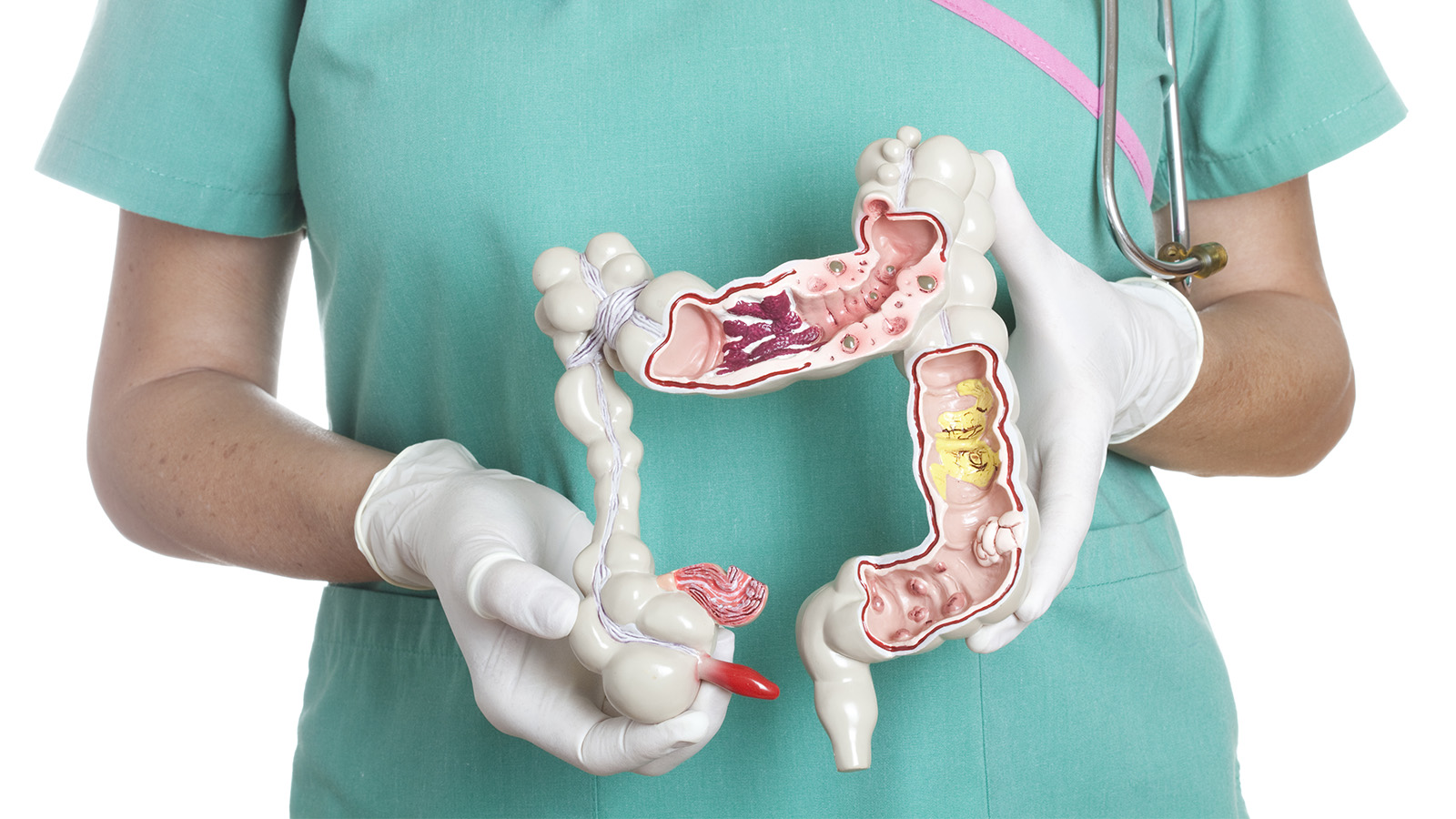
Colitis
OVERVIEW | CAUSES | RISK FACTORS | SYMPTOMS | COMPLICATION | Diagnosis | TREATMENT | PREVENTION | REFERENCES

Overview
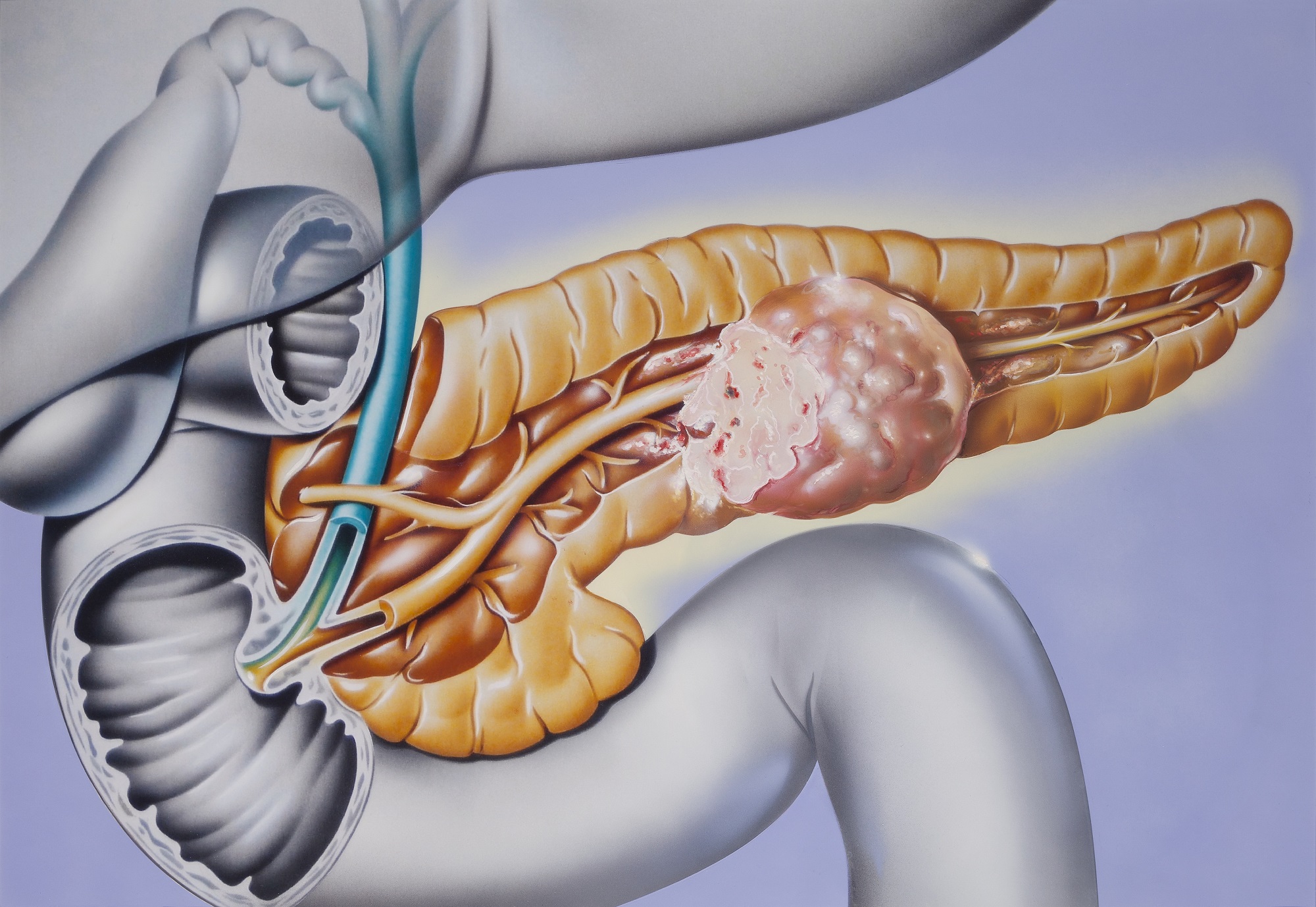
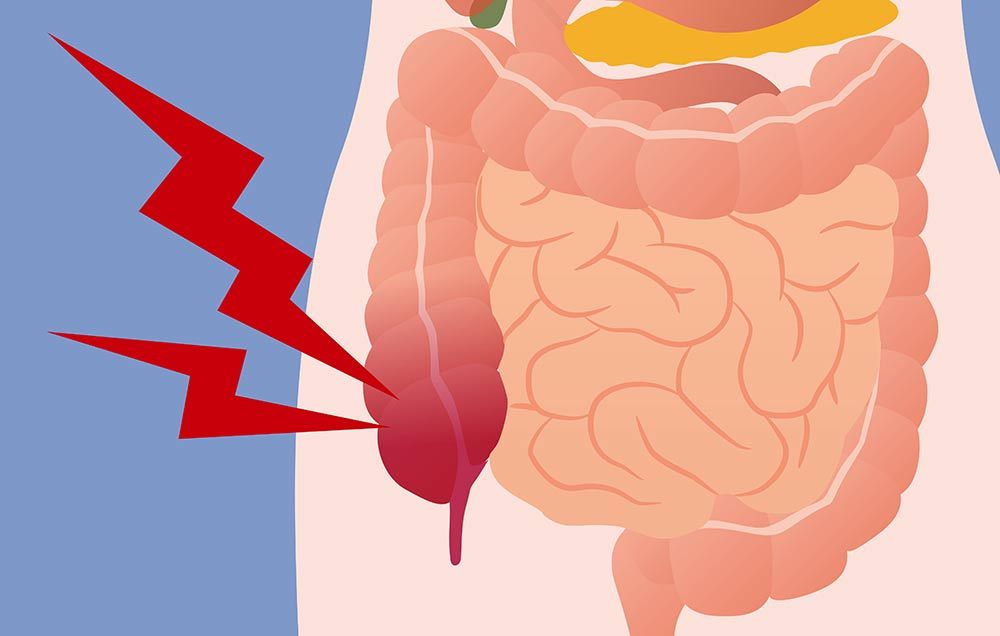
Colitis is inflammation of your colon, also known as your large intestine. If you have colitis, you’ll feel discomfort and pain in your abdomen that may be mild and reoccurring over a long period of time, or severe and appearing suddenly.
There are different types of colitis, and treatment varies depending on what type you have.
Causes
Depending upon the cause, colitis is categorized under different types:
Ulcerative colitis
Ulcerative colitis (UC) is one of two conditions classified as inflammatory bowel disease. The other is Crohn’s disease.
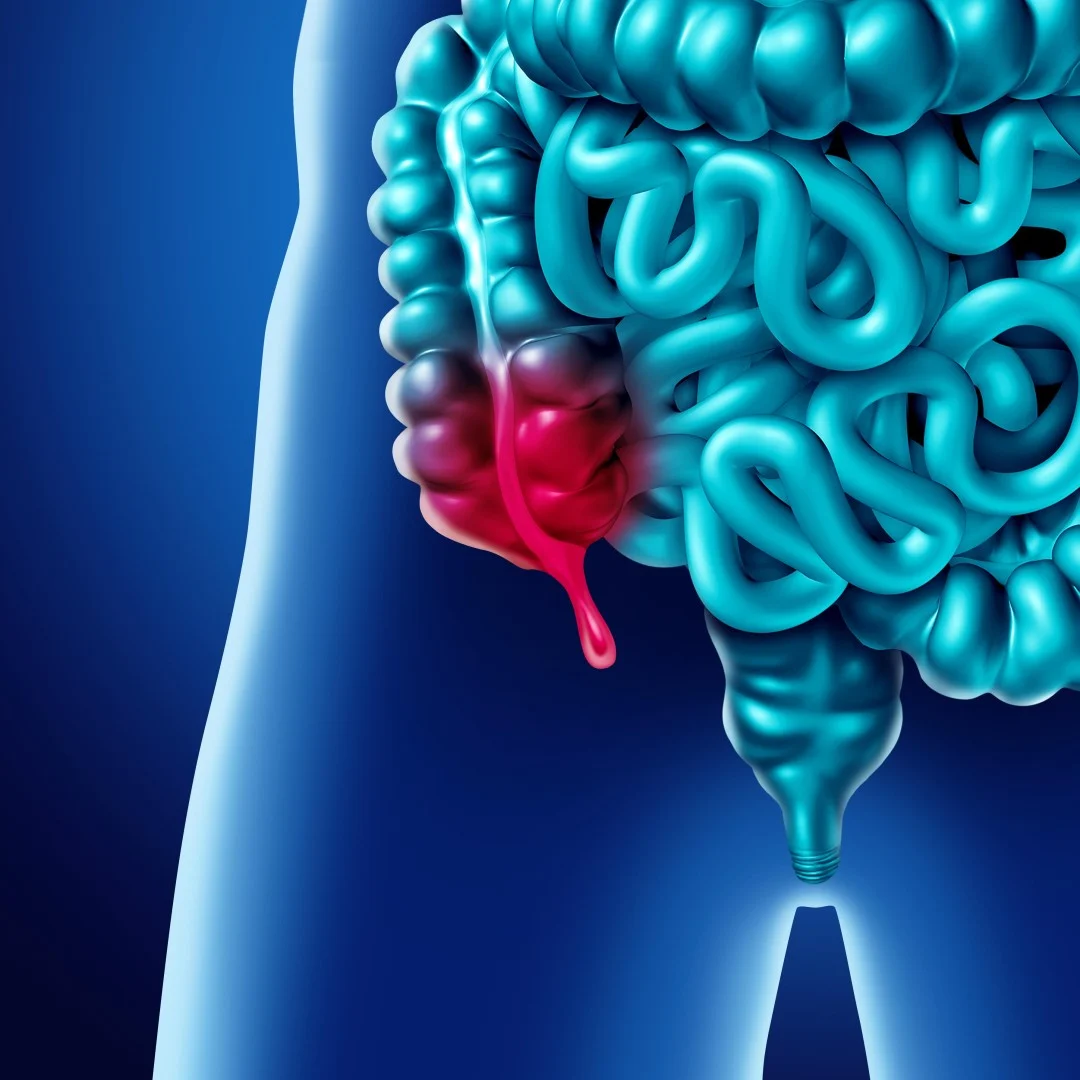
UC is a lifelong disease that produces inflammation and bleeding ulcers within the inner lining of your large intestine. It generally begins in the rectum and spreads to the colon.
UC is the most commonly diagnosed type of colitis. It occurs when the immune system overreacts to bacteria and other substances in the digestive tract, but experts don’t know why this happens. Common types of UC include:
- Proctosigmoiditis, which affects the rectum and lower portion of the colon
- Left-sided colitis, which affects the left side of the colon beginning at the rectum
- Pancolitis, which affects the entire large intestine
Pseudomembranous colitis
Pseudomembranous colitis (PC) occurs from overgrowth of the bacterium Clostridium difficile. This kind of bacteria normally lives in the intestine, but it doesn’t cause problems because it’s balanced by the presence of “good” bacteria.
Certain medications, especially antibiotics, may destroy healthy bacteria. This allows Clostridium difficile to take over, releasing toxins that cause inflammation.
Ischemic colitis
Ischemic colitis (IC) occurs when blood flow to the colon is suddenly cut off or restricted. Blood clots can be a reason for sudden blockage. Atherosclerosis, or buildup of fatty deposits, in the blood vessels that supply the colon is usually the reason for recurrent IC.
This type of colitis is often the result of underlying conditions. These may include:
- Vasculitis, an inflammatory disease of the blood vessels
- Diabetes
- Colon cancer
- Dehydration
- Blood loss
- Heart failure
- Obstruction
- Trauma
Although it’s rare, IC may occur as a side effect of taking certain medications.
Microscopic colitis
Microscopic colitis is a medical condition a doctor can only identify by looking at a tissue sample of the colon under a microscope. A doctor will view signs of inflammation, such as lymphocytes, which are a kind of white blood cell.
Doctors sometimes classify microscopic colitis into two categories: lymphocytic and collagenous colitis. Lymphocytic colitis is when a doctor identifies a significant number of lymphocytes. However, the colon tissues and lining are not abnormally thickened.
Collagenous colitis occurs when the colon’s lining becomes thicker than usual due to a buildup of collagen under the outermost layer of tissue. Different theories exist about each microscopic colitis type, but some doctors theorize that both colitis types are different forms of the same condition.
Doctors don’t know exactly what causes microscopic colitis. However, they do know some people are more at risk for the condition. These include:
- Current smokers
- Female gender
- History of an autoimmune disorder
- Older than age 50
The most common symptoms of microscopic colitis are chronic watery diarrhea, abdominal bloating, and abdominal pain.
Allergic colitis in infants
Allergic colitis is a condition that can occur in infants, usually within the first two months after birth. The condition can cause symptoms in infants that include reflux, excessive spitting up, fussiness, and possible flecks of blood in a baby’s stool.
Doctors don’t know exactly what causes allergic colitis. According to a 2013 study published in the World Journal of Gastroenterology, one of the most popular theories is that infants have an allergic or hypersensitive reaction to certain components in breast milk.
Doctors will often recommend an elimination diet for mom where she slowly stops eating certain foods known to contribute to allergic colitis. Examples include cow’s milk, eggs, and wheat. If the baby stops having symptoms, these foods were likely the culprit.
Additional causes
Other causes of colitis include infection from parasites, viruses, and food poisoning from bacteria. You may also develop the condition if your large intestine has been treated with radiation.
Risk factors
Different risk factors are associated with each type of colitis.
You’re more at risk for UC if you:
- Are between the ages of 15 and 30 (most common) or 60 and 80
- Are of Jewish or Caucasian descent
- Have a family member with UC
You’re more at risk for PC if you:
- Are taking long-term antibiotics
- Are hospitalized
- Are receiving chemotherapy
- Are taking immunosuppressant drugs
- Are older
- Have had PC before
You’re more at risk for IC if you:
- Are over age 50
- Have or are at risk for heart disease
- Have heart failure
- Have low blood pressure
- Have had an abdominal operation
Symptoms
Depending on your condition, you may experience one or more of the following symptoms:
- Abdominal pain or cramping
- Bloating in your abdomen
- Weight loss
- Diarrhea with or without blood
- Blood in your stool
- Urgent need to move your bowels
- Chills or fever
- Vomiting
Complications
Colitis is associated with complications both within the digestive system and outside the digestive system (which are called extra-intestinal symptoms).
Intestinal complications can include:
- Bowel perforation. A hole in the colon which is a medical emergency that can cause severe bleeding and abdominal pain. This complication is uncommon in people who have ulcerative colitis.
- Fissure. A fissure is a tear that occurs in the lining of the anal canal that can cause bleeding and pain but is usually treatable at home.
- Toxic megacolon. An uncommon condition that causes severe distention of the colon, toxic megacolon is a serious complication that needs emergency treatment.
- Colon cancer. After having ulcerative colitis for about 8 to 10 years, the risk of developing colon cancer increases. It's important to work with a gastroenterologist to schedule screening for colon cancer at regular intervals.
Extra-intestinal complications can include:
- Delayed growth in children. Some older medications used to treat ulcerative colitis and malnutrition caused by the disease can contribute to growth problems.12
- Eye diseases. Several eye conditions, including uveitis, glaucoma, keratopathy, episcleritis, and dry eyes, are associated with ulcerative colitis or the treatments for the disease.13
- Arthritis. The most common of the extra-intestinal manifestations, several different forms of arthritis can occur in people with ulcerative colitis, including peripheral arthritis, axial arthritis, rheumatoid arthritis, and ankylosing spondylitis.14
- Skin conditions. Erythema nodosum and pyoderma gangrenosum are uncommon conditions that occur more frequently in people who have IBD. Psoriasis, another immune-mediated condition, is also more common in people who have IBD.15
- Mouth ulcers. Also called aphthous stomatitis, these are lesions in the lining of the mouth that may occur along with an ulcerative colitis flare-up.16
- Symptoms during menstruation. Some women with IBD find that pre-menstrual syndrome (PMS) occurring in the days leading up to their period brings on more diarrhea and pain.
Diagnosis
Your doctor may ask about the frequency of your symptoms and when they first occurred. They’ll perform a thorough physical exam and use diagnostic tests such as:
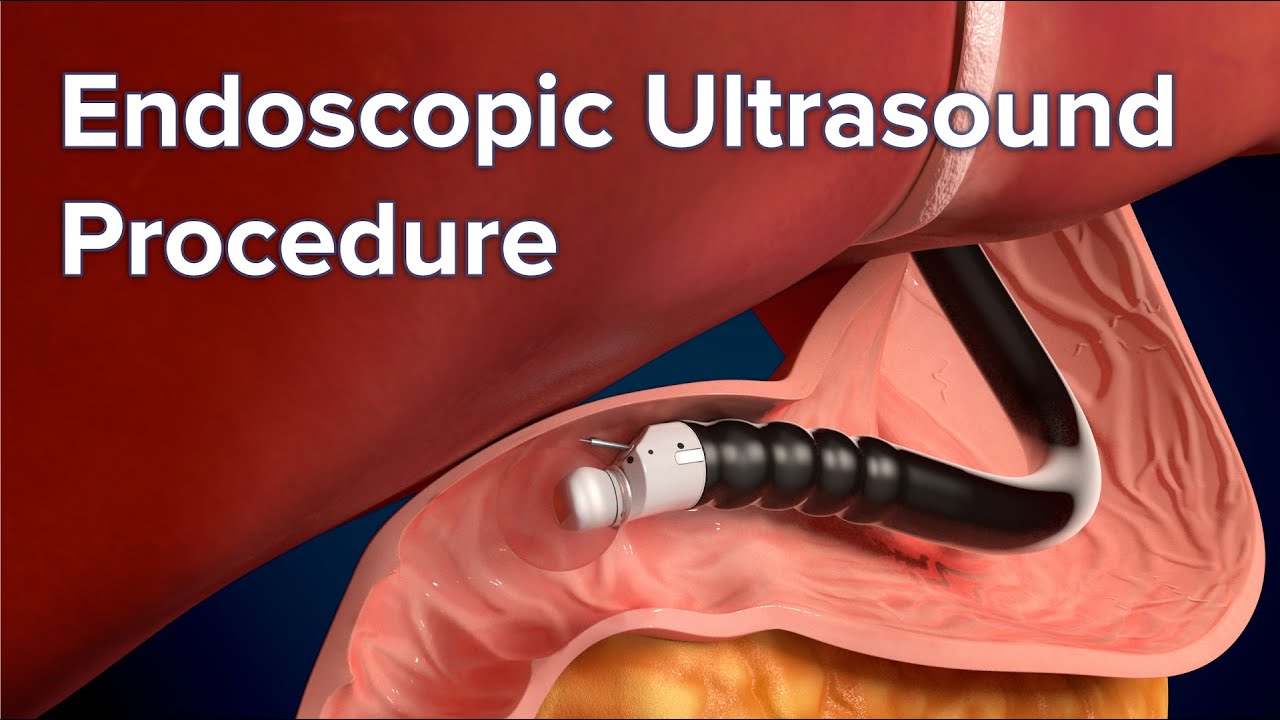
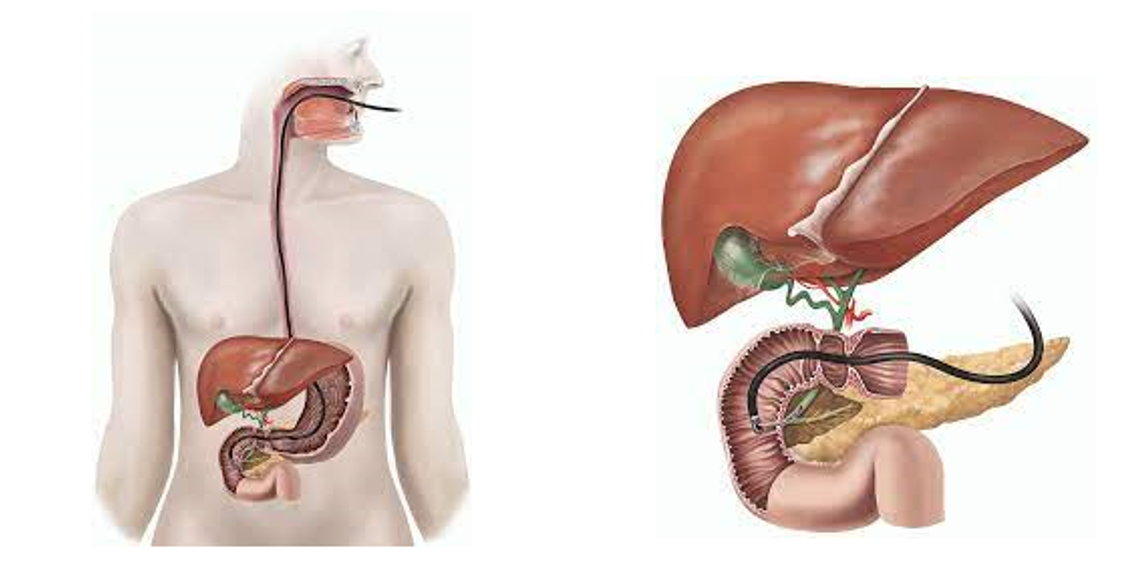
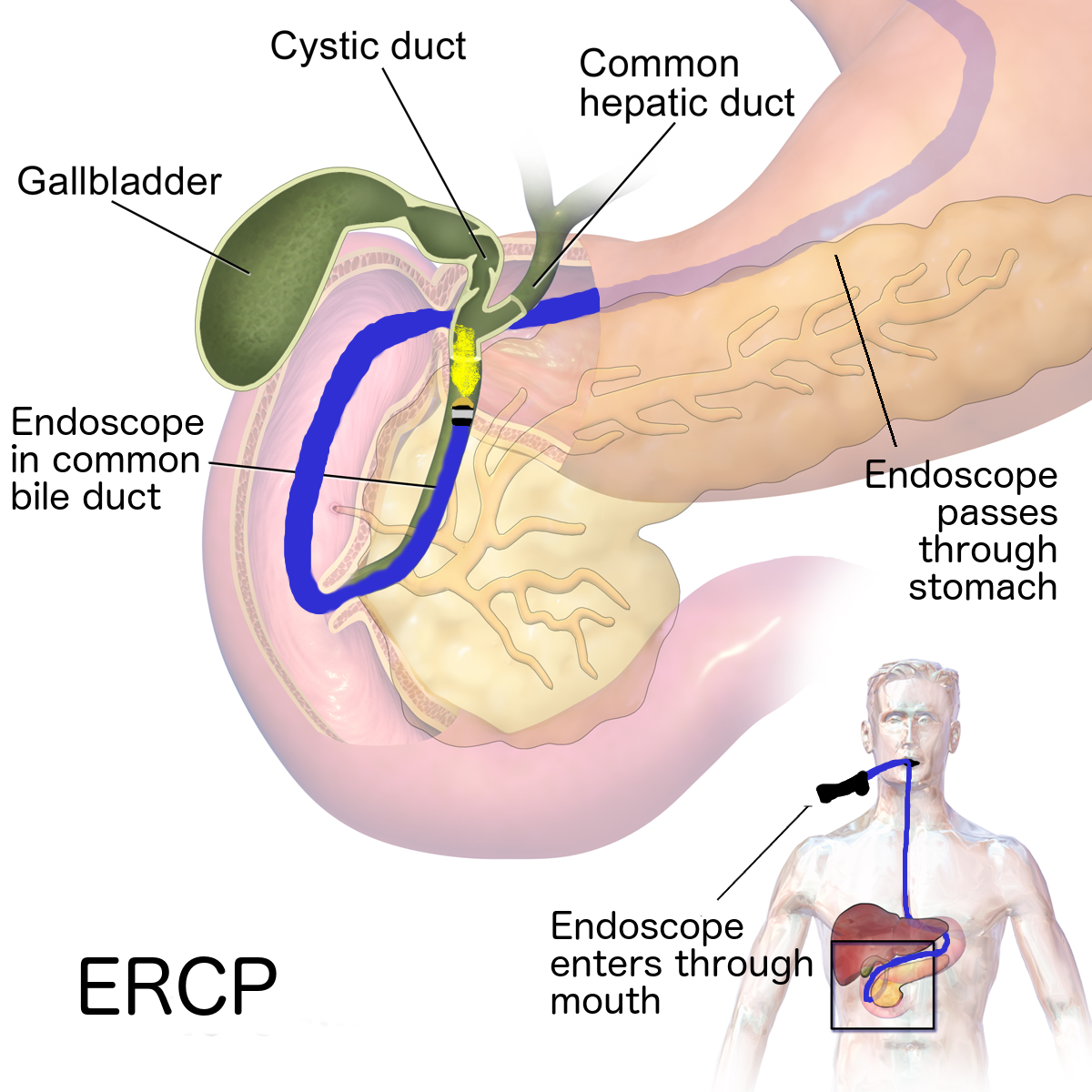
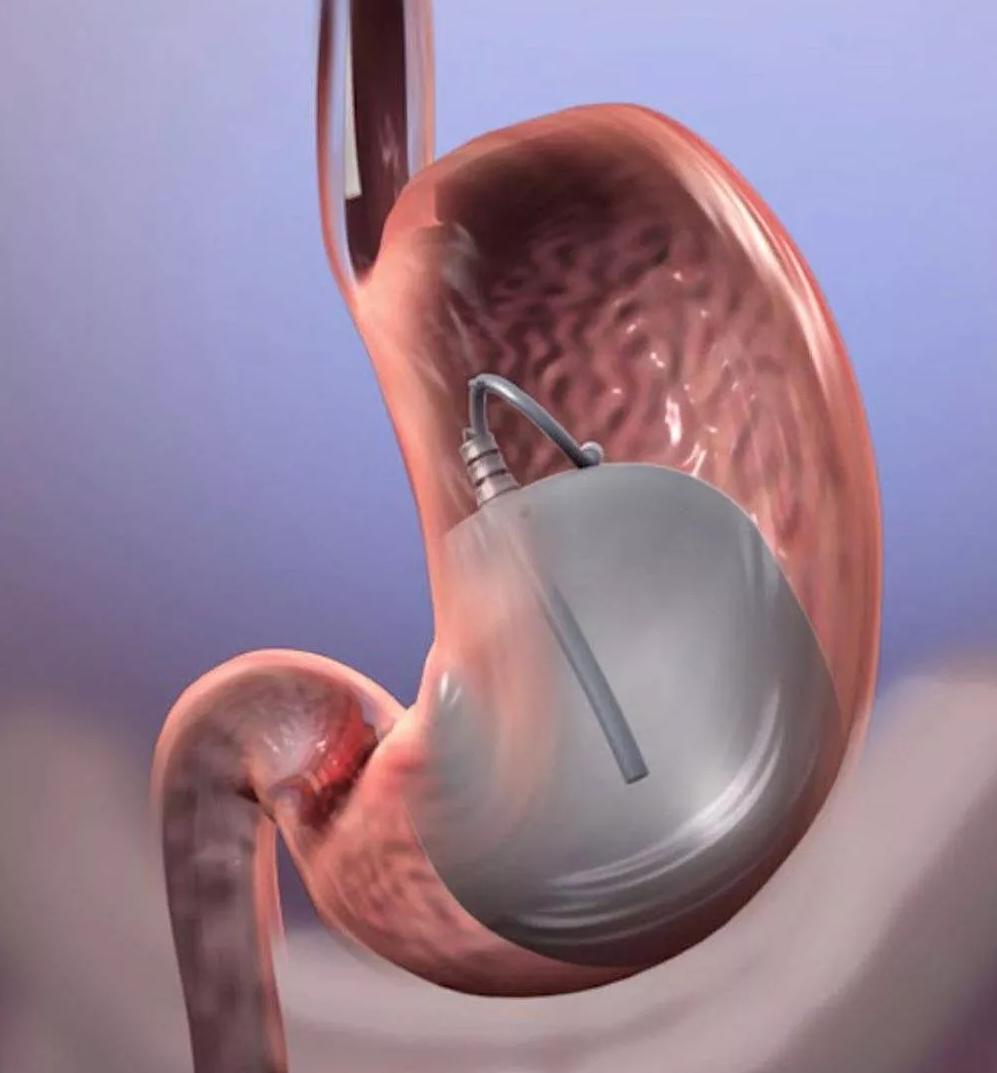
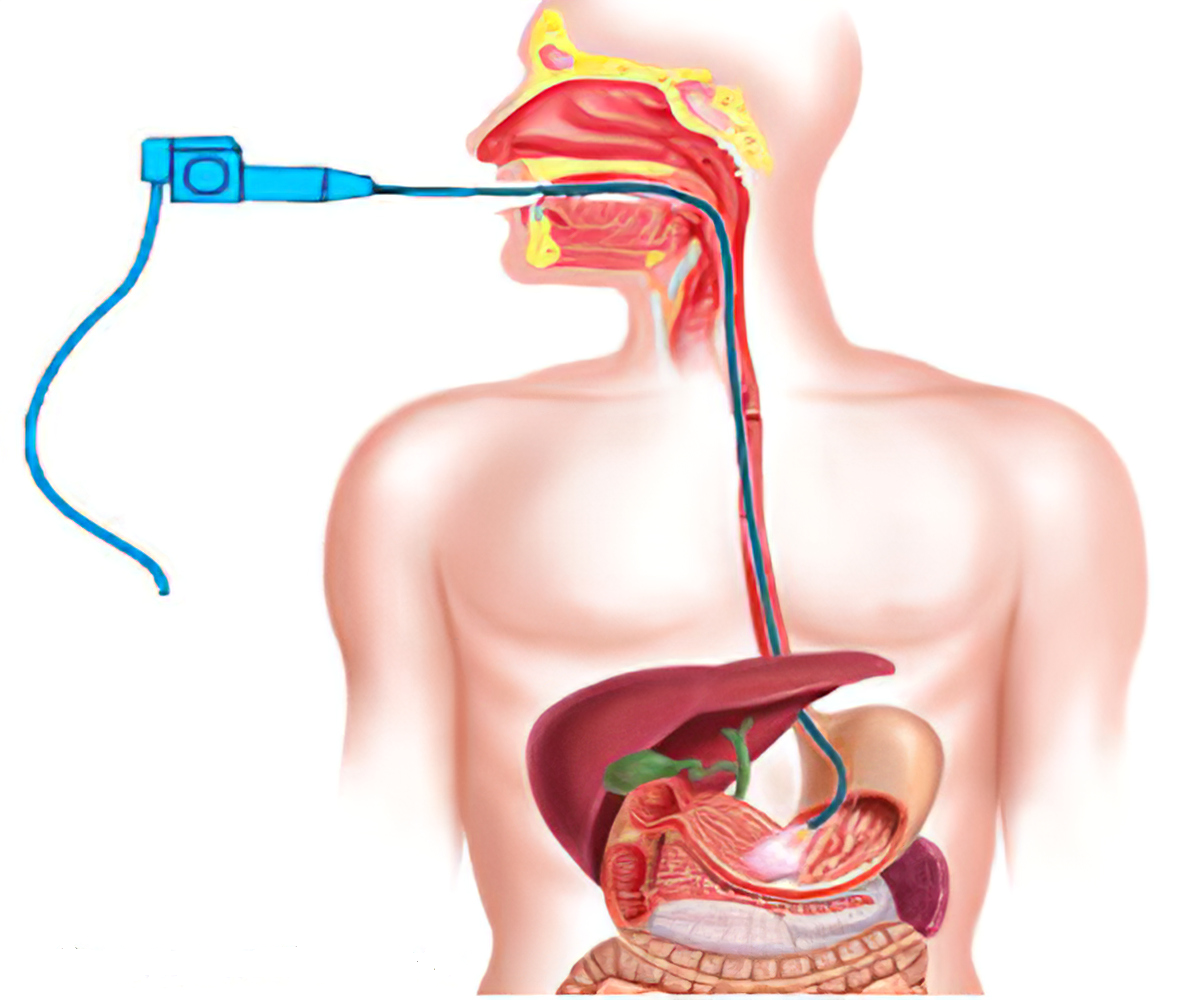
- Colonoscopy, which involves threading a camera on a flexible tube through the anus to view the rectum and colon
- Sigmoidoscopy, which is similar to a colonoscopy but shows only the rectum and lower colon
- Stool samples
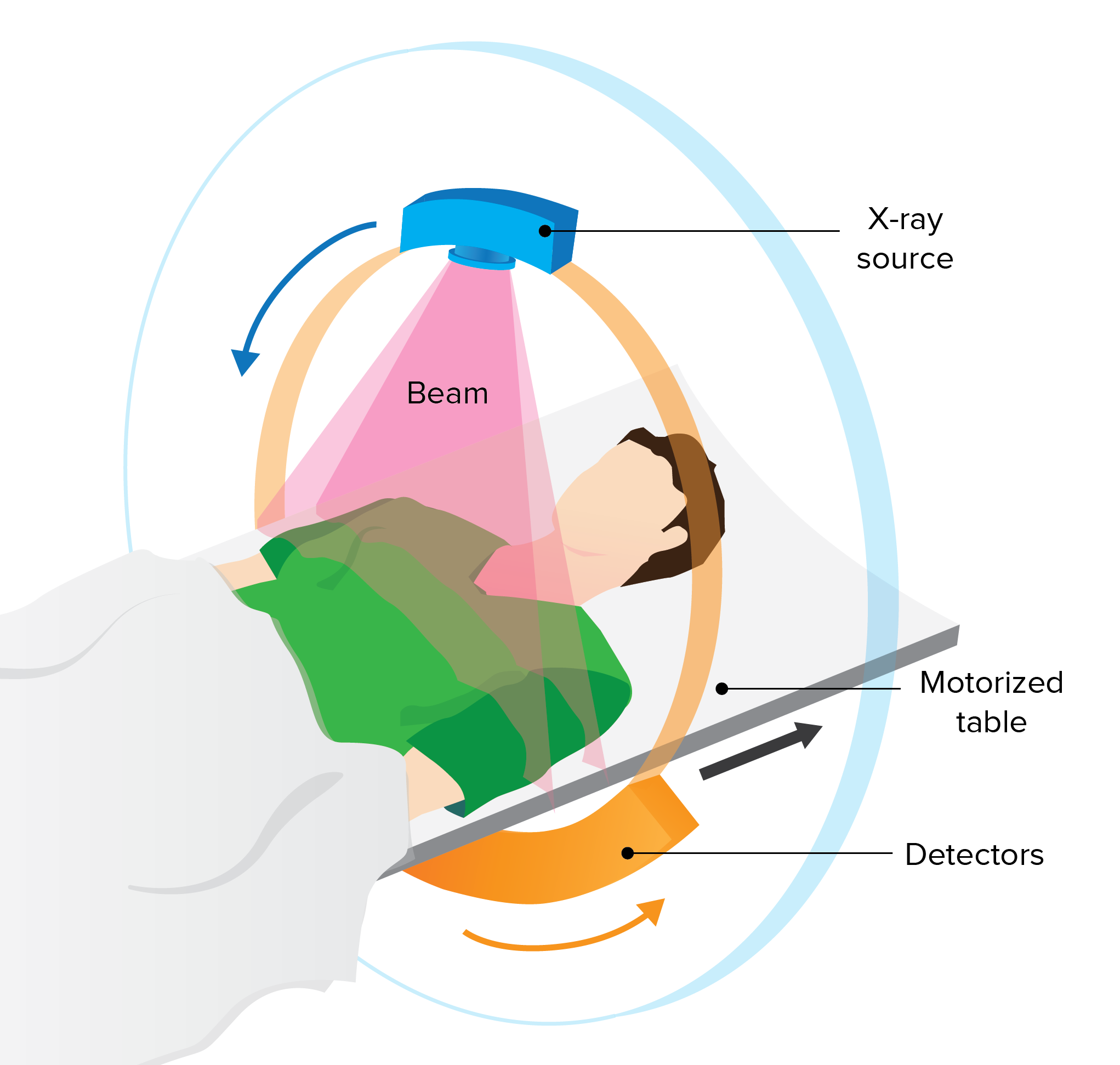
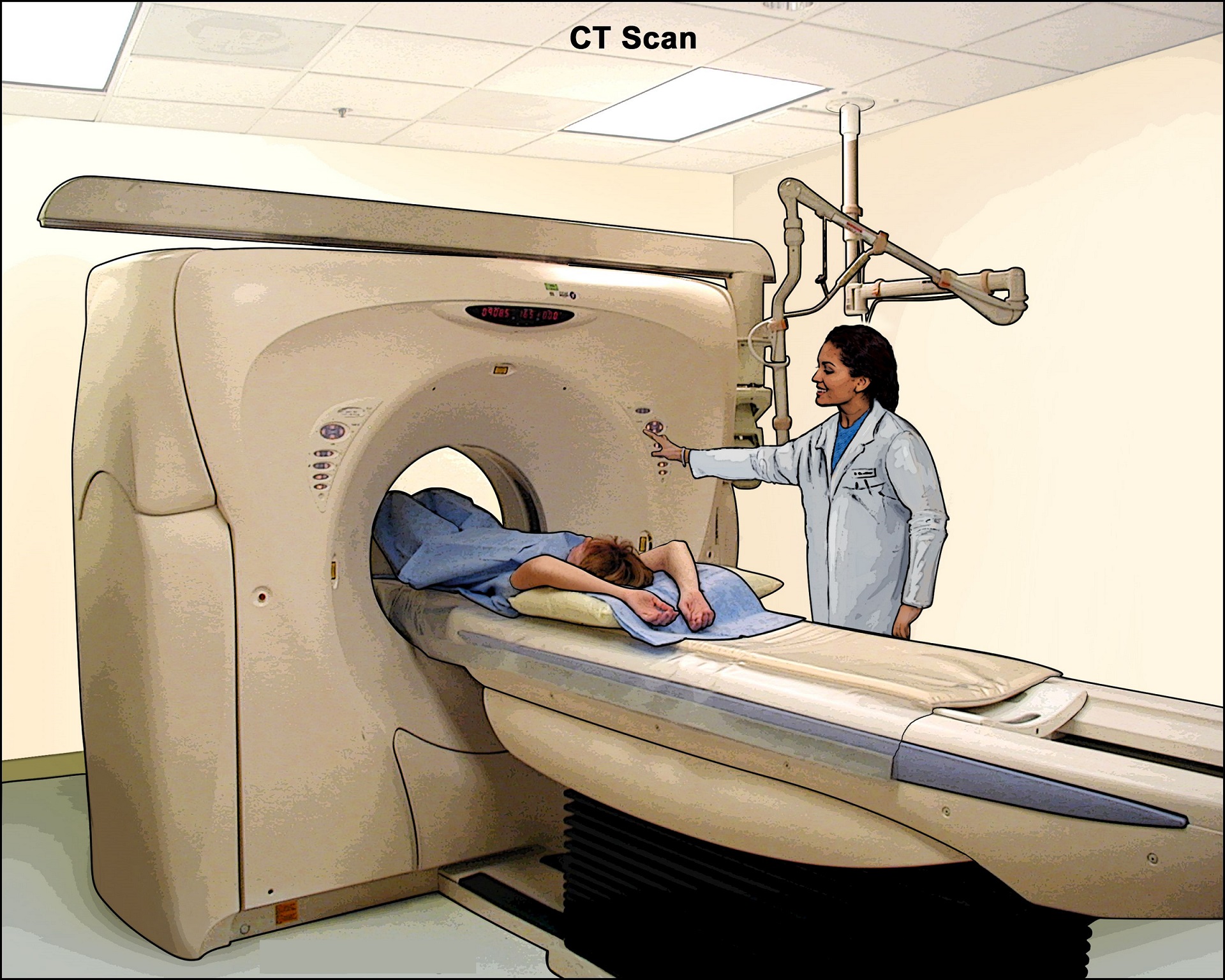
- Abdominal imaging such as MRI or CT scans
- Ultrasound, which is useful depending on the area being scanned
- Barium enema, an X-ray of the colon after it’s injected with barium, which helps make images more visible
Treatment
Treatments vary by a few factors:
- type of colitis
- age
- overall physical condition
Bowel rest
Limiting what you take in by mouth can be useful, especially if you have IC. Taking fluids and other nutrition intravenously may be necessary during this time.
Medication
Your doctor may prescribe anti-inflammatory medication to treat swelling and pain, and antibiotics to treat infection. Your doctor may also treat you with pain medications or antispasmodic drugs.
Surgery
Surgery to remove part or all of your colon or rectum may be necessary if other treatments don’t work.
Prevention
Colitis cannot be prevented and patients should see their physician regularly to develop a plan of care to help manage the symptoms and effects of their disease.