COVID-19
COVID-19 and Mucormycosis fungal infection: All you need to know
After Delhi’s Sri Ganga Ram Hospital reported cases of a rare fungal infection in Covid-19 patients, hospitals of several other cities have reported the same occurrence. This is not new but a rare infection that affects people with weakened immunity.
Summary: 60 Second Read
This article will cover-
Overview
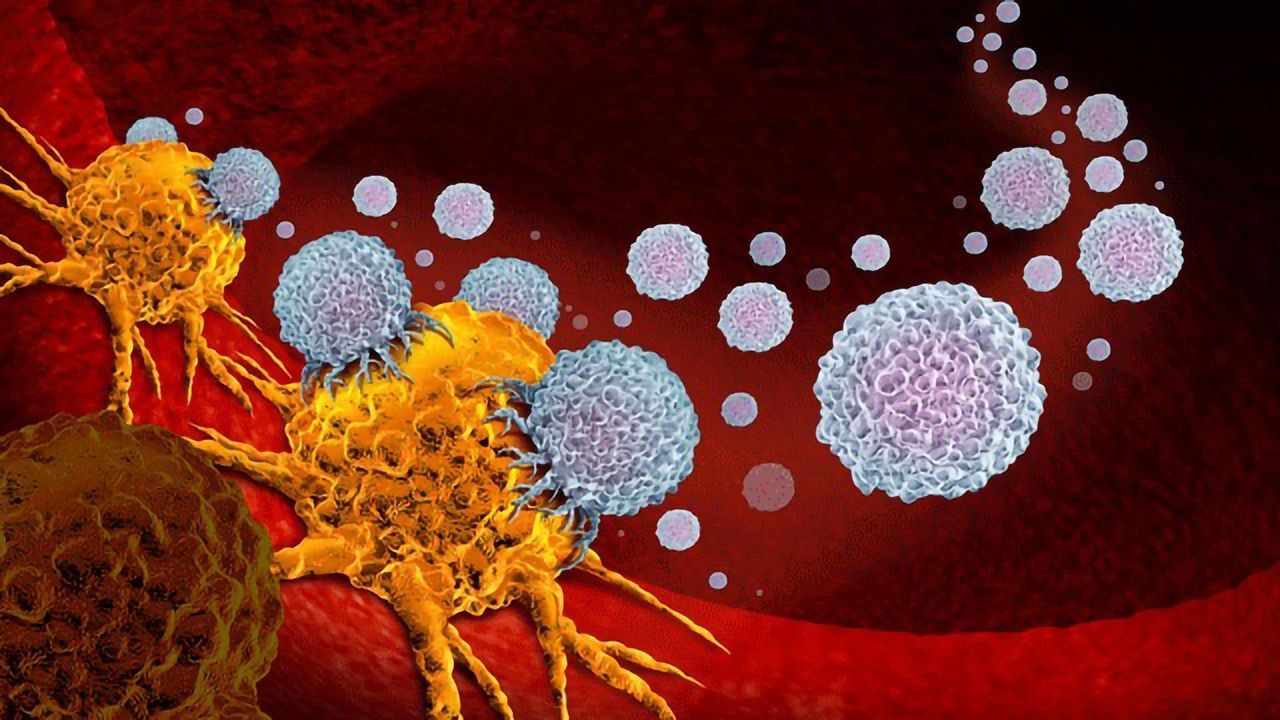
One may suffer mild to moderate respiratory issues if infected with COVID-19, but in many cases, the virus is affecting a patient’s overall well-being and aggravating other severe diseases, if any, as well. After months of research, it is now known that apart from attacking the respiratory tract, COVID also affects blood vessels and the body’s defense mechanism drastically.
But as of late, a number of hospitals have reported Mucormycosis in COVID-recovered patients.
What is Mucormycosis?
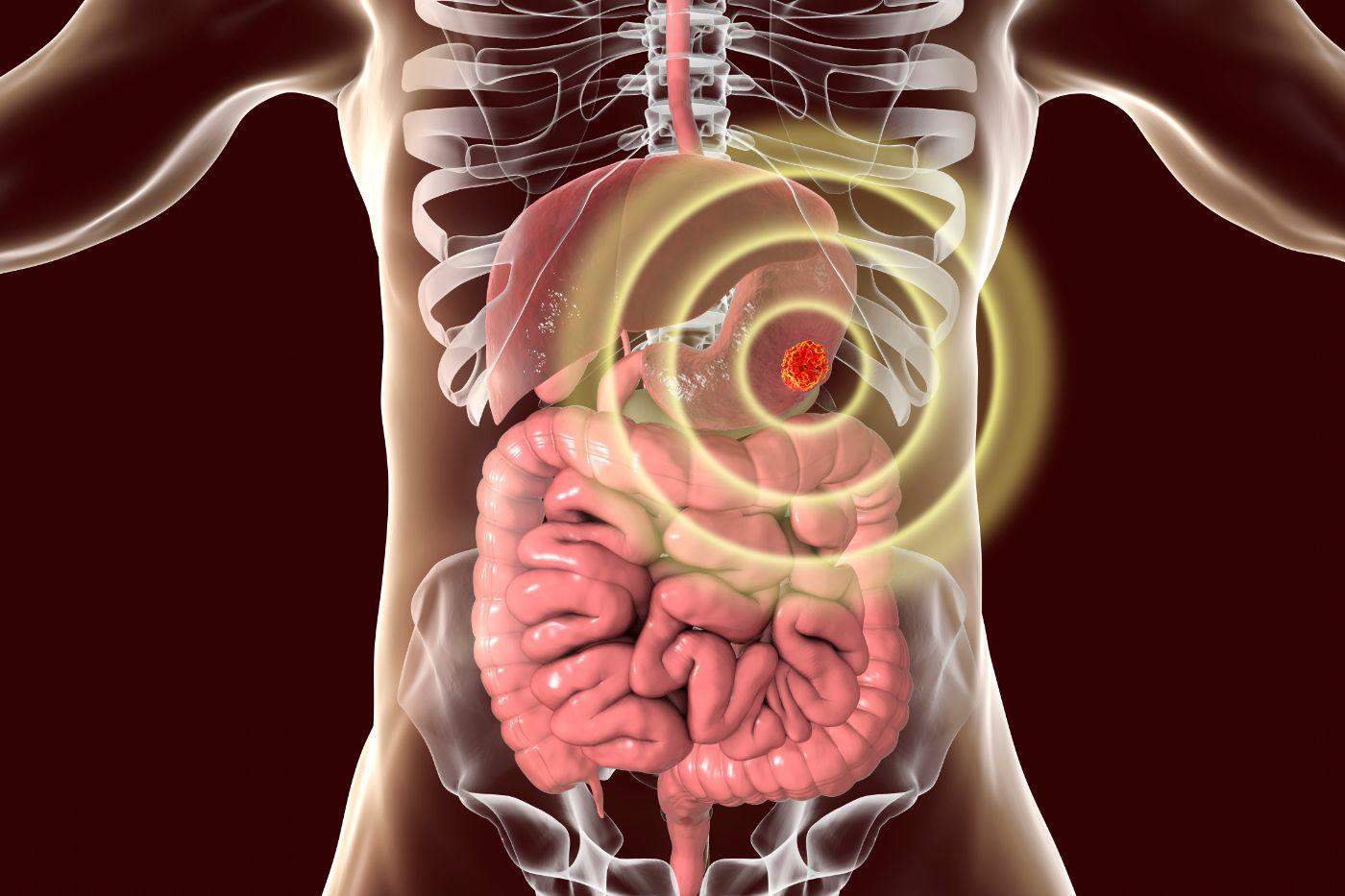
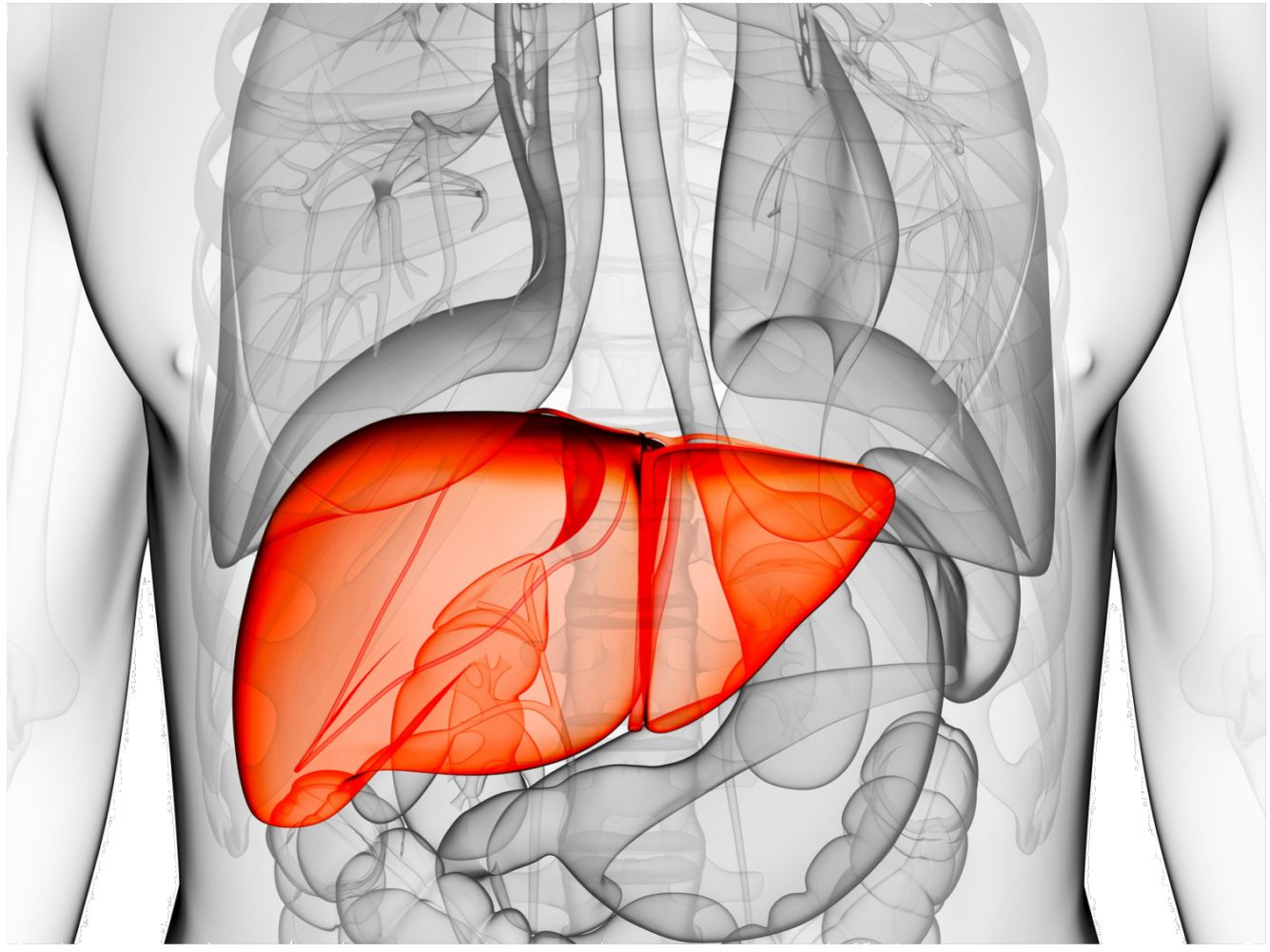
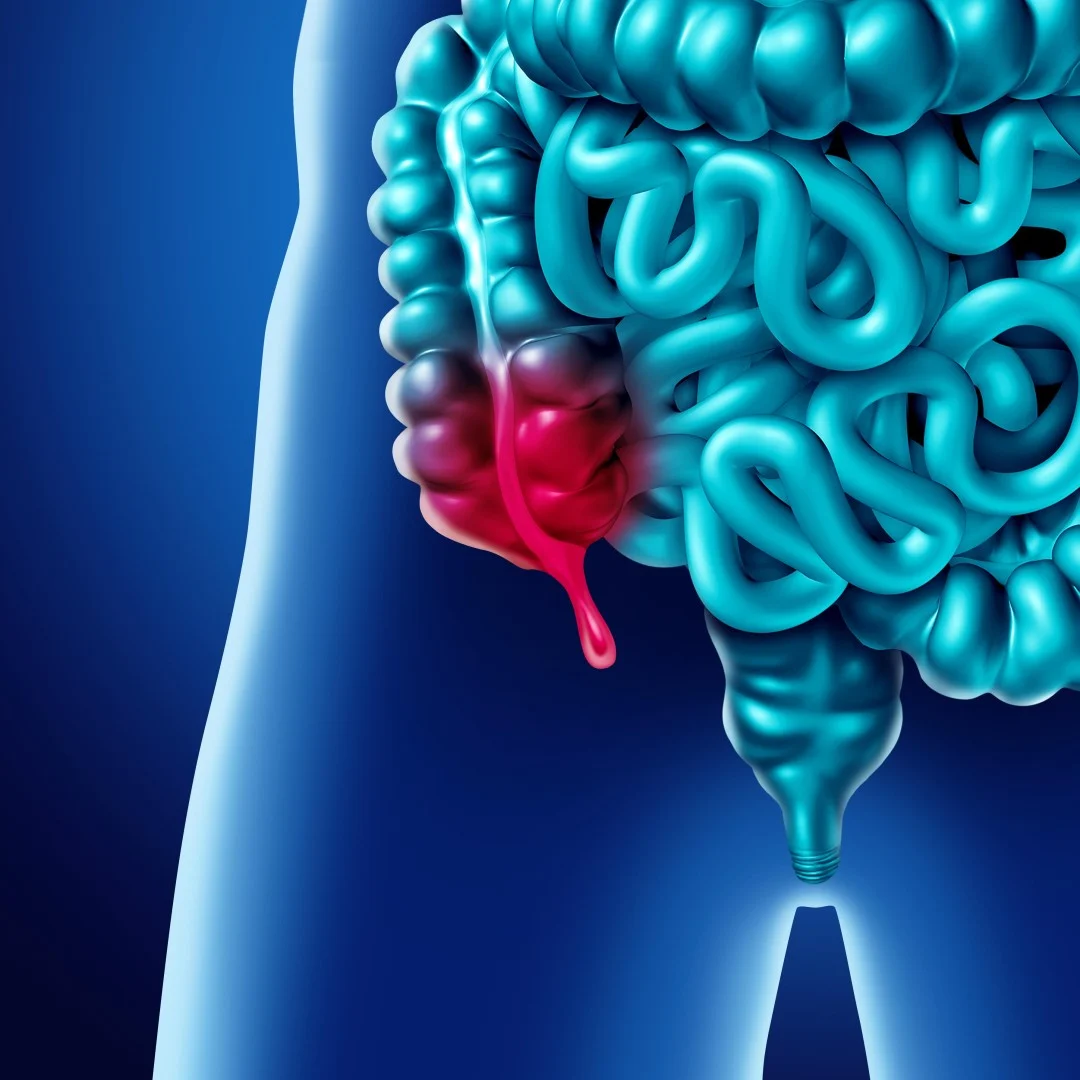
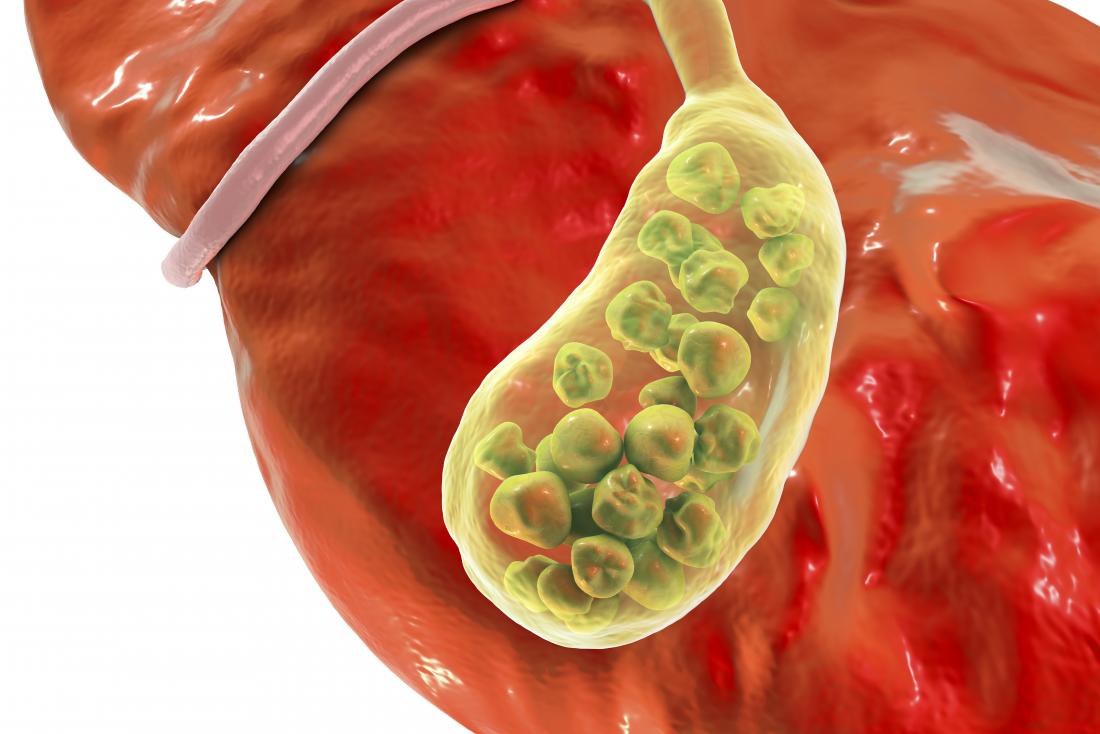
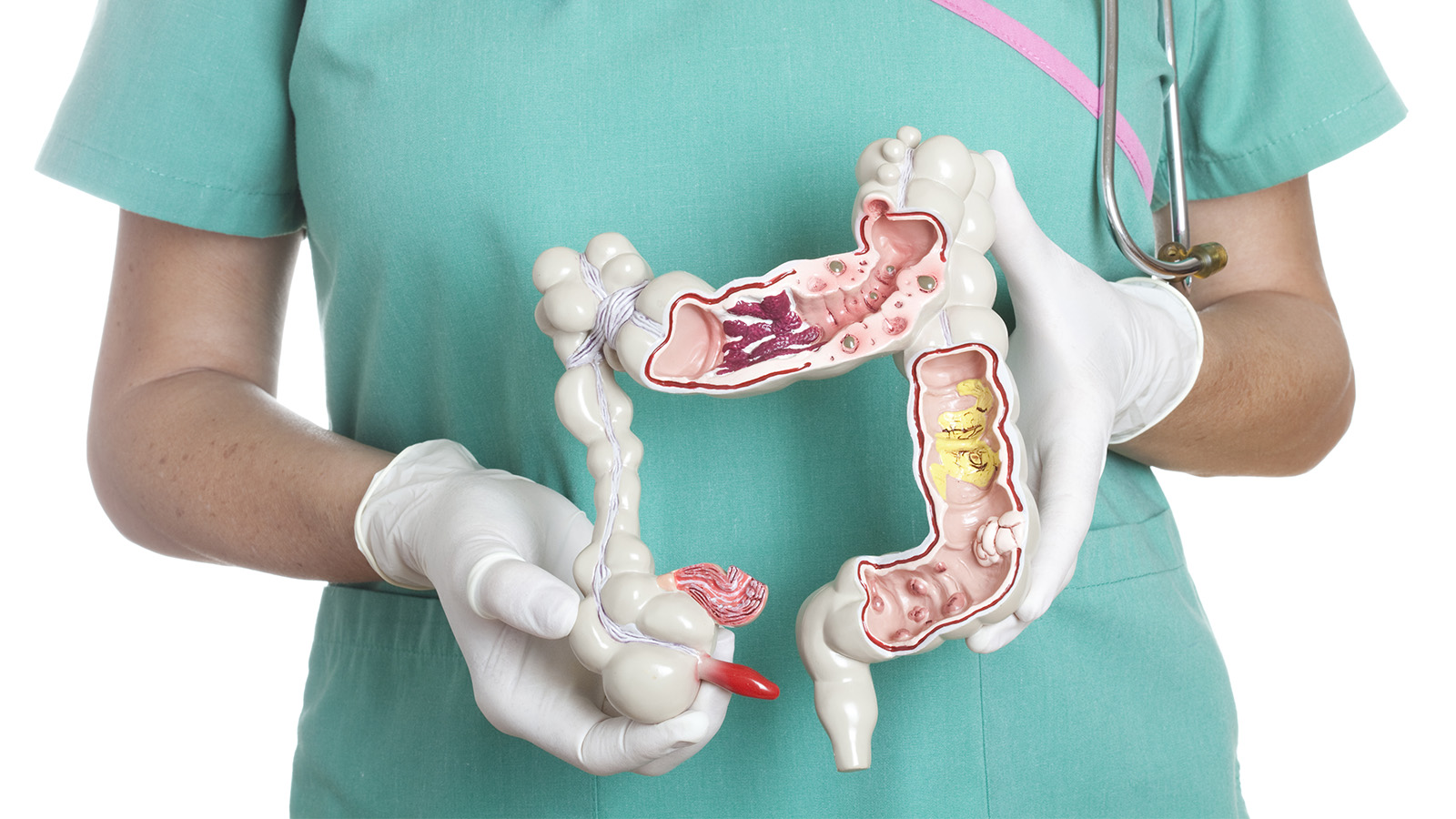
Mucormycosis is a fungal infection which starts in the nasal area, throat, and then soon spreads to the eyes, brain, and finally, the entire body. Once it starts infecting a patient’s brain, it becomes life-threatening. Its rapid spread worsens the condition which can lead to multiple organ failure as well if left untreated or not treated at the right time. In the process, it damages immunity, aggravates other diseases, and makes the patient infection-prone.
Here is all you need to know about it:
- It can occur in almost any part of the body. It can affect the sinuses or the lungs if the fungus enters through inhaling. It can also enter the skin through a cut, burn or any other type of skin injury.
- If not detected early, the infection – Mucormycosis also known as black fungus – can lead to loss of vision or jaw.
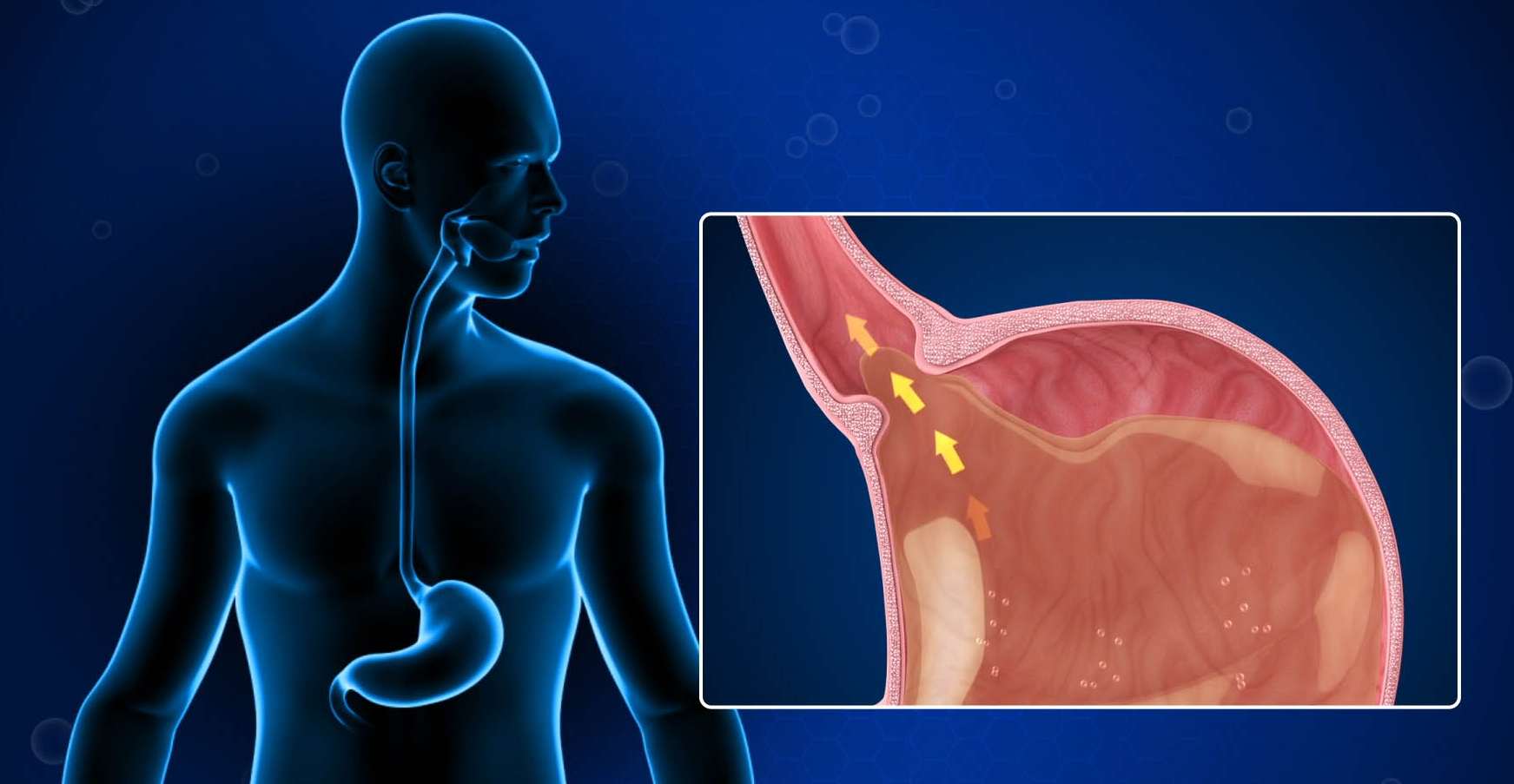
- How does it affect the eyesight? It enters through the nose and then spreads to the eyes, paralyses the muscles around the pupils which might lead to blindness. It may also cause meningitis if it spreads to the brain.
- This is not contagious.
- The connection between Covid-19 and Mucormycosis is the weakened immunity response.
Symptoms
Continuous headache, heaviness in the facial area, or swelling can be called initial minor symptoms. Visible symptoms may include badly swollen eyes, black spots around the swollen area, choked throat etc. It is recommended to seek the advice of a medical practitioner even if mild symptoms start showing.
Common symptoms are:
- One-sided facial swelling, headache, nasal or sinus congestion, black lesions on nasal bridge or upper inside of mouth, fever are symptoms of mucormycosis in sinus and brain.
- Fever, cough, chest pain, shortness of breath are the symptoms of mucormycosis in the lungs.
Skin mucormycosis has symptoms like blisters or ulcers, blackening of a portion of skin or excessive redness, swelling around a wound etc.
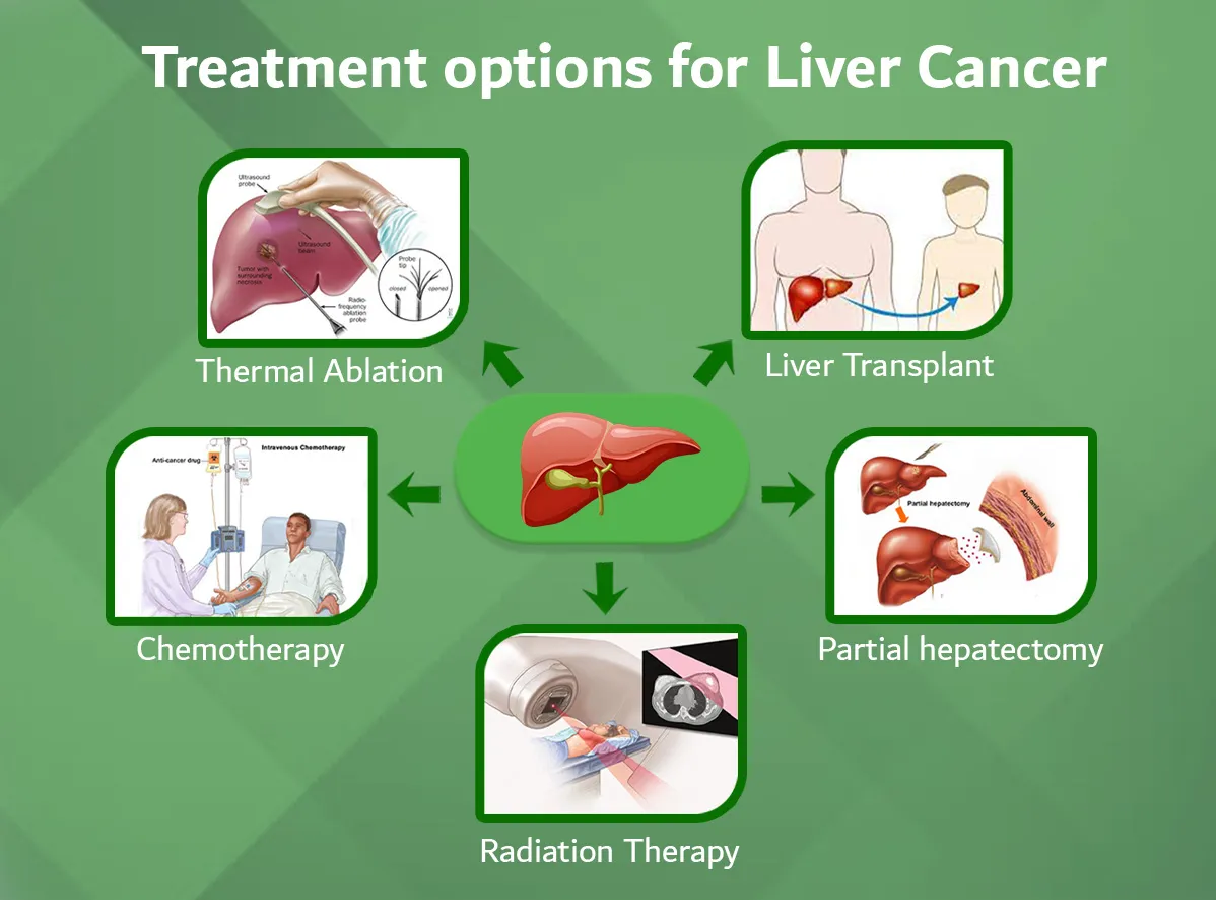
Treatment
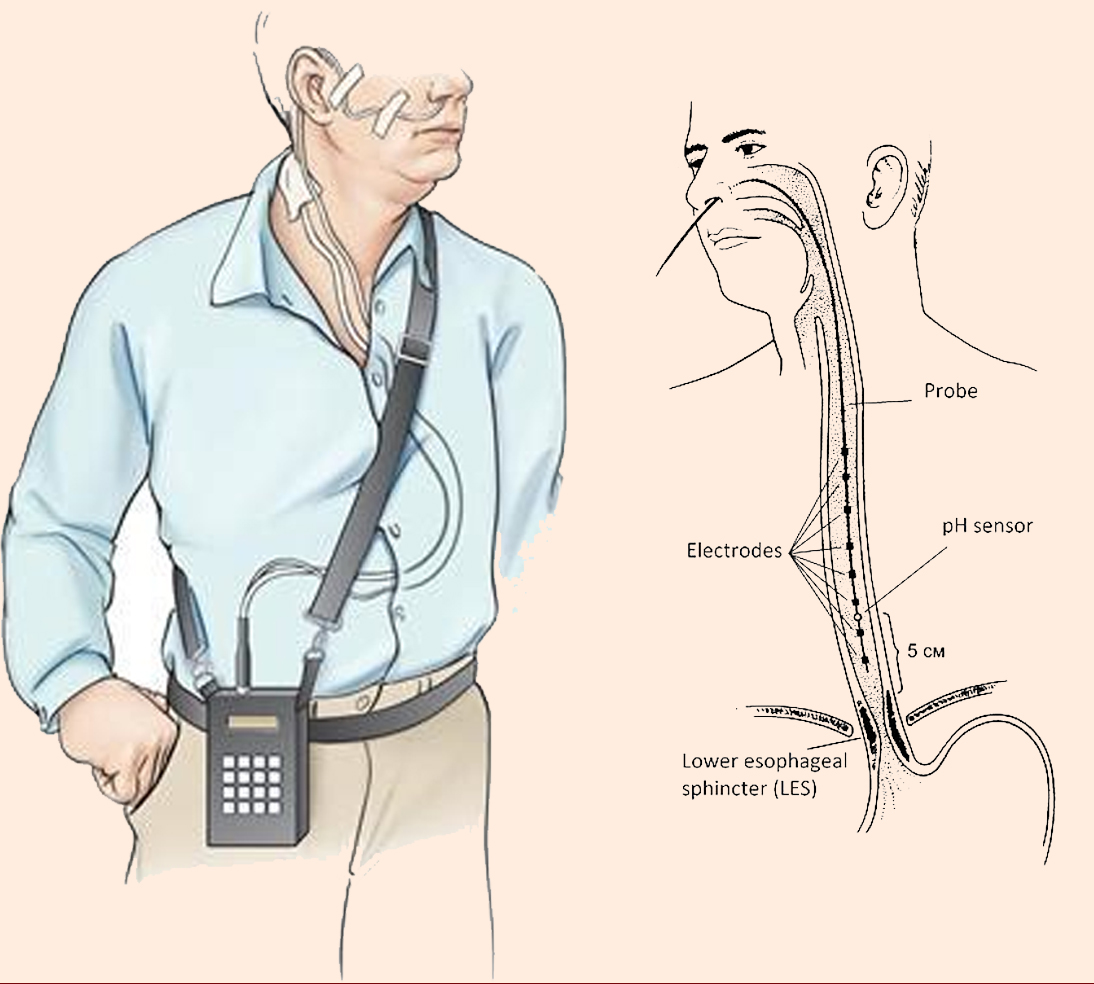
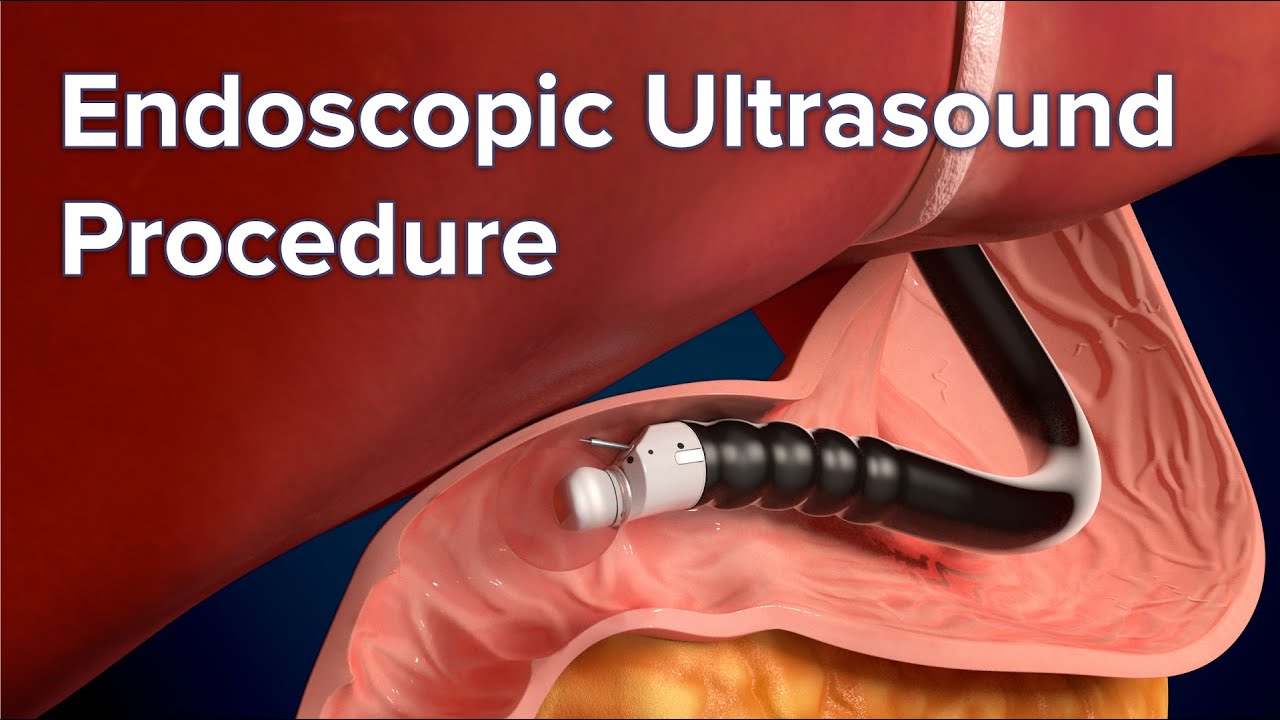
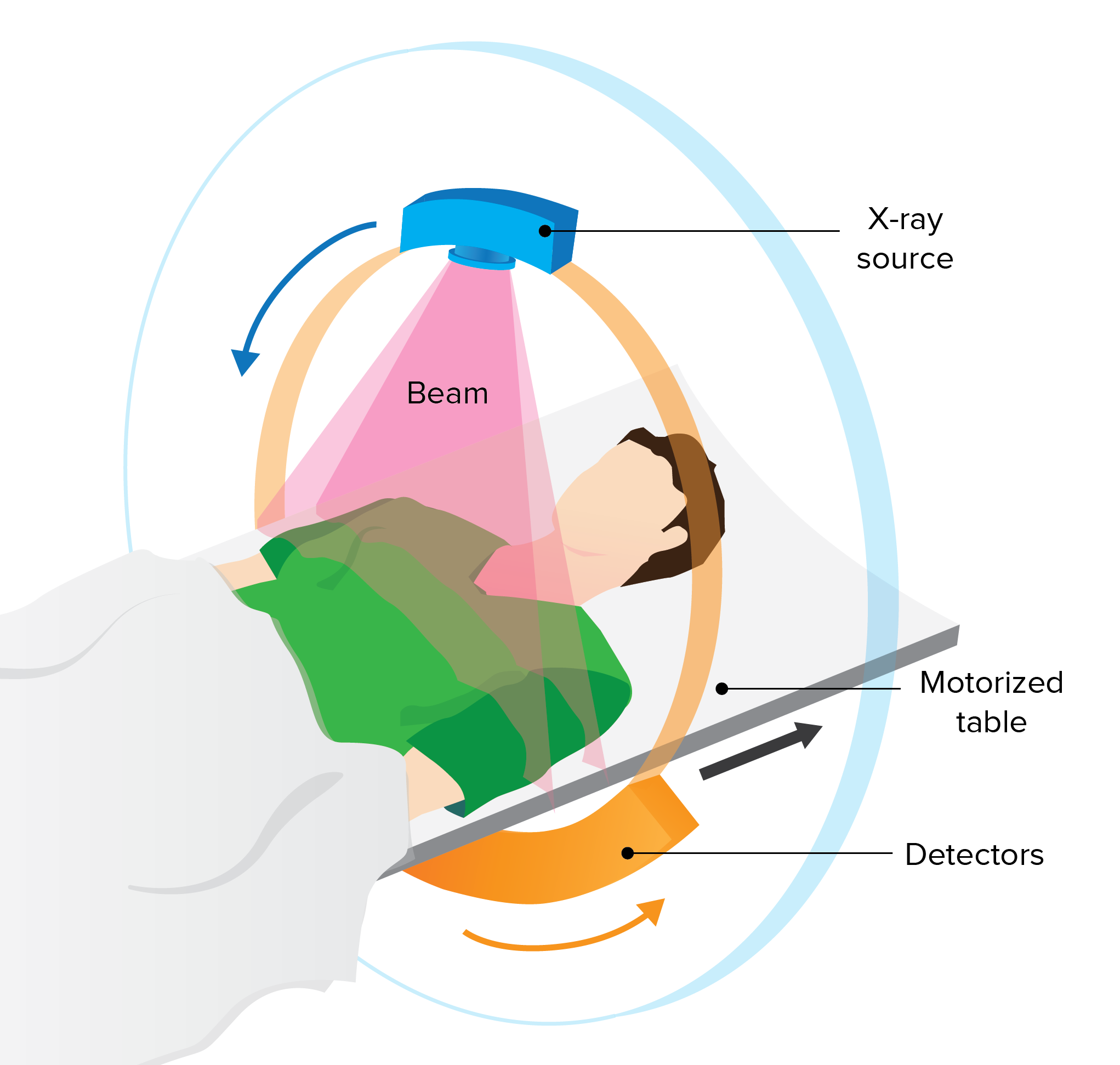
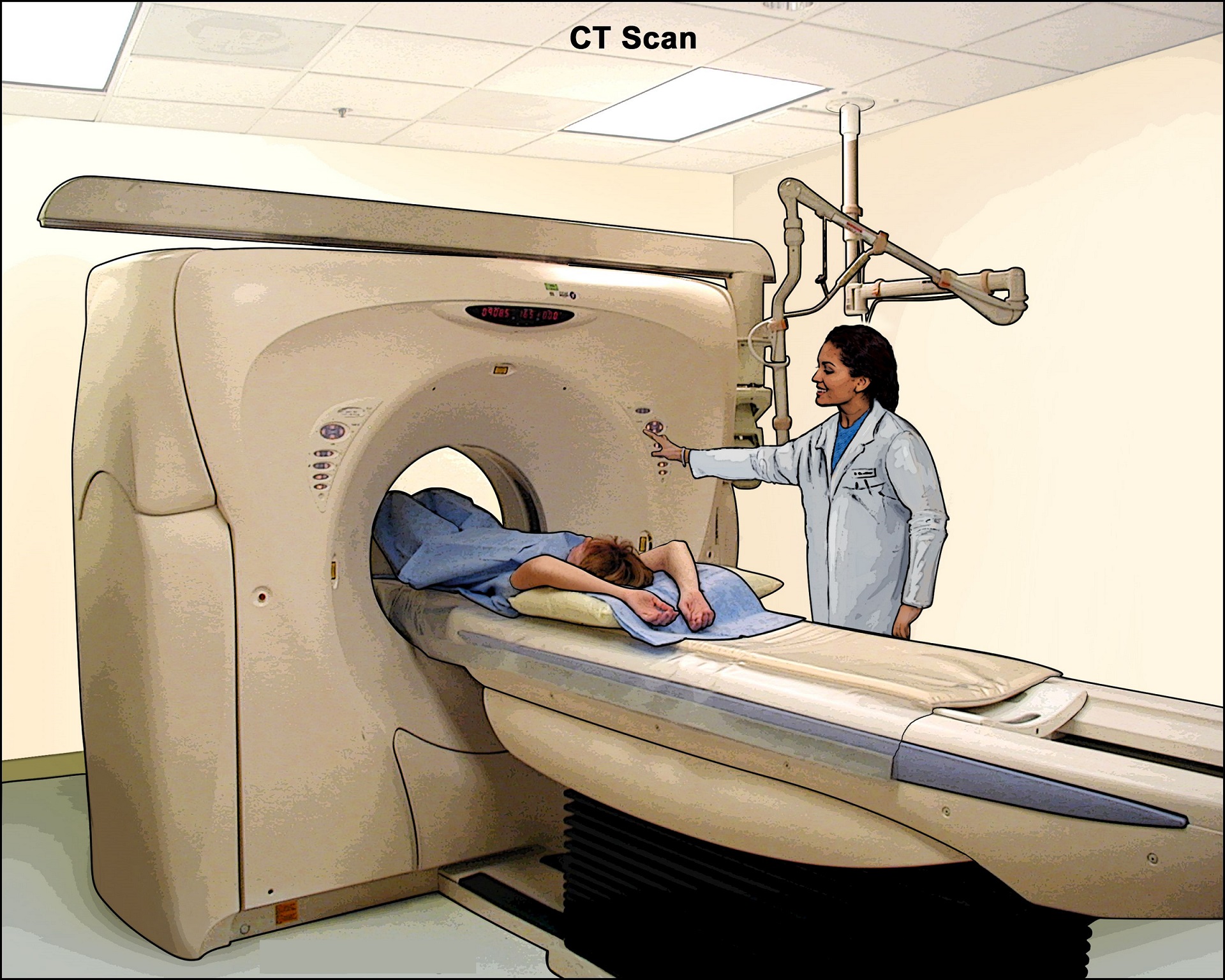
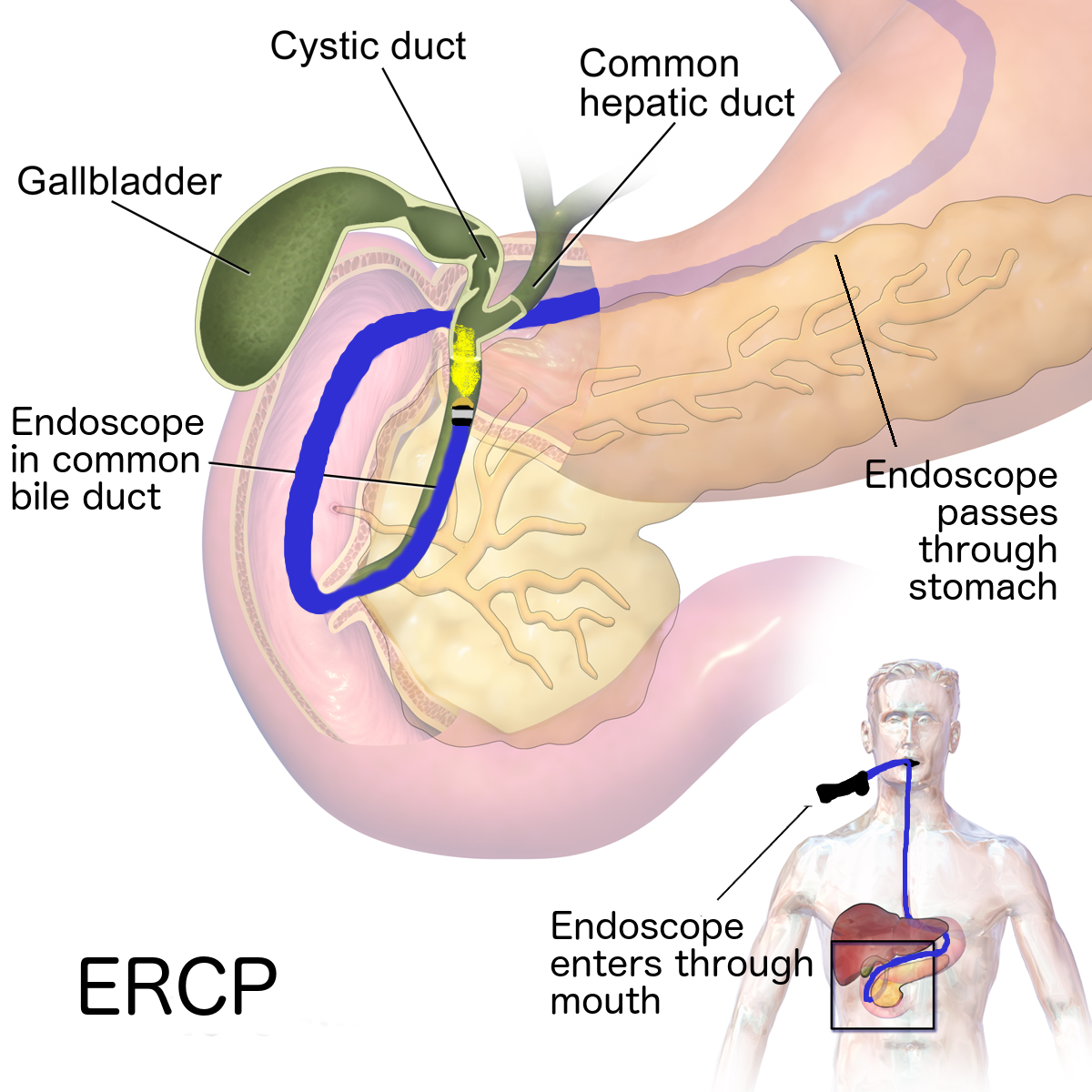
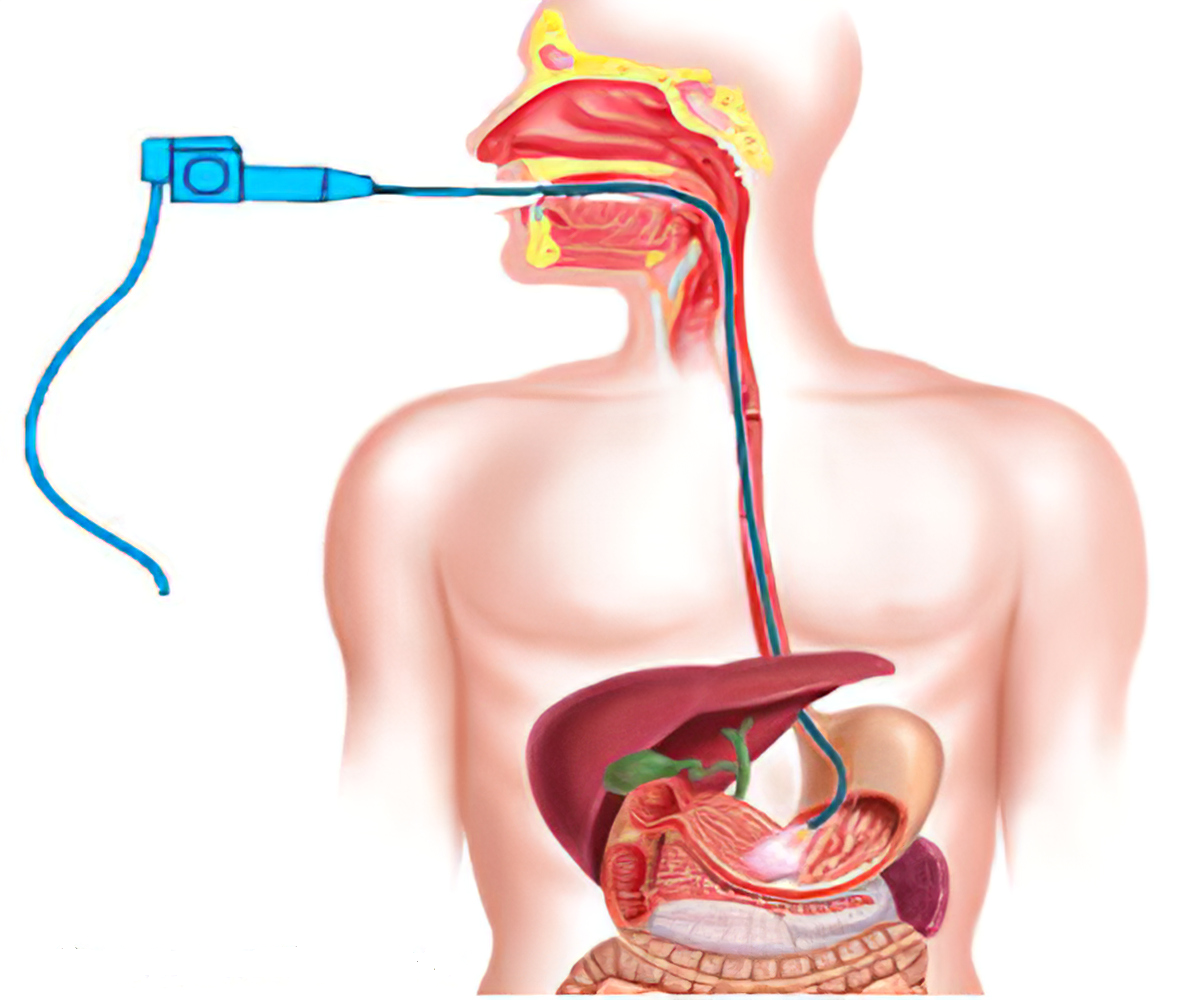
Initially, CT scan and endoscopy for diagnosis are done. Then after finding its occurrence, antifungal injections are given.
Surgical interventions may be needed to remove fungal balls from the affected organs. But the condition of the patient and concerned doctor’s analysis decide the course of treatment.
COVID and Mucormycosis
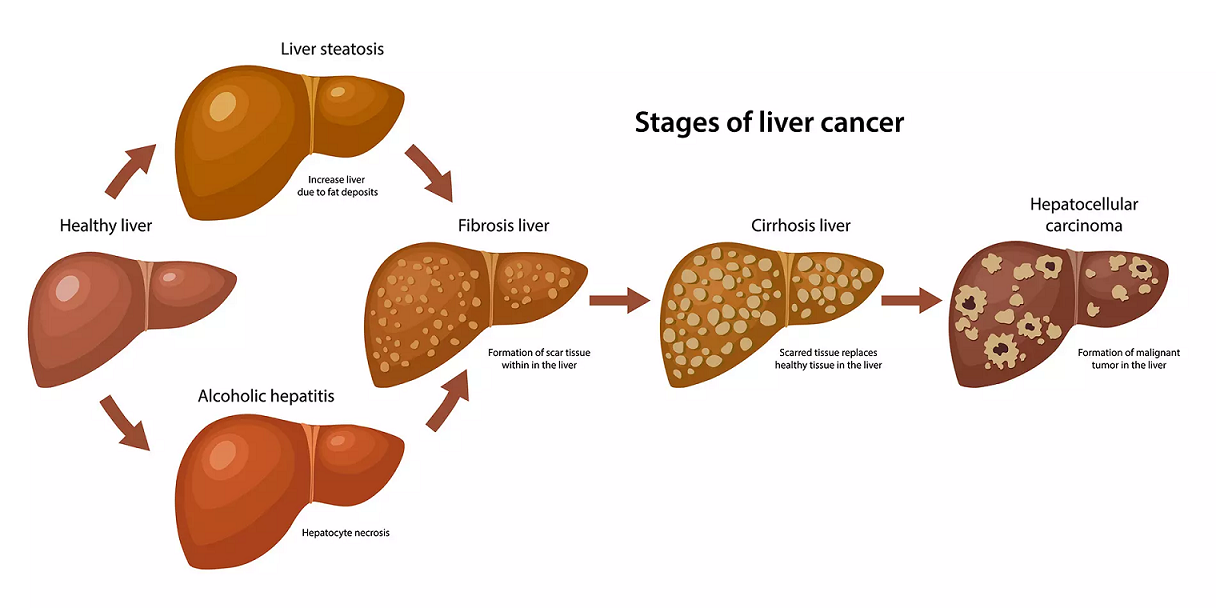
Considering the severity, it is not wise to put mucormycosis among other general fungal infections. Being a rare but severe fungal infection, mucormycosis generally occurs in highly immunity-compromised patients like cancer patients, patients with severe diabetes or those who underwent multiple organ surgeries or have had a complicated surgery.
Since it is now showing in several COVID patients post-recovery, it reflects how COVID infection affects our immune system on a deeper level. It calls for serious attention as people now need more to be health-conscious and work on their overall well-being.
How can I lower the risk of mucormycosis?
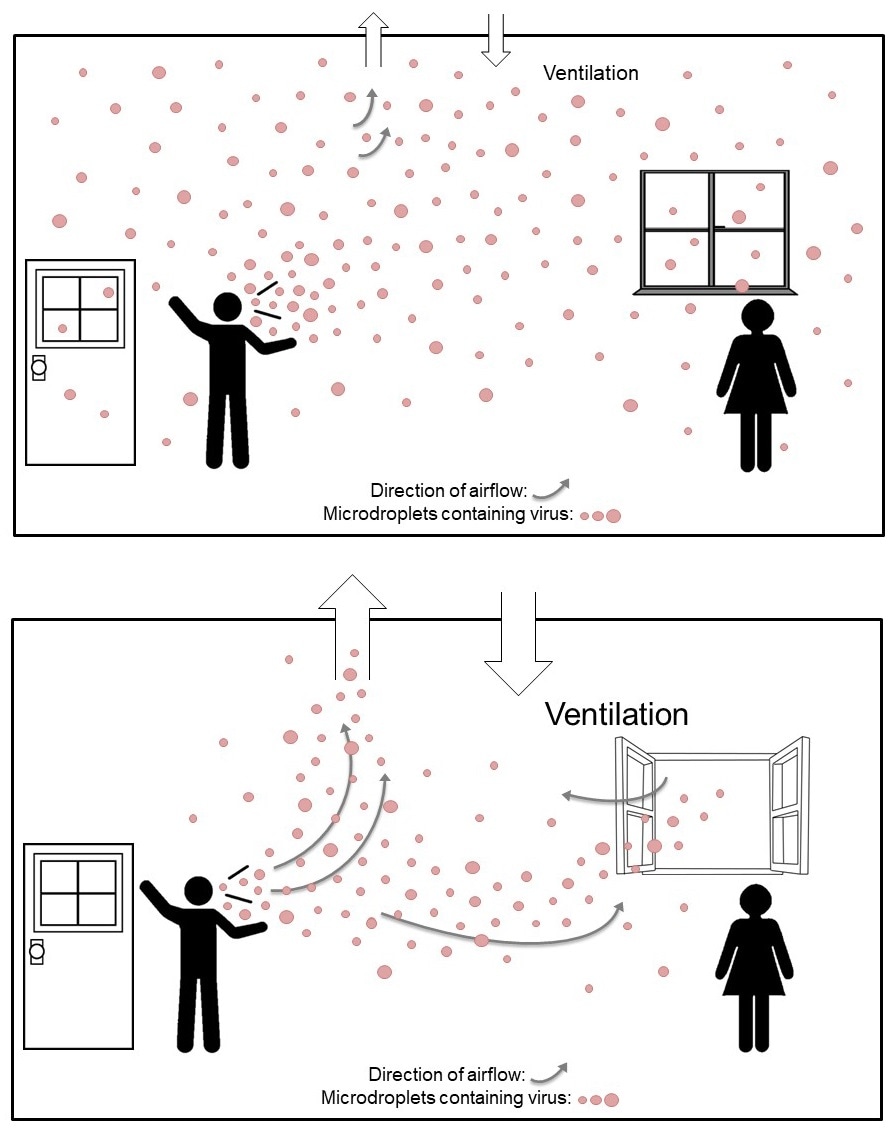
It’s difficult to avoid breathing in fungal spores because the fungi that cause mucormycosis are common in the environment.
There is no vaccine to prevent mucormycosis.
For people who have weakened immune systems, there may be some ways to lower the chances of developing mucormycosis.
- Protect yourself from the environment. It’s important to note that although these actions are recommended, they haven’t been proven to prevent mucormycosis.
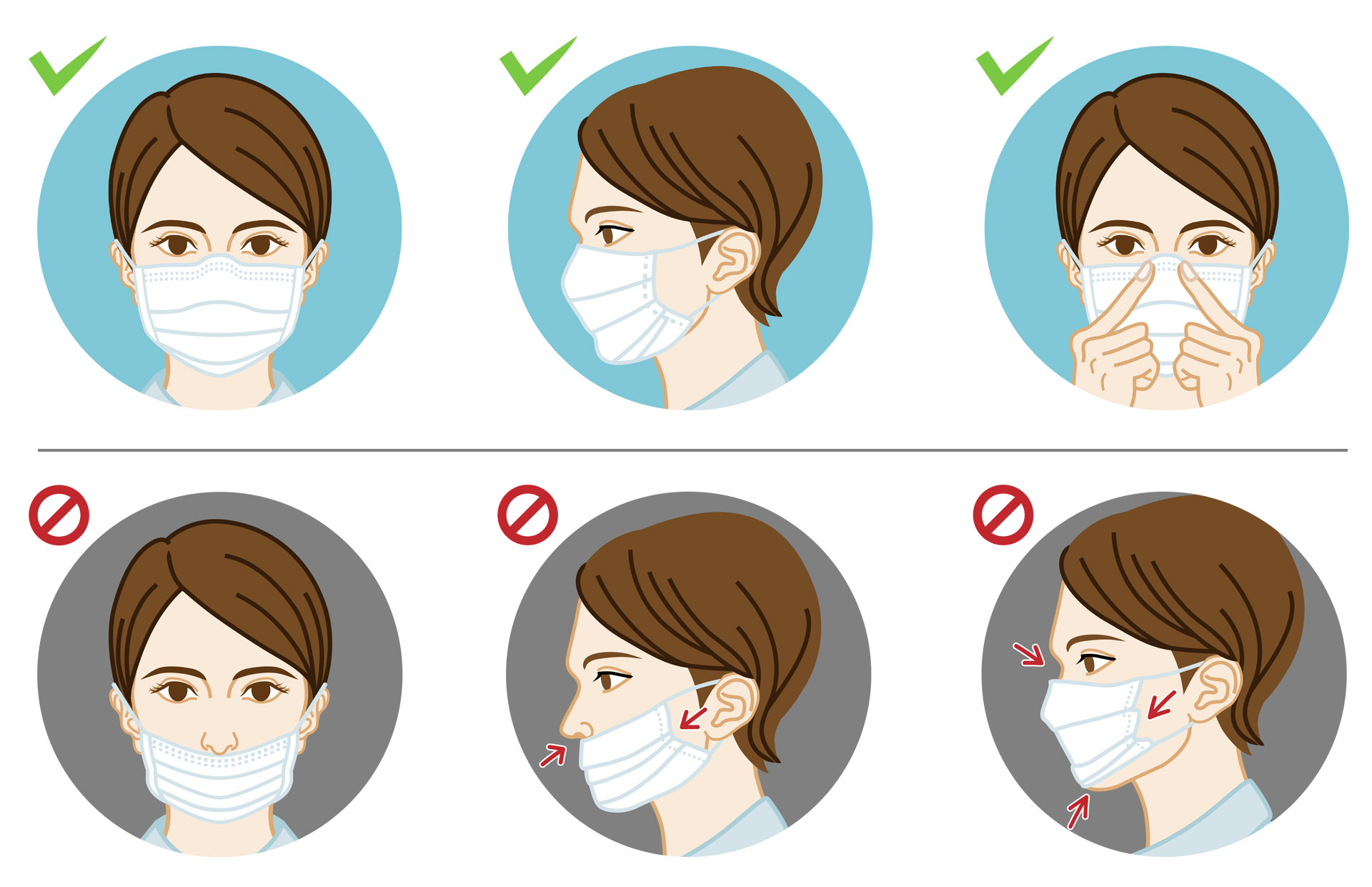
- Try to avoid areas with a lot of dust like construction or excavation sites. If you can’t avoid these areas, wear an N95 respirator (a type of face mask) while you’re there.
- Avoid direct contact with water-damaged buildings and flood water after hurricanes and natural disasters.
- Avoid activities that involve close contact to soil or dust, such as yard work or gardening. If this isn’t possible,
- Wear shoes, long pants, and a long-sleeved shirt when doing outdoor activities such as gardening, yard work, or visiting wooded areas.
- Wear gloves when handling materials such as soil, moss, or manure.
- To reduce the chances of developing a skin infection, clean skin injuries well with soap and water, especially if they have been exposed to soil or dust.
Bottomline
Right information is the key.
After COVID infection, keep a positive approach towards life and follow the doctor’s suggestions. Even post-COVID, keep going for regular health check-ups. It will help in bringing immediate attention to diseases, if any, at their initial stage and get relevant treatment.
Reference
- https://www.cdc.gov/fungal/diseases/mucormycosis/risk-prevention.html
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7599039/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7394275/