Diabetes
Know more about Type 2 Diabetes: Life expectancy, Diabetes diet, prevention & complications
This article looks at the prevalence of type 2 diabetes, its causes and risk factors, and the life expectancy of those with the condition. It also covers ways to prevent diabetes.
Overview
What is Type 2 diabetes?
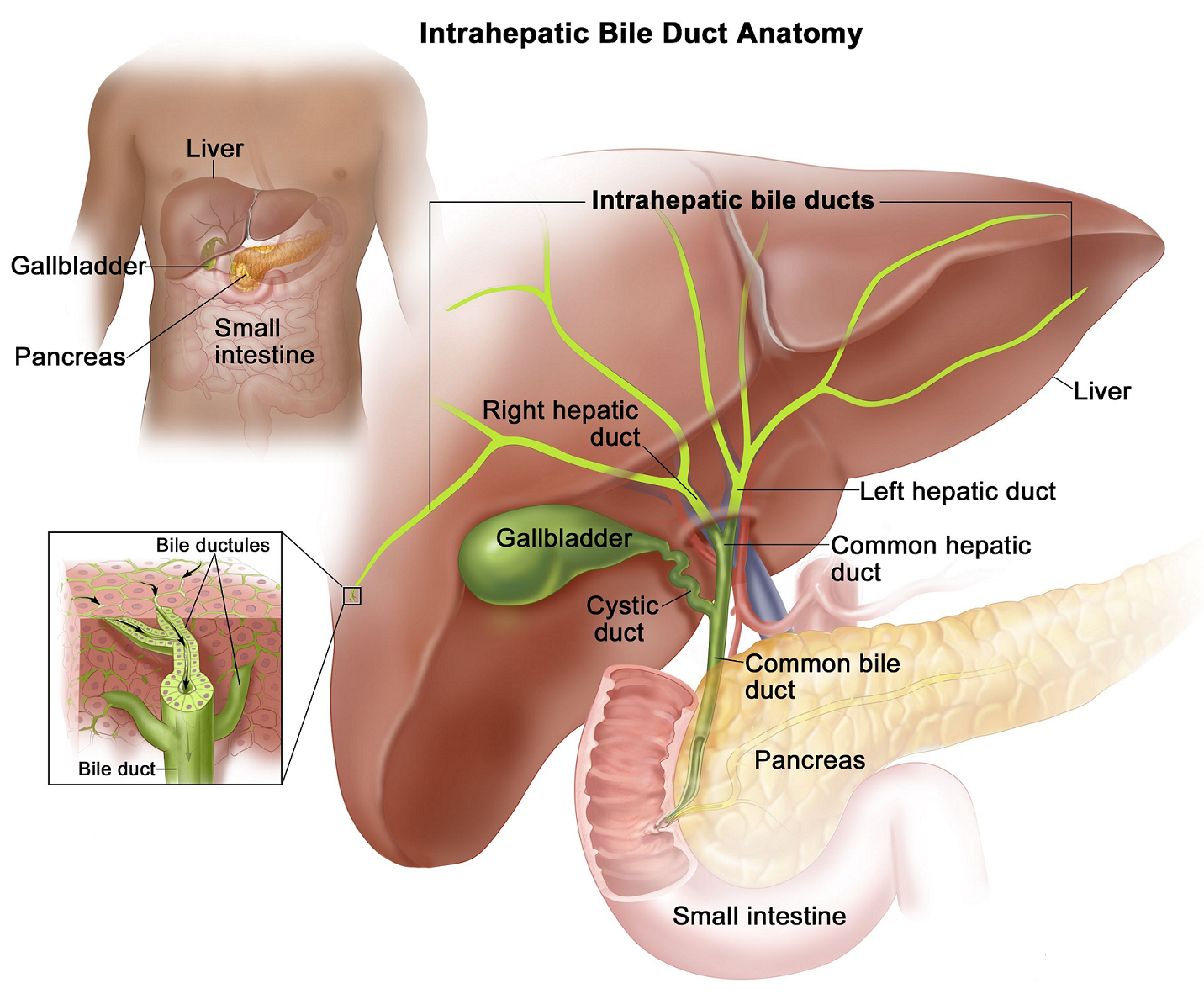
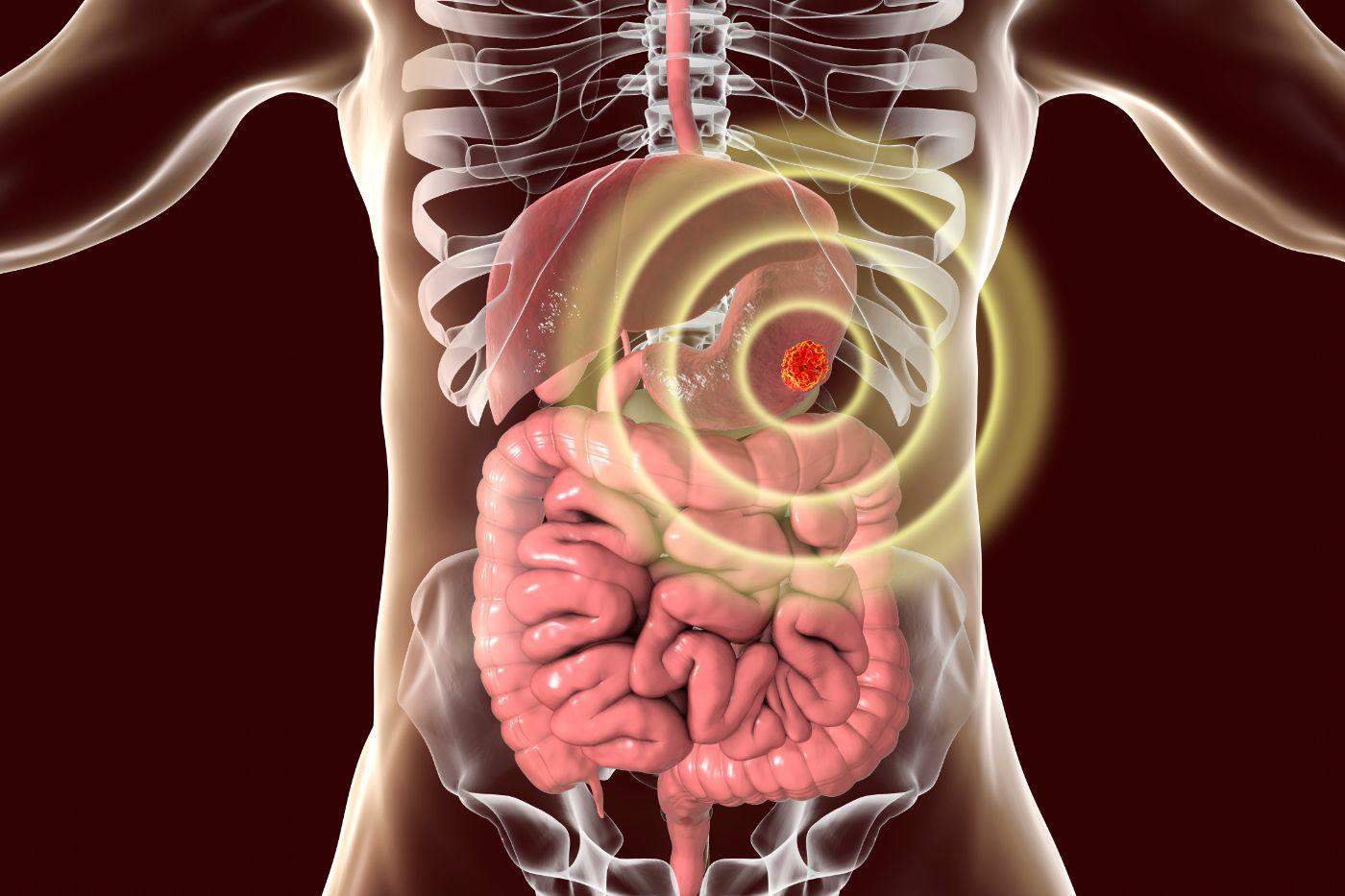
Type 2 diabetes is a disease where your body can’t use energy from food properly. Your pancreas produces insulin (a hormone) to help your cells use glucose (sugar). But over time your pancreas makes less insulin and the cells resist the insulin. This causes too much sugar to build up in your blood. High blood sugar levels from Type 2 diabetes can lead to serious health problems including heart disease, stroke or death.
Type 1 vs. Type 2 diabetes: What’s the difference?
Type 2 diabetes is not the same as Type 1 diabetes. In Type 1 diabetes, your pancreas doesn’t make any insulin. In Type 2, your pancreas doesn’t make enough insulin, and the insulin it is making doesn’t always work as it should. Both types are forms of diabetes mellitus, meaning they lead to hyperglycemia (high blood sugar).
Type 2 diabetes usually affects older adults, though it’s becoming more common in children. Type 1 diabetes usually develops in children or young adults, but people of any age can get it.
Prevalence of Type 2 Diabetes
The burden of diabetes mellitus is rising globally, and at a much faster rate in developed regions, such as Western Europe. The gender distribution is equal, and the incidence peaks at around 55 years of age. Global prevalence of type 2 diabetes is projected to increase to 7079 individuals per 100,000 by 2030, reflecting a continued rise across all regions of the world. There are concerning trends of rising prevalence in lower-income countries. Urgent public health and clinical preventive measures are warranted. (Source)
Life Expectancy: Factors that Influence Prognosis
Type 2 diabetes can greatly affect your health, but how long you can live with the condition depends on the timeliness of your diagnosis and treatment. Life expectancy is also affected by how well you manage your blood sugar levels and your ability to avoid factors that raise the risk of complications. These risk factors include smoking, lack of exercising, poor diet, and maintaining an unhealthy weight.
Research shows that on average type 2 diabetes is associated with a 1.3 to 2.0 times higher risk of early death, which is most often the result of cardiovascular disease.
Still, some factors contribute to a better outlook for people with diabetes. New medications and screening techniques have improved diagnostics and treatment, and a renewed emphasis on eating a balanced diet and maintaining a healthy weight can make a difference.
Age
The older you get, the greater your risk of type 2 diabetes- regardless of your genetics, weight, or eating habits. That's because the cells' ability to respond to insulin, called insulin sensitivity, decreases with age, especially after age 45.
When cells become more resistant to insulin (insulin resistance), it makes it harder for blood sugar to be effectively removed from the bloodstream, which causes blood sugar levels to rise excessively high.
Scientists theorize that the pancreas "ages" as well, losing its ability to pump insulin as efficiently as it did when we were younger.
Genetics
A diagnosis of diabetes is usually met with a ton of questions. Did I inherit this condition? Are my children at risk? Could I have prevented this, or was I genetically predisposed to get this all along?
The answers are complex, but research has shown that genetics play a role in type 2 diabetes. In fact, it is now believed that many people inherit a predisposition to the disease, but something in your environment triggers it. Genetics alone don't explain why one person develops type 2 diabetes and another does not.
Type 2 diabetes has a strong genetic component—more so than Type 1 diabetes—as indicated by twin studies that show that if one twin has the condition the other twin is three to four times as likely to get it. Similarly, family history seems to play a large role since obesity, which is significantly linked to diabetes, and diabetes itself are often seen in both parents and their children.
Diet
Your diet is one of the most important factors in maintaining healthy blood sugar levels and extending your life expectancy when you have type 2 diabetes.
Managing blood sugar can be difficult either because your pancreas isn't making enough insulin or the insulin it makes isn't being used efficiently. Learning what to eat and what not to eat, portion control, and how to meet your dietary needs are paramount to leading a healthy, symptom-free life.
There are some diets, sometimes called “diabetic diets” that have been proven to keep blood sugars within a healthy range. These diets all encourage high fibre intake, little or no added sugar, complex carbs, and avoidance of foods high in trans and saturated fats. The goal is to provide you with the macronutrients you need while cutting the simple carbs that lead to spikes in blood sugar.
While there's no one-size-fits-all diabetic diet, it's important to note that there are some well-studied meal plans that have been shown to lower your risk of medical complications as a result of type 2 diabetes. These meal plans include:
- The Mediterranean diet: This diet has been shown to improve fasting glucose and A1C levels (which are used to monitor diabetes) for those with type 2 diabetes. It emphasizes eating vegetables, minimally processed foods, a moderate amount of fish, poultry, and eggs, and little dairy or red meat (once a week approximately).
- Dietary Approaches to Stop Hypertension (DASH) diet: In addition to promoting blood pressure control, this low-fat, low-sodium eating pattern has been shown to improve insulin resistance and hyperlipidemia (too many fats in the blood). It also promotes weight loss. But at its extreme, this diet can promote too many carbs and not enough healthy fats so you may want to consult with a specialist to formulate a plan that works best for you.
- Paleo: Paleo mimics the way earliest humans ate, cutting out all sugar, dairy, and processed foods. Paleo diets are generally low in carbohydrates; therefore, they are effective at improving glycemic control.
- Vegetarian or plant-based diets. Vegetarian and vegan diets have been shown to lessen insulin resistance in those with type 2 diabetes but only if you're mindful of your carbohydrate intake. Carb consumption tends to go up when replacing meat or dairy (two major sources of protein), but emphasizing high-fibre legumes (beans), nuts, and healthy plant-based fat sources like avocado can help you avoid this pitfall.
Prevention
Healthy lifestyle choices can help prevent type 2 diabetes, and that's true even if you have biological relatives living with diabetes. If you've received a diagnosis of prediabetes, lifestyle changes may slow or stop the progression to diabetes.
A healthy lifestyle includes:
- Eating healthy foods. Choose foods lower in fat and calories and higher in fiber. Focus on fruits, vegetables and whole grains.
- Getting active. Aim for 150 or more minutes a week of moderate to vigorous aerobic activity, such as a brisk walk, bicycling, running or swimming.
- Losing weight. Losing a modest amount of weight and keeping it off can delay the progression from prediabetes to type 2 diabetes. If you have prediabetes, losing 7% to 10% of your body weight can reduce the risk of diabetes.
- Avoiding inactivity for long periods. Sitting still for long periods can increase your risk of type 2 diabetes. Try to get up every 30 minutes and move around for at least a few minutes.
For people with prediabetes, metformin (Fortamet, Glumetza, others), an oral diabetes medication, may be prescribed to reduce the risk of type 2 diabetes. This is usually prescribed for older adults who are obese and unable to lower blood sugar levels with lifestyle changes.
Comorbid Conditions
Obesity is often associated with and first thought of when many people think of type 2 diabetes, but hypertension, heart disease, hyperlipidemia, obstructive sleep apnea, and chronic kidney disease are also conditions that can be caused or made worse by diabetes.
Risk factors for many of these conditions overlap with risk factors for diabetes. Thus, lifestyle changes and other treatments that help you manage or prevent diabetes can also lower the chances you'll have problems from these comorbidities.
When to Talk to Your Healthcare Provider
If you have certain risk factors, like excess belly fat or a sedentary lifestyle, you may want to work with your healthcare provider to assess your diabetes risk.
Type 2 diabetes is a manageable condition, but early detection and treatment under the care of a trusted medical professional are key. With the help of a diabetes care team, you can formulate a plan with reachable goals and figure out the best course of action moving forward.
Summary
While there's no one cause of type 2 diabetes, it's largely thought of as a lifestyle disease. Avoiding the following habits can reduce your risk of developing type 2 diabetes.
- Poor diet
- Obesity
- Sedentary lifestyle
- Smoking and frequent alcohol use
If you are diagnosed with type 2 diabetes, it's important to manage your blood sugar levels by eating a healthy, low-sugar diet, exercising regularly, and losing weight. These strategies can help you avoid health complications from diabetes.
Reference
- https://www.who.int/news-room/fact-sheets/detail/diabetes
- https://www.mayoclinic.org/diseases-conditions/type-2-diabetes/symptoms-causes/syc-20351193
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3977406/
- https://my.clevelandclinic.org/health/diseases/21501-type-2-diabetes
- https://www.cdc.gov/diabetes/basics/type2.html
- https://pubmed.ncbi.nlm.nih.gov/32175717/