Ulcerative Colitis
OVERVIEW | CAUSES | RISK FACTORS | SYMPTOMS | COMPLICATION | Diagnosis | TREATMENT | PREVENTION | REFERENCES

Overview
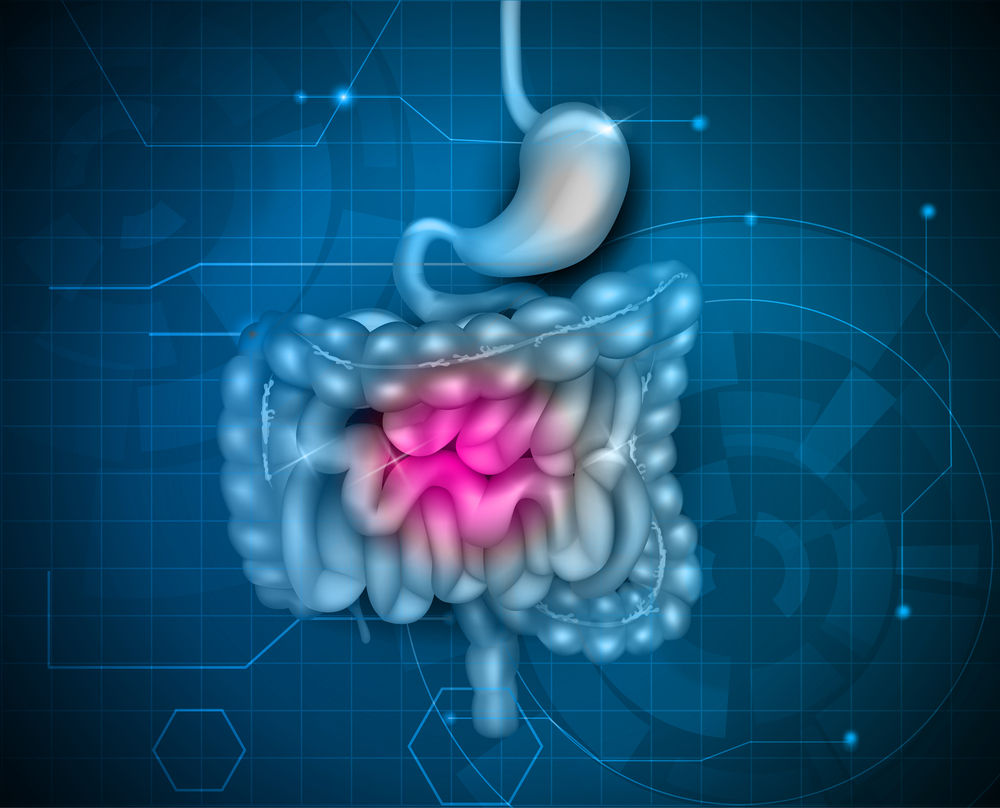
Ulcerative colitis is an inflammatory bowel disease (IBD) that causes inflammation and ulcers (sores) in your digestive tract. Ulcerative colitis affects the innermost lining of your large intestine (colon) and rectum. Symptoms usually develop over time, rather than suddenly.
Ulcerative colitis can be debilitating and can sometimes lead to life-threatening complications. While it has no known cure, treatment can greatly reduce signs and symptoms of the disease and bring about long-term remission.
Causes
The exact cause of ulcerative colitis remains unknown. Previously, diet and stress were suspected, but now doctors know that these factors may aggravate but don't cause ulcerative colitis.
One possible cause is an immune system malfunction. When your immune system tries to fight off an invading virus or bacterium, an abnormal immune response causes the immune system to attack the cells in the digestive tract, too.
Heredity also seems to play a role in that ulcerative colitis is more common in people who have family members with the disease. However, most people with ulcerative colitis don't have this family history.
Risk factors
Ulcerative colitis affects about the same number of women and men. Risk factors may include:
- Age. Ulcerative colitis usually begins before the age of 30. But, it can occur at any age, and some people may not develop the disease until after age 60.
- Race or ethnicity. Although whites have the highest risk of the disease, it can occur in any race. If you're of Ashkenazi Jewish descent, your risk is even higher.
- Family history. You're at higher risk if you have a close relative, such as a parent, sibling or child, with the disease.
Symptoms
Ulcerative colitis symptoms can vary, depending on the severity of inflammation and where it occurs. Signs and symptoms may include:
- Diarrhea, often with blood or pus
- Abdominal pain and cramping
- Rectal pain
- Rectal bleeding — passing small amount of blood with stool
- Urgency to defecate
- Inability to defecate despite urgency
- Weight loss
- Fatigue
- Fever
- In children, failure to grow
Most people with ulcerative colitis have mild to moderate symptoms. The course of ulcerative colitis may vary, with some people having long periods of remission.
Types
Doctors often classify ulcerative colitis according to its location. Types of ulcerative colitis include:
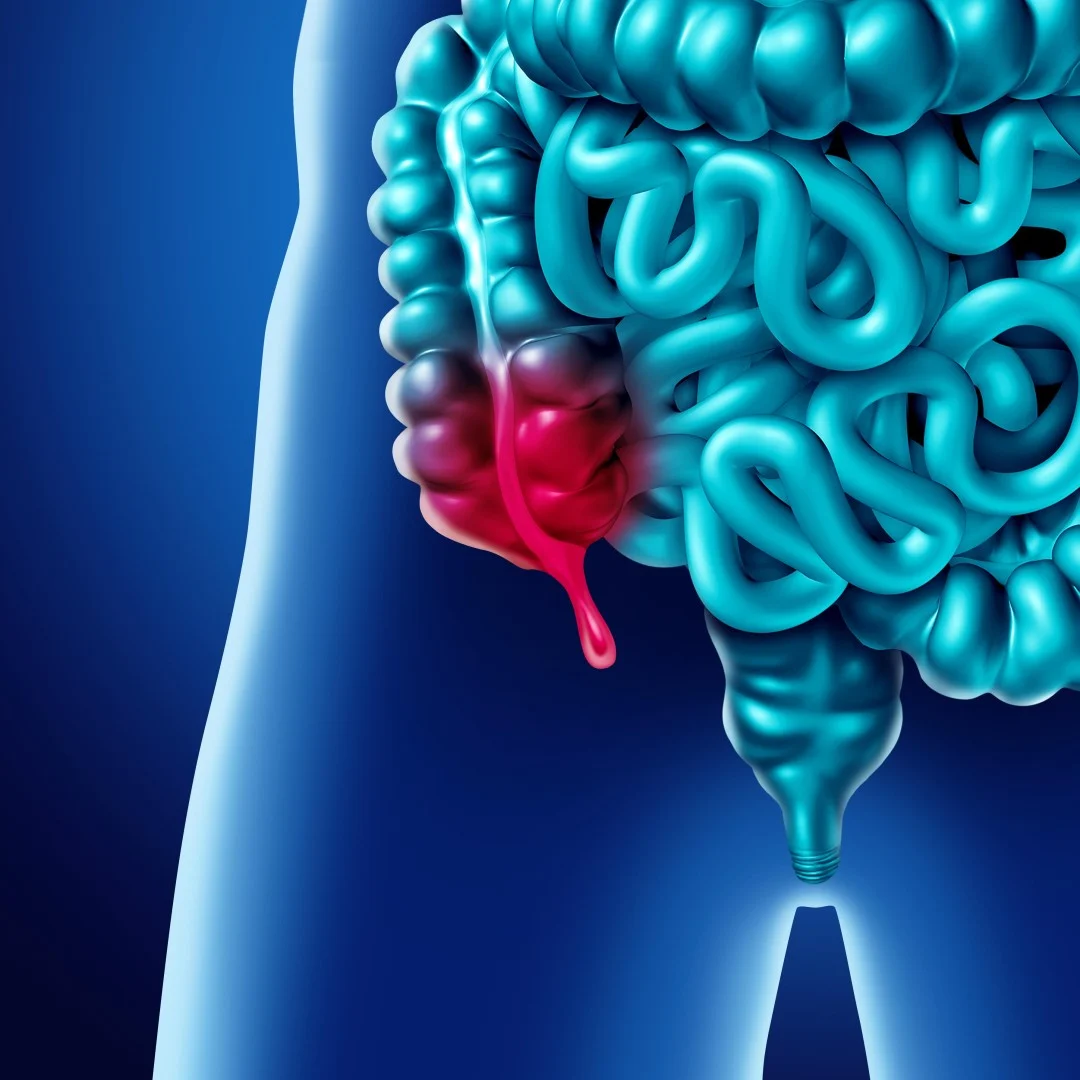
- Ulcerative proctitis. Inflammation is confined to the area closest to the anus (rectum), and rectal bleeding may be the only sign of the disease.
- Proctosigmoiditis. Inflammation involves the rectum and sigmoid colon — the lower end of the colon. Signs and symptoms include bloody diarrhea, abdominal cramps and pain, and an inability to move the bowels in spite of the urge to do so (tenesmus).
- Left-sided colitis. Inflammation extends from the rectum up through the sigmoid and descending colon. Signs and symptoms include bloody diarrhea, abdominal cramping and pain on the left side, and urgency to defecate.
- Pancolitis. This type often affects the entire colon and causes bouts of bloody diarrhea that may be severe, abdominal cramps and pain, fatigue, and significant weight loss.
Complications
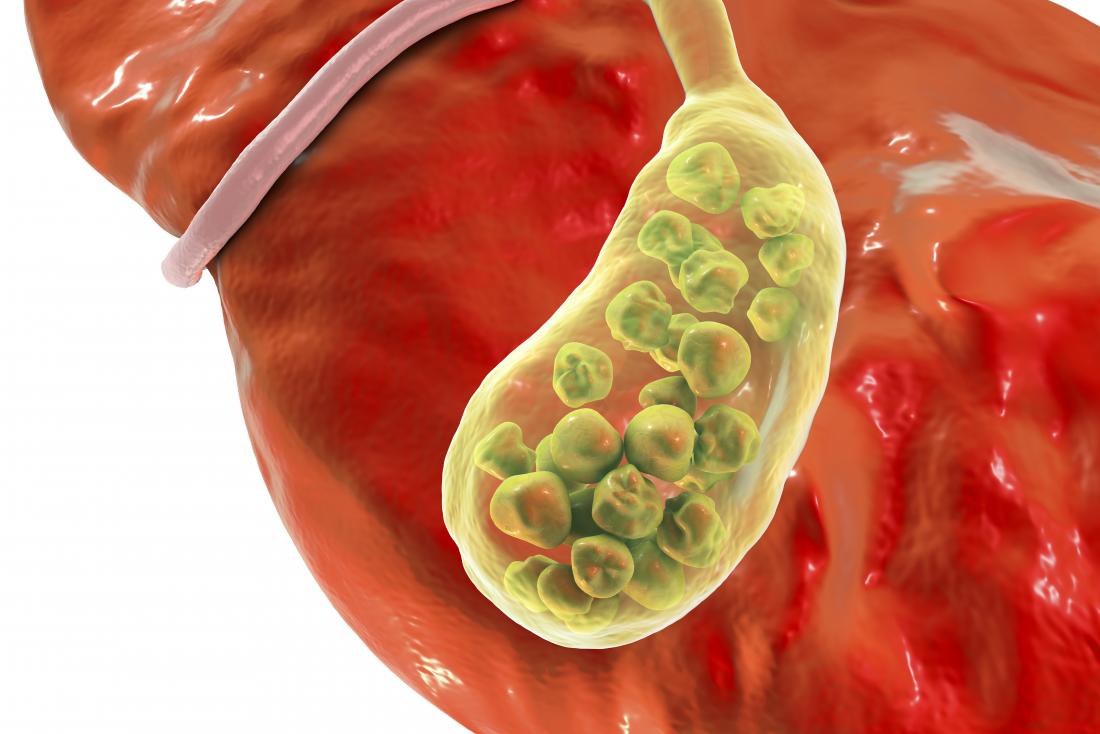
Possible complications of ulcerative colitis include:
- Severe bleeding
- A hole in the colon (perforated colon)
- Severe dehydration
- Bone loss (osteoporosis)
- Inflammation of your skin, joints and eyes
- An increased risk of colon cancer
- A rapidly swelling colon (toxic megacolon)
- Increased risk of blood clots in veins and arteries
Diagnosis
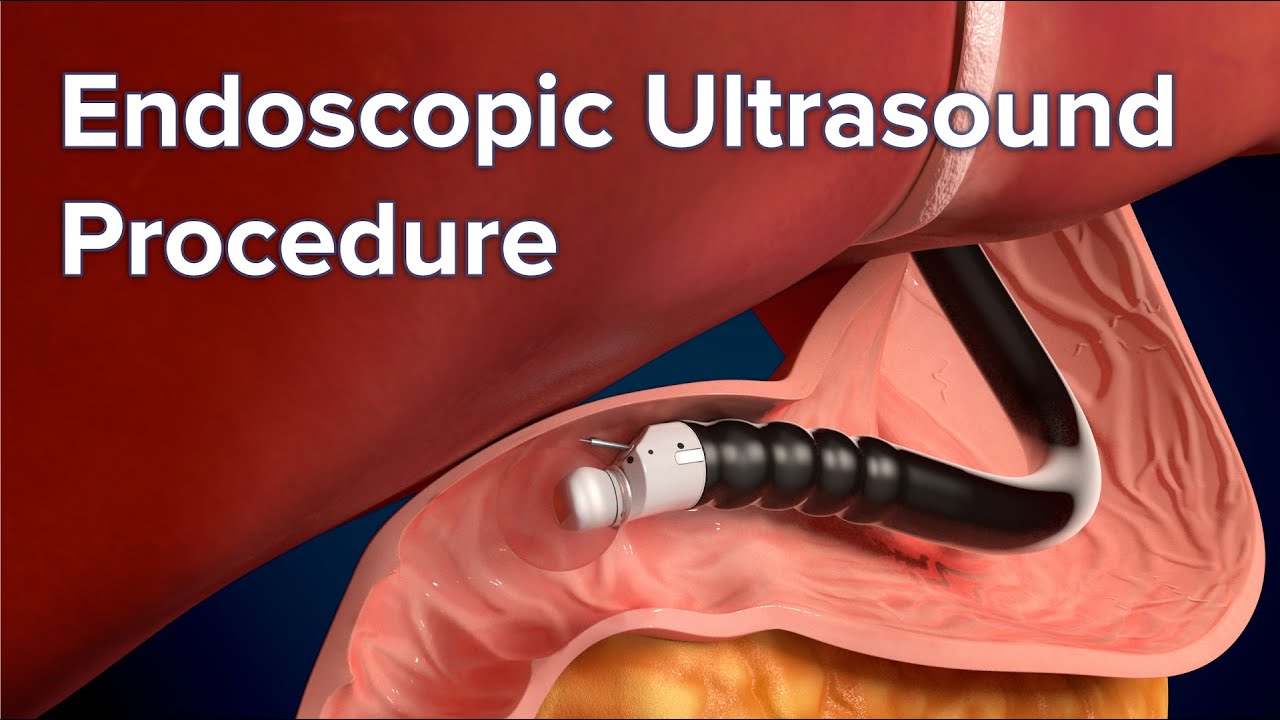
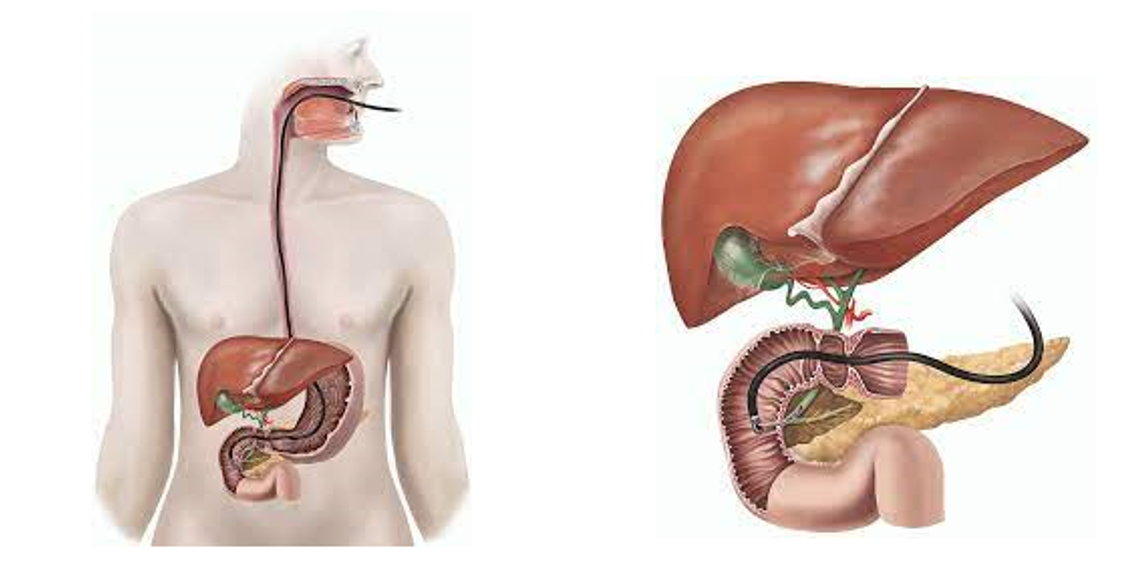
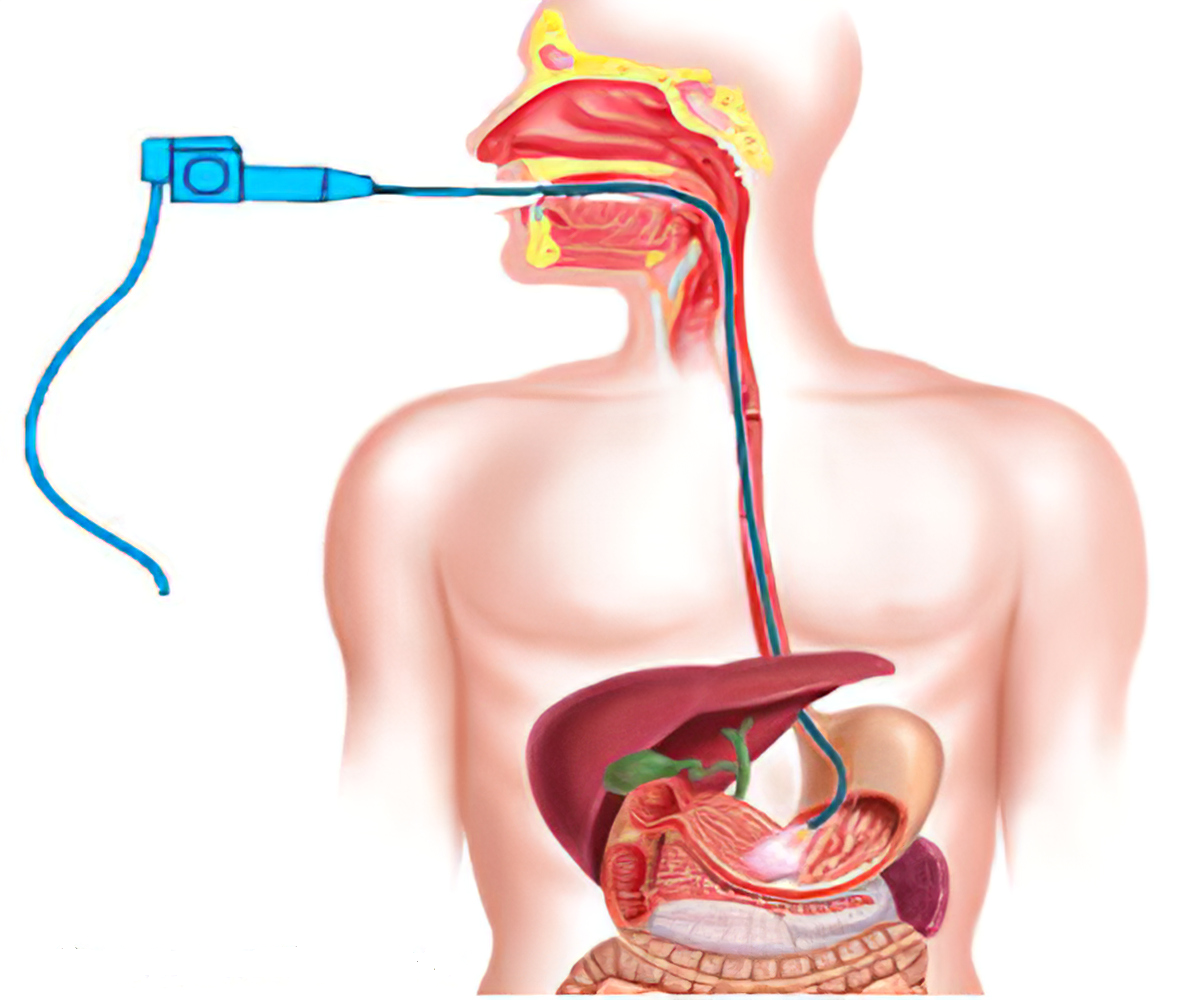
Endoscopic procedures with tissue biopsy are the only way to definitively diagnose ulcerative colitis. Other types of tests can help rule out complications or other forms of inflammatory bowel disease, such as Crohn's disease.
To help confirm a diagnosis of ulcerative colitis, you may have one or more of the following tests and procedures:
Lab tests
- Blood tests. Your doctor may suggest blood tests to check for anemia — a condition in which there aren't enough red blood cells to carry adequate oxygen to your tissues — or to check for signs of infection.
- Stool studies. White blood cells or certain proteins in your stool can indicate ulcerative colitis. A stool sample can also help rule out other disorders, such as infections caused by bacteria, viruses and parasites.
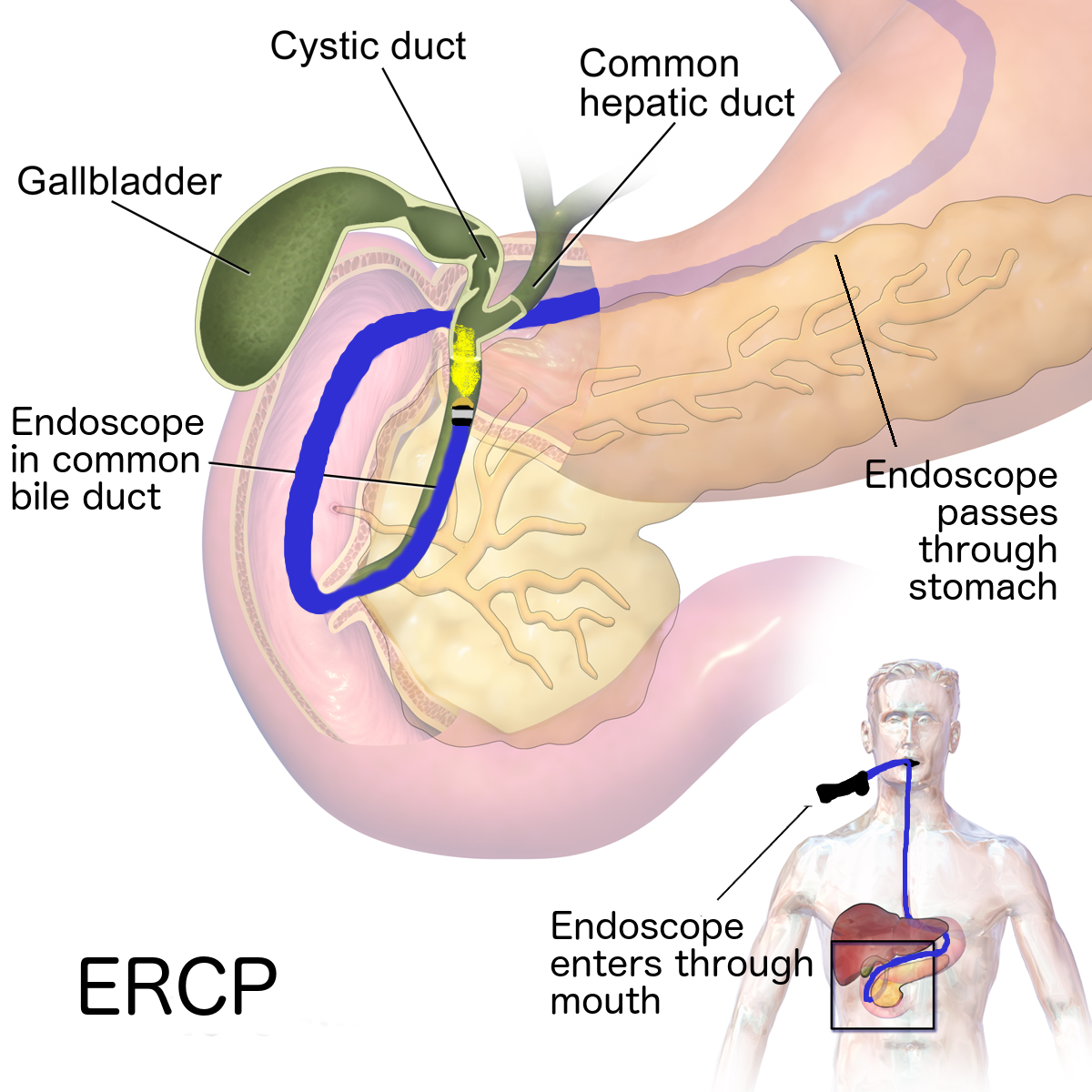
Endoscopic procedures
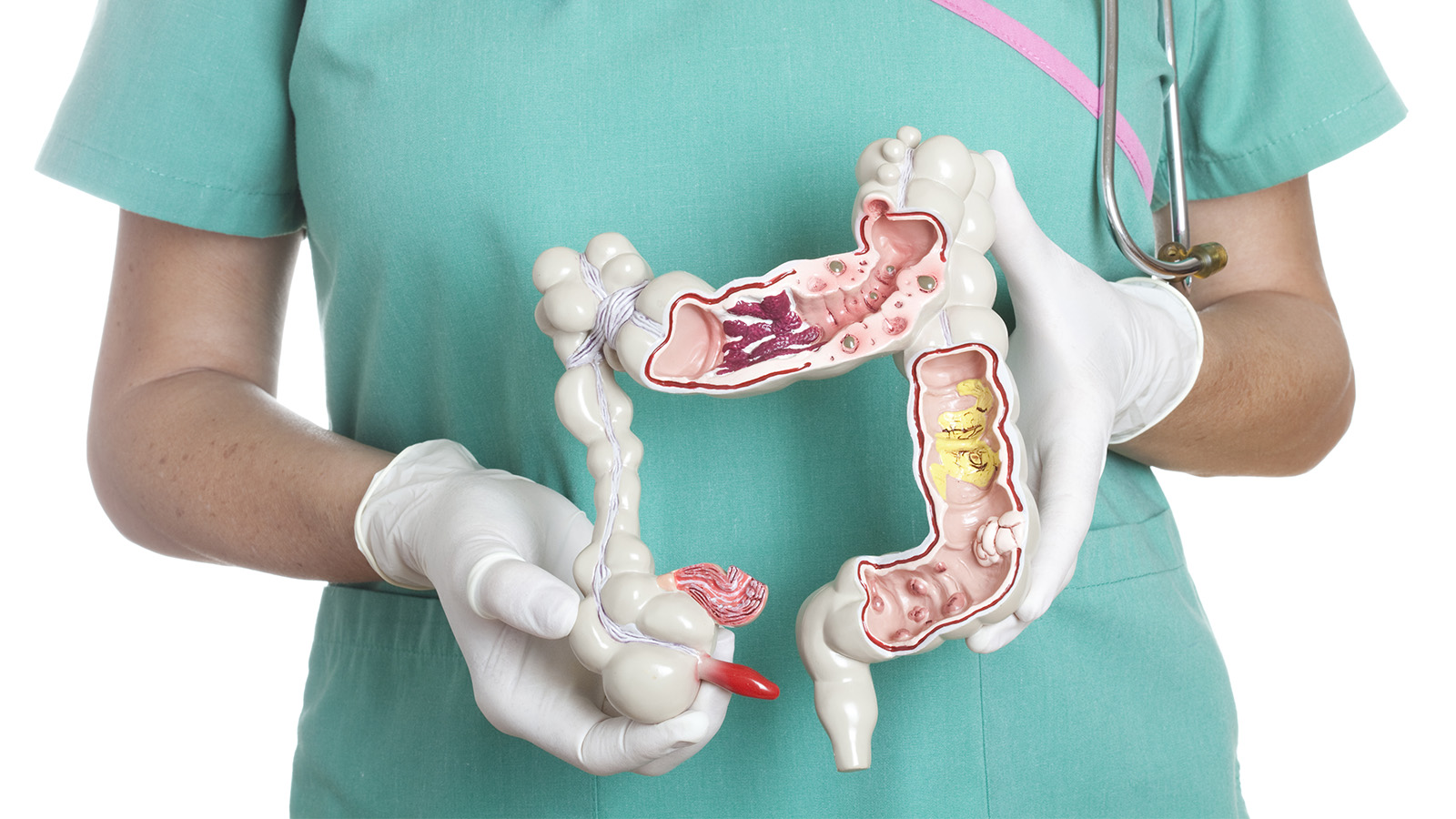
- Colonoscopy. This exam allows your doctor to view your entire colon using a thin, flexible, lighted tube with a camera on the end. During the procedure, your doctor can also take small samples of tissue (biopsy) for laboratory analysis. A tissue sample is necessary to make the diagnosis.
- Flexible sigmoidoscopy. Your doctor uses a slender, flexible, lighted tube to examine the rectum and sigmoid colon — the lower end of your colon. If your colon is severely inflamed, your doctor may perform this test instead of a full colonoscopy.
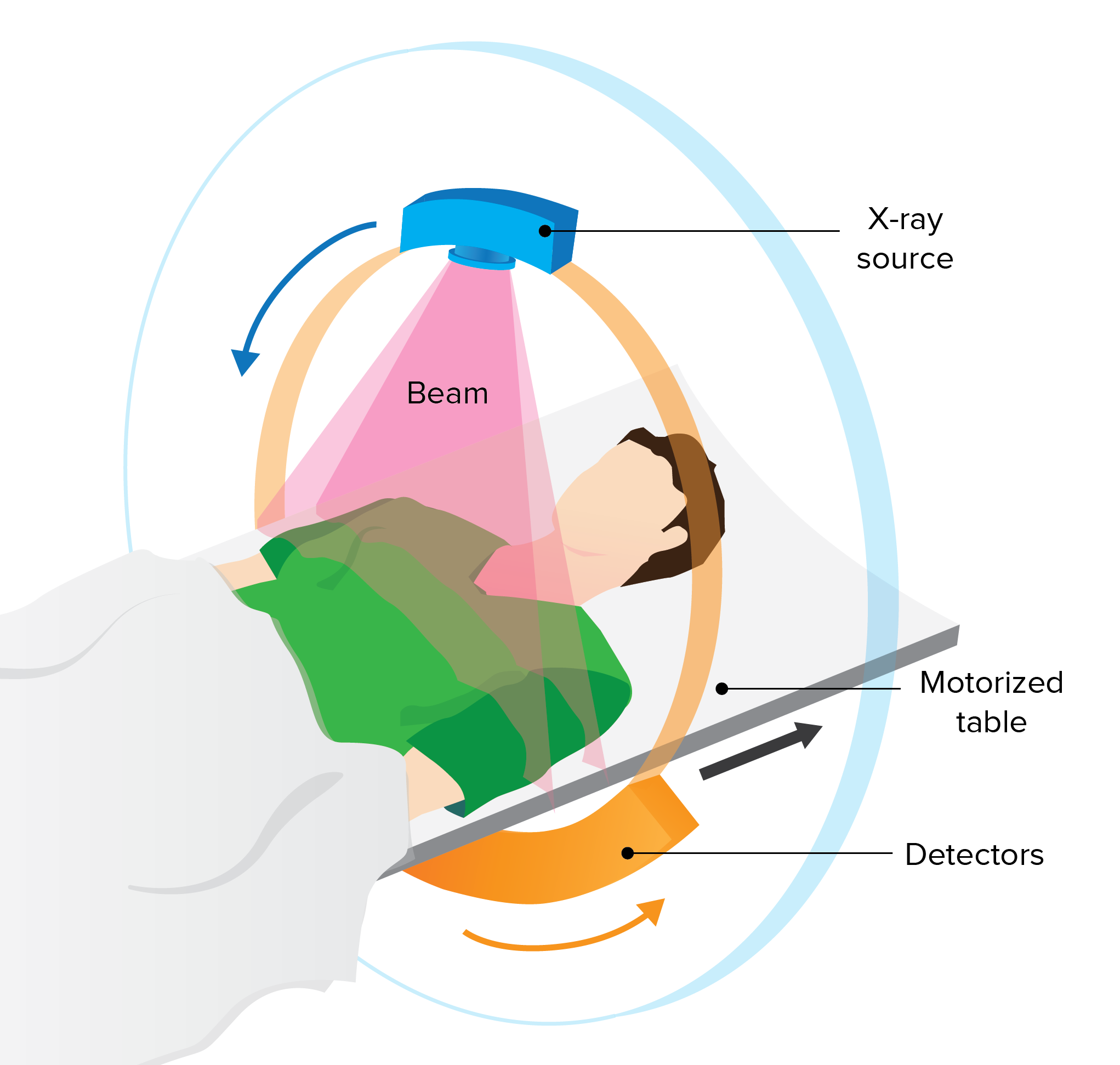
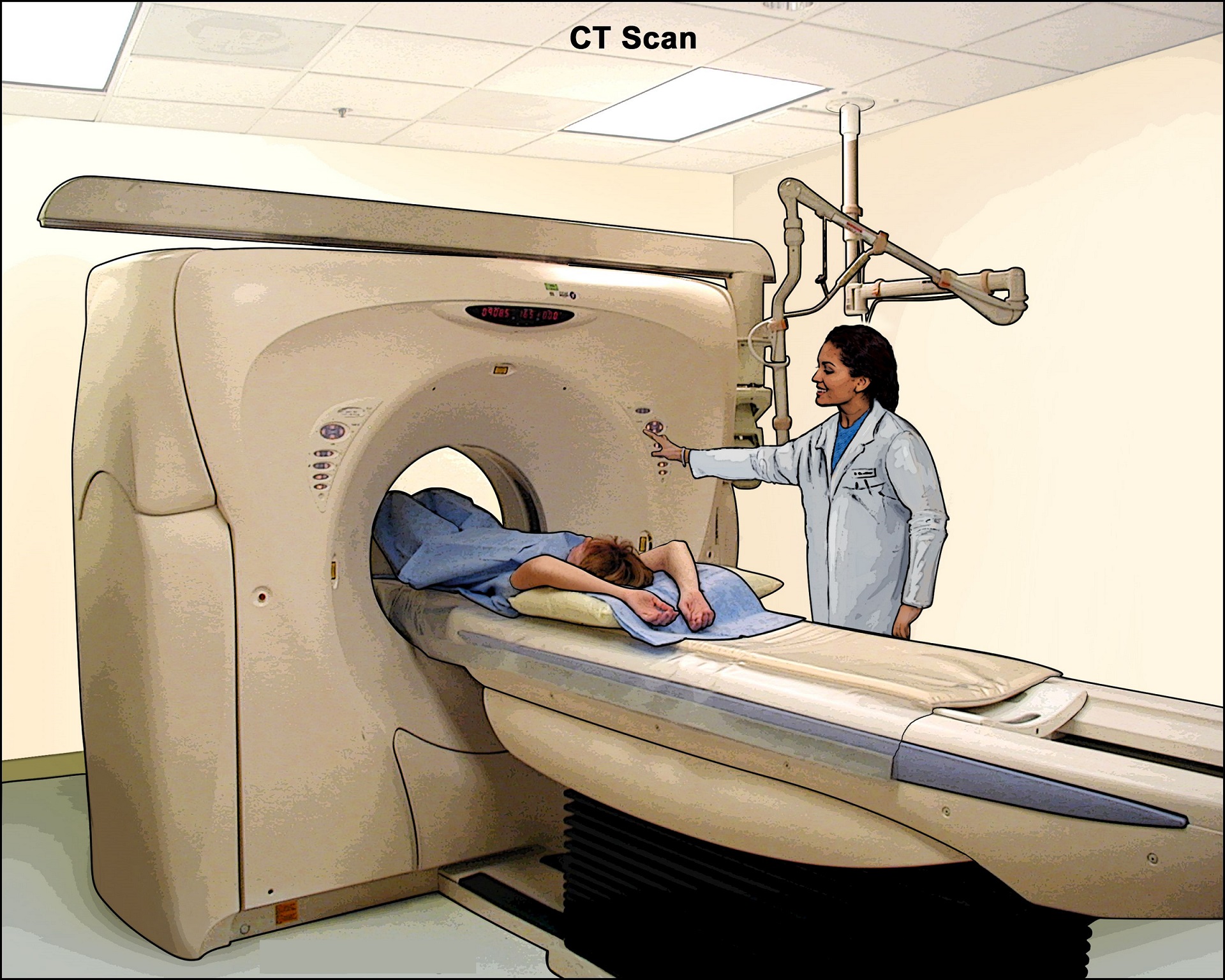
Imaging procedures
- X-ray. If you have severe symptoms, your doctor may use a standard X-ray of your abdominal area to rule out serious complications, such as a perforated colon.
- CT scan. A CT scan of your abdomen or pelvis may be performed if your doctor suspects a complication from ulcerative colitis. A CT scan may also reveal how much of the colon is inflamed.
- Computerized tomography (CT) enterography and magnetic resonance (MR) enterography. Your doctor may recommend one of these noninvasive tests if he or she wants to exclude any inflammation in the small intestine. These tests are more sensitive for finding inflammation in the bowel than are conventional imaging tests. MR enterography is a radiation-free alternative.
Treatment
Ulcerative colitis treatment usually involves either drug therapy or surgery.
Several categories of drugs may be effective in treating ulcerative colitis. The type you take will depend on the severity of your condition. The drugs that work well for some people may not work for others, so it may take time to find a medication that helps you.
In addition, because some drugs have serious side effects, you'll need to weigh the benefits and risks of any treatment.
Anti-inflammatory drugs
Anti-inflammatory drugs are often the first step in the treatment of ulcerative colitis and appropriate for the majority of people with this condition. They include:
-
5-aminosalicylates. Examples of this type of medication include sulfasalazine (Azulfidine), mesalamine (Asacol HD, Delzicol, others), balsalazide (Colazal) and olsalazine (Dipentum). Which one you take, and whether it is taken by mouth or as an enema or suppository, depends on the area of your colon that's affected.
-
Corticosteroids. These drugs, which include prednisone and budesonide, are generally reserved for moderate to severe ulcerative colitis that doesn't respond to other treatments. Due to the side effects, they are not usually given long term.
Immune system suppressors
These drugs also reduce inflammation, but they do so by suppressing the immune system response that starts the process of inflammation. For some people, a combination of these drugs works better than one drug alone.
Immunosuppressant drugs include:
- Azathioprine (Azasan, Imuran) and mercaptopurine (Purinethol, Purixan). These are the most widely used immunosuppressants for the treatment of inflammatory bowel disease. Taking them requires that you follow up closely with your doctor and have your blood checked regularly to look for side effects, including effects on the liver and pancreas.
- Cyclosporine (Gengraf, Neoral, Sandimmune). This drug is normally reserved for people who haven't responded well to other medications. Cyclosporine has the potential for serious side effects and is not for long-term use.
- Tofacitinib (Xeljanz). This is called a "small molecule" and works by stopping the process of inflammation. Tofacitinib is effective when other therapies don't work. Main side effects include the increased risk of shingles infection and blood clots.
Biologics
This class of therapies targets proteins made by the immune system. Types of biologics used to treat ulcerative colitis include:
- Infliximab (Remicade), adalimumab (Humira) and golimumab (Simponi). These drugs, called tumor necrosis factor (TNF) inhibitors, or biologics, work by neutralizing a protein produced by your immune system. They are for people with severe ulcerative colitis who don't respond to or can't tolerate other treatments.
- Vedolizumab (Entyvio). This medication is approved for treatment of ulcerative colitis for people who don't respond to or can't tolerate other treatments. It works by blocking inflammatory cells from getting to the site of inflammation.
- Ustekinumab (Stelara). This medication is approved for treatment of ulcerative colitis for people who don't respond to or can't tolerate other treatments. It works by blocking a different protein that causes inflammation.
Other medications
You may need additional medications to manage specific symptoms of ulcerative colitis. Always talk with your doctor before using over-the-counter medications. He or she may recommend one or more of the following.
- Anti-diarrheal medications. For severe diarrhea, loperamide (Imodium A-D) may be effective. Use anti-diarrheal medications with great caution and after talking with your doctor, because they may increase the risk of enlarged colon (toxic megacolon).
- Pain relievers. For mild pain, your doctor may recommend acetaminophen (Tylenol, others) — but not ibuprofen (Advil, Motrin IB, others), naproxen sodium (Aleve) and diclofenac sodium, which can worsen symptoms and increase the severity of disease.
- Antispasmodics. Sometimes doctors will prescribe antispasmodic therapies to help with cramps.
- Iron supplements. If you have chronic intestinal bleeding, you may develop iron deficiency anemia and be given iron supplements.
Surgery
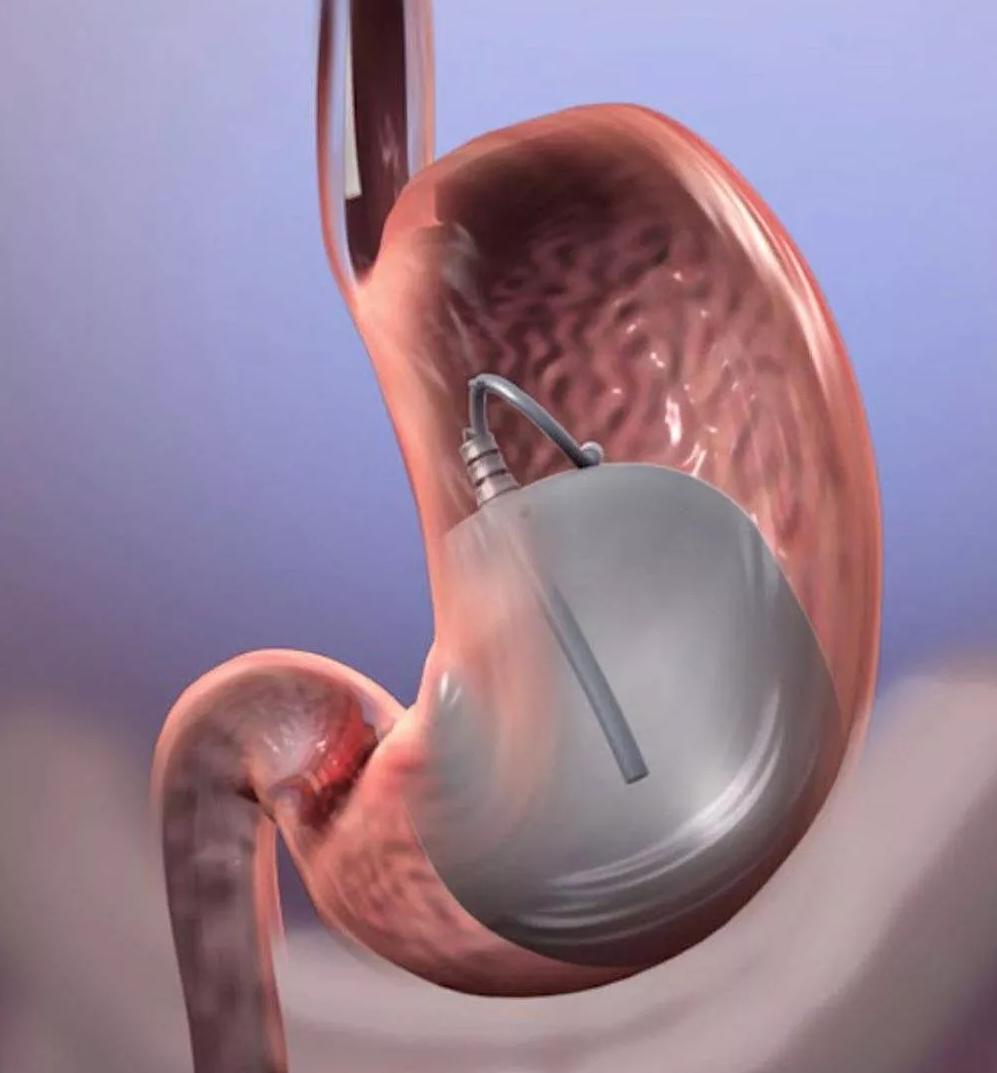
Surgery can eliminate ulcerative colitis and involves removing your entire colon and rectum (proctocolectomy).
In most cases, this involves a procedure called ileoanal anastomosis (J-pouch) surgery. This procedure eliminates the need to wear a bag to collect stool. Your surgeon constructs a pouch from the end of your small intestine. The pouch is then attached directly to your anus, allowing you to expel waste relatively normally.
In some cases a pouch is not possible. Instead, surgeons create a permanent opening in your abdomen (ileal stoma) through which stool is passed for collection in an attached bag.
Cancer surveillance
You will need more-frequent screening for colon cancer because of your increased risk. The recommended schedule will depend on the location of your disease and how long you have had it. People with proctitis are not at increased risk of colon cancer.
If your disease involves more than your rectum, you will require a surveillance colonoscopy every one to two years, beginning as soon as eight years after diagnosis if the majority of your colon is involved, or 15 years if only the left side of your colon is involved.
Prevention
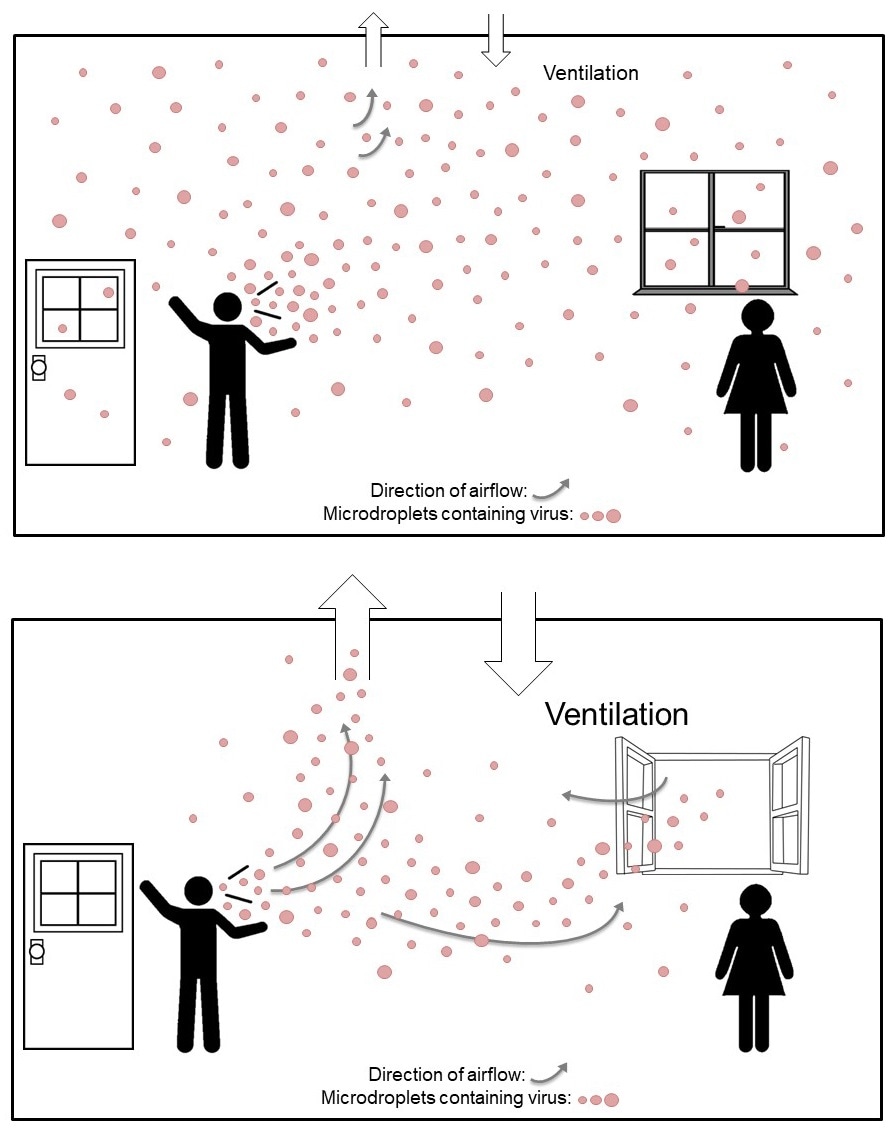
When you’re in remission from ulcerative colitis, you’ll want to do everything you can to prevent a flare-up. Things that may cause a flare-up include:
- Emotional stress: Get at least seven hours of sleep a night, exercise regularly and find healthy ways to relieve stress, such as meditation.
- NSAID use: For pain relief or a fever, use acetaminophen (Tylenol®) instead of NSAIDs like Motrin® and Advil®.
- Antibiotics: Let your healthcare provider know if antibiotics trigger your symptoms.
What role does diet and nutrition play in ulcerative colitis?
Diet does not cause the development of ulcerative colitis nor can any special diet cure the disease. However, the foods you or your child eat may play a role in managing symptoms and lengthening the time between flare-ups.
Some foods may make symptoms worse and should be avoided, especially during flare-ups. Foods that trigger symptoms are different from person to person. To narrow down what foods affect you, keep track of what you eat each day and how you feel afterward (a food journal).
Problem foods often include:
- Greasy foods.
- High sugar foods and drinks.
- Carbonated beverages.
- High-fiber foods.
- Alcohol.
In addition to the problem foods listed above, infants, children and teenagers can also experience issues with:
- Salt.
- Dairy products.
Keep a careful eye on your child’s diet and nutrition. Their appetite may decrease during a flare-up and they might not eat enough to stay healthy, and grow. Also, the inflammation caused by ulcerative colitis may keep their digestive tract from absorbing enough nutrients. This can also affect your child’s health. For these reasons, you may have to increase the amount of calories your child consumes.
It’s best to work with your provider and nutritionist to come up with a personalized diet plan if you or your child has ulcerative colitis.