. There are many other causes for elevated liver tests. For that reason your physician may obtain a baseline liver panel prior to starting a medication to be sure that it is normal.
Minor elevations of these tests may occur after starting a medication and do not indicate significant liver damage. Generally speaking physicians are most concerned about serious medication-induced liver damage when the levels of AST and ALT rise 3 to 5 times or more over baseline or if there is an increase in bilirubin. If the elevations are minor, the medication is continued and the liver tests monitored. In most cases, the liver tests will return to normal despite continuing the medication.
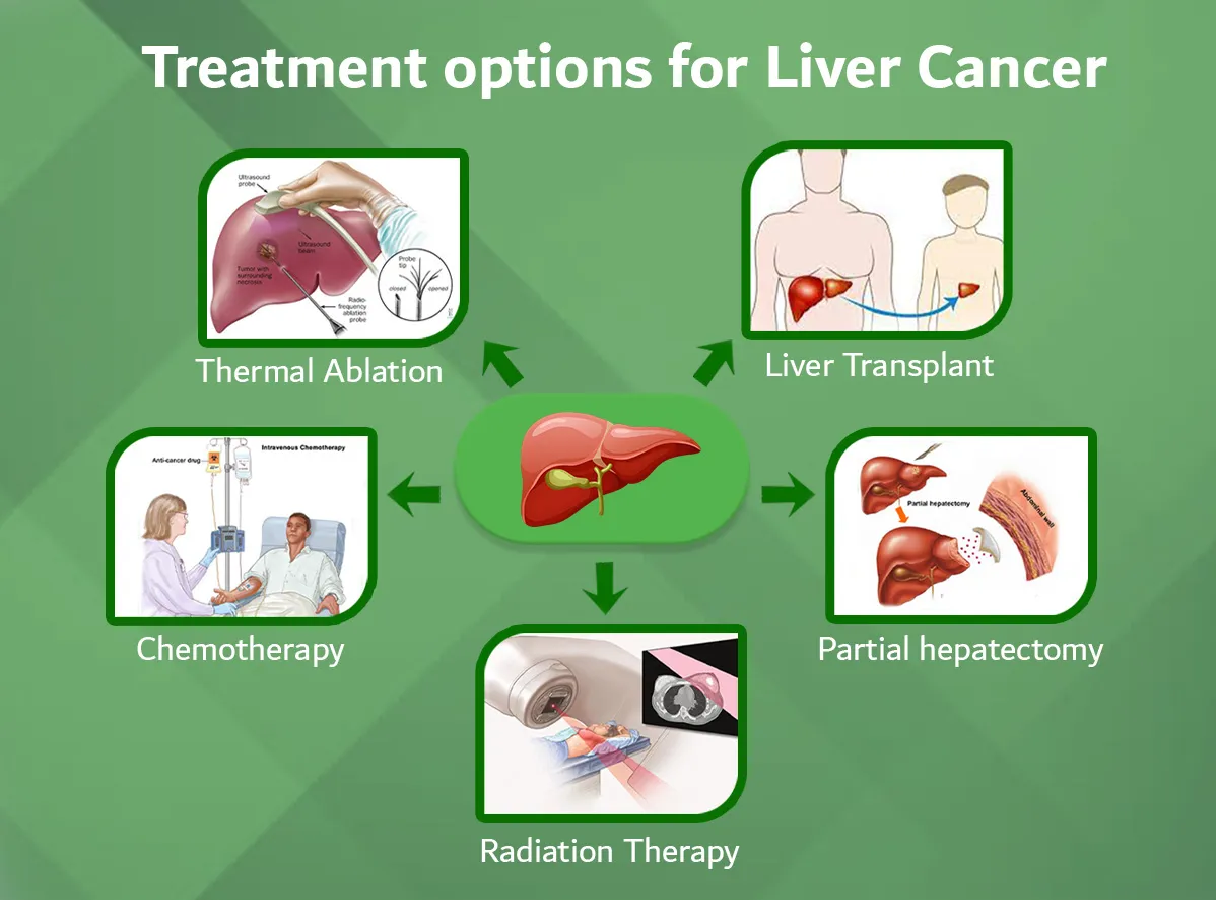
TREATMENT
The most important treatment for drug-induced liver disease is stopping the drug that is causing the liver disease. In most patients, signs and symptoms of liver disease will resolve and blood tests will become normal and there will be no long-term liver damage. There are exceptions, however. For example, Tylenol overdoses are treated with oral N-acetylcysteine to prevent severe liver necrosis and failure. Liver transplantation may be necessary for some patients with acute liver failure. Some drugs also can cause irreversible liver damage and cirrhosis.
Never use more than the recommended dose of over-the-counter medicines containing acetaminophen (Tylenol).
DO NOT take these medicines if you drink heavily or regularly; talk to your provider about safe doses.
Always tell your provider about all the medicines you take, including over-the-counter drugs and herbal or supplemental preparations. This is very important if you have liver disease.
Talk to your provider about other medicines you may need to avoid. Your provider can tell you which medicines are safe for you.
REFERENCE
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3157241/
- https://medlineplus.gov/ency/article/000226.htm
- https://www.hopkinsmedicine.org/health/conditions-and-diseases/hepatitis/druginduced-hepatitis
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3160634/
- https://gi.org/topics/medications-and-the-liver/